Chapter 34 TRICHOTHECENE MYCOTOXINS
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Biological Toxins As the Potential Tools for Bioterrorism
International Journal of Molecular Sciences Review Biological Toxins as the Potential Tools for Bioterrorism Edyta Janik 1, Michal Ceremuga 2, Joanna Saluk-Bijak 1 and Michal Bijak 1,* 1 Department of General Biochemistry, Faculty of Biology and Environmental Protection, University of Lodz, Pomorska 141/143, 90-236 Lodz, Poland; [email protected] (E.J.); [email protected] (J.S.-B.) 2 CBRN Reconnaissance and Decontamination Department, Military Institute of Chemistry and Radiometry, Antoniego Chrusciela “Montera” 105, 00-910 Warsaw, Poland; [email protected] * Correspondence: [email protected] or [email protected]; Tel.: +48-(0)426354336 Received: 3 February 2019; Accepted: 3 March 2019; Published: 8 March 2019 Abstract: Biological toxins are a heterogeneous group produced by living organisms. One dictionary defines them as “Chemicals produced by living organisms that have toxic properties for another organism”. Toxins are very attractive to terrorists for use in acts of bioterrorism. The first reason is that many biological toxins can be obtained very easily. Simple bacterial culturing systems and extraction equipment dedicated to plant toxins are cheap and easily available, and can even be constructed at home. Many toxins affect the nervous systems of mammals by interfering with the transmission of nerve impulses, which gives them their high potential in bioterrorist attacks. Others are responsible for blockage of main cellular metabolism, causing cellular death. Moreover, most toxins act very quickly and are lethal in low doses (LD50 < 25 mg/kg), which are very often lower than chemical warfare agents. For these reasons we decided to prepare this review paper which main aim is to present the high potential of biological toxins as factors of bioterrorism describing the general characteristics, mechanisms of action and treatment of most potent biological toxins. -

Medical Management of Biological Casualties Handbook
USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 U.S. ARMY MEDICAL RESEARCH INSTITUTE OF INFECTIOUS DISEASES FORT DETRICK FREDERICK, MARYLAND Emergency Response Numbers National Response Center: 1-800-424-8802 or (for chem/bio hazards & terrorist events) 1-202-267-2675 National Domestic Preparedness Office: 1-202-324-9025 (for civilian use) Domestic Preparedness Chem/Bio Helpline: 1-410-436-4484 or (Edgewood Ops Center – for military use) DSN 584-4484 USAMRIID’s Emergency Response Line: 1-888-872-7443 CDC'S Emergency Response Line: 1-770-488-7100 Handbook Download Site An Adobe Acrobat Reader (pdf file) version of this handbook can be downloaded from the internet at the following url: http://www.usamriid.army.mil USAMRIID’s MEDICAL MANAGEMENT OF BIOLOGICAL CASUALTIES HANDBOOK Sixth Edition April 2005 Lead Editor Lt Col Jon B. Woods, MC, USAF Contributing Editors CAPT Robert G. Darling, MC, USN LTC Zygmunt F. Dembek, MS, USAR Lt Col Bridget K. Carr, MSC, USAF COL Ted J. Cieslak, MC, USA LCDR James V. Lawler, MC, USN MAJ Anthony C. Littrell, MC, USA LTC Mark G. Kortepeter, MC, USA LTC Nelson W. Rebert, MS, USA LTC Scott A. Stanek, MC, USA COL James W. Martin, MC, USA Comments and suggestions are appreciated and should be addressed to: Operational Medicine Department Attn: MCMR-UIM-O U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID) Fort Detrick, Maryland 21702-5011 PREFACE TO THE SIXTH EDITION The Medical Management of Biological Casualties Handbook, which has become affectionately known as the "Blue Book," has been enormously successful - far beyond our expectations. -

Realtime Laboratories Technical Brief the Importance of Testing for Macrocyclic Trichothecene Mycotoxins
RealTime Laboratories Technical Brief The Importance of Testing for Macrocyclic Trichothecene Mycotoxins REALTIME LABORATORIES, INC. 4100 Fairway Drive • Suite 600 • Carrollton, Texas 75010 (972) 492-0419 • [email protected] • www.realtimelab.com There are over 50,000 different species of mold, but only about 200 species may present serious health risks to humans or animals. These species, referred to as toxic mold, are potentially hazardous because they produce toxins, known as Mycotoxins. The impact of these Mycotoxins on our health can be life threatening. Commonly Encountered Mycotoxin Producing Fungi Species Mycotoxin Aspergillus flavus Aflatoxin (AT) Aspergillus parasiticus AT Aspergillus ochraceus Ochratoxin A (OTA) Aspergillus niger OTA Penicillium verrucosum OTA Penicillium nordicum OTA Penicillium chrysogenum OTA Stachybotrys chartarum Macrocyclic Trichothecenes (e.g. Roridin, Satratoxin, Verrucarin) Aspergillus versicolor Sterigmatocystin Aspergillus fumigatus Gliotoxin Chaetomium globosum Chaetoglobsin A, C Fusarium sp. Simple Trichothecenes (e.g. T-2, Fumonison, DON ) Macrocyclic Trichothecene- Satrotoxin H Simple Trichothecene- T-2 The Real Time Lab Mycotoxin Test Panel determines the presence of the following Mycotoxins RTL’s 15 Mycotoxin Testing Panel 1. Ochratoxins • Ochratoxin A 2. Aflatoxins • Aflatoxin B1 • Aflatoxin B2 • Aflatoxin G1 • Aflatoxin G2 3. Macrocyclic Trichothecenes • Satratoxin G • Satratoxin H • Isosatratoxin F • Roridin A • Roridin E • Roridin H • Roridin L-2 (Biosynthetic derivative of Roridin) • Verrucarin A • Verrucarin J 4. Gliotoxin It is important to note: All of the Trichothecenes in the RTL panel are Macrocyclic Trichothecenes. When testing patients for Trichothecenes, it is critical that the test is for Macrocyclic Trichothecenes and not simple Trichothecenes such as T-2, DON or Fumonisin. Why is this so important? 1. -

Trichothecenes in Food and Feed, Relevance to Human and Animal Health and Methods of Detection: a Systematic Review
molecules Review Trichothecenes in Food and Feed, Relevance to Human and Animal Health and Methods of Detection: A Systematic Review Magdalena Polak-Sliwi´ ´nska* and Beata Paszczyk Faculty of Food Sciences, University of Warmia and Mazury in Olsztyn, Plac Cieszy´nski1, 10-726 Olsztyn, Poland; [email protected] * Correspondence: [email protected]; Tel.: +48-89-523-45-84 Abstract: Trichothecene mycotoxins are sesquiterpenoid compounds primarily produced by fungi in taxonomical genera such as Fusarium, Myrothecium, Stachybotrys, Trichothecium, and others, under specific climatic conditions on a worldwide basis. Fusarium mold is a major plant pathogen and produces a number of trichothecene mycotoxins including deoxynivalenol (or vomitoxin), nivalenol, diacetoxyscirpenol, and T-2 toxin, HT-2 toxin. Monogastrics are sensitive to vomitoxin, while poultry and ruminants appear to be less sensitive to some trichothecenes through microbial metabolism of trichothecenes in the gastrointestinal tract. Trichothecene mycotoxins occur worldwide however both total concentrations and the particular mix of toxins present vary with environmental condi- tions. Proper agricultural practices such as avoiding late harvests, removing overwintered stubble from fields, and avoiding a corn/wheat rotation that favors Fusarium growth in residue can reduce trichothecene contamination of grains. Due to the vague nature of toxic effects attributed to low concentrations of trichothecenes, a solid link between low level exposure and a specific trichothecene is difficult to establish. Multiple factors, such as nutrition, management, and environmental con- ditions impact animal health and need to be evaluated with the knowledge of the mycotoxin and concentrations known to cause adverse health effects. Future research evaluating the impact of low-level exposure on livestock may clarify the potential impact on immunity. -
Ketabton.Com (C) Ketabton.Com: the Digital Library
Ketabton.com (c) ketabton.com: The Digital Library ټوکسيکولوژي اثـــر: Hans Marquardt Siegfried G. Schafer Roger O. McClellan Frank Welsch ژباړن: عبدالکريم توتاخېل ۴۹۳۱ل کال (c) ketabton.com: The Digital Library د کتاب نوم: ټوکسيکولوژي ژباړن: عبدالکريم توتاخېل خـپرونـدی: د افغانستان ملي تحريک، فرهنګي څانګه وېــبپـاڼـه: www.melitahrik.com ډيـزايـنګر: ضياء ساپی پښتۍ ډيزاين: فياض حميد چــاپشمېـر: ۰۱۱۱ ټوکه چــاپـکـــال: ۰۹۳۱ ل کال/ ۵۱۰۲م د تحريک د خپرونو لړ: )۱۰( (c) ketabton.com: The Digital Library فهرست عنوان مخ مخکنۍ خبرې...................................................................................................الف د ژباړن سريزه.........................................................................................................ب لمړی فصل )کیمیاوي او بیولوژيکی عاملین(..............................................1 کیمیاوي عاملین ..............................................................................................1 بیولوژيکي عاملین ......................................................................................۲۶ دويم فصل )طبعي مرکبات(..........................................................................۵۸ پېژندنه ..............................................................................................................۵۸ د حیواناتو زهر)وينوم( او وينوم ..................................................................۵۲ د پروتوزوا او الجیانو توکسینونه...............................................................1۶۱ مايکوتوکسینونه .............................................................................................1۱۱ -

Toxic Effects of Mycotoxins in Humans M
Research Toxic effects of mycotoxins in humans M. Peraica,1 B. RadicÂ,2 A. LucicÂ,3 & M. Pavlovic 4 Mycotoxicoses are diseases caused by mycotoxins, i.e. secondary metabolites of moulds. Although they occur more frequently in areas with a hot and humid climate, favourable for the growth of moulds, they can also be found in temperate zones. Exposure to mycotoxins is mostly by ingestion, but also occurs by the dermal and inhalation routes. Mycotoxicoses often remain unrecognized by medical professionals, except when large numbers of people are involved. The present article reviews outbreaks of mycotoxicoses where the mycotoxic etiology of the disease is supported by mycotoxin analysis or identification of mycotoxin-producing fungi. Epidemiological, clinical and histological findings (when available) in outbreaks of mycotoxicoses resulting from exposure to aflatoxins, ergot, trichothecenes, ochratoxins, 3-nitropropionic acid, zearalenone and fumonisins are discussed. Voir page 763 le reÂsume en francËais. En la pa gina 763 figura un resumen en espanÄ ol. Introduction baking of bread made with ergot-contaminated wheat, as well as to other ergot toxins and Mycotoxins are secondary metabolites of moulds that hallucinogens, as well as belladonna alkaloids from exert toxic effects on animals and humans. The toxic mandragora apple, which was used to treat ergotism effect of mycotoxins on animal and human health is (3). While ergotism no longer has such important referred to as mycotoxicosis, the severity of which implications for public health, recent reports indicate depends on the toxicity of the mycotoxin, the extent that outbreaks of human mycotoxicoses are still of exposure, age and nutritional status of the possible (4). -

Military Potential of Biological Toxins
journal of applied biomedicine 12 (2014) 63–77 Available online at www.sciencedirect.com ScienceDirect journal homepage: http://www.elsevier.com/locate/jab Review Article Military potential of biological toxins Xiujuan Zhang a, Kamil Kuča b,c,**, Vlastimil Dohnal c, Lucie Dohnalová d, Qinghua Wu e, Chu Wu a,* a College of Horticulture and Garden, Yangtze University, Jingzhou, Hubei 434023, People's Republic of China b Biomedical Research Center, University Hospital Hradec Kralove, Czech Republic c Department of Chemistry, Faculty of Science, University of Hradec Kralove, Hradec Kralove, Rokitanskeho 62, 500 03, Czech Republic d Department of Hygiene, Faculty of Military Health, University of Defence, Hradec Kralove, Czech Republic e National Reference Laboratory of Veterinary Drug Residues (HZAU), Huazhong Agricultural University, Wuhan, Hubei 430070, People's Republic of China article info abstract Article history: Toxins are produced by bacteria, plants and animals for defense or for predation. Most of the Received 27 November 2013 toxins specifically affect the mammalian nervous system by interfering with the transmission Received in revised form of nerve impulses, and such toxins have the potential for misuse by the military or terrorist 17 February 2014 organizations. This review discusses the origin, structure, toxicity and symptoms, transmis- Accepted 19 February 2014 sion, mechanism(s) of action, symptomatic treatment of the most important toxins and Available online 1 March 2014 venoms derived from fungi, plants, marine animals, and microorganisms, along with their potential for use in bioweapons and/or biocrime. Fungal trichothecenes and aflatoxins are Keywords: potent inhibitors of protein synthesis in most eukaryotes and have been used as biological Military toxins warfare agents. -

Chronic Illness Associated with Mold and Mycotoxins: Is Naso-Sinus Fungal Biofilm the Culprit?
Toxins 2014, 6, 66-80; doi:10.3390/toxins6010066 OPEN ACCESS toxins ISSN 2072-6651 www.mdpi.com/journal/toxins Article Chronic Illness Associated with Mold and Mycotoxins: Is Naso-Sinus Fungal Biofilm the Culprit? Joseph H. Brewer 1,*, Jack D. Thrasher 2 and Dennis Hooper 3 1 Plaza Infectious Disease and St. Luke’s Hospital, 4320 Wornall Road, Suite 440, Kansas City, MO 64111, USA 2 Citrus Heights, CA 95610, USA; E-Mail: [email protected] 3 RealTime Laboratories, Carrollton, TX 75010, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +1-816-531-1550; Fax: +1-816-531-8277. Received: 2 December 2013; in revised form: 16 December 2013 / Accepted: 17 December 2013 / Published: 24 December 2013 Abstract: It has recently been demonstrated that patients who develop chronic illness after prior exposure to water damaged buildings (WDB) and mold have the presence of mycotoxins, which can be detected in the urine. We hypothesized that the mold may be harbored internally and continue to release and/or produce mycotoxins which contribute to ongoing chronic illness. The sinuses are the most likely candidate as a site for the internal mold and mycotoxin production. In this paper, we review the literature supporting this concept. Keywords: mycotoxin; biofilm; rhinosinusitis; chronic fatigue syndrome 1. Introduction Exposure to water damaged buildings (WDB) have been associated with numerous health problems that include fungal sinusitis, abnormalities in T and B cells, central and peripheral neuropathy, asthma, sarcoidosis, respiratory infections and chronic fatigue [1–14]. It has been well established that mold and mycotoxins are important constituents of the milieu in WDB that can lead to illness [15–22]. -
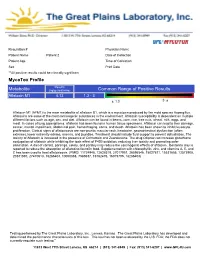
Metabolite Common Range of Positive Results Mycotox Profile
Patient Name: Debbe Krause Requisition #: 504797 Requisition # Physician Name Patient Name Patient 2 Date of Collection Patient Age Time of Collection Sex Print Date **All positive results could be clinically significant MycoTox Profile Results Metabolite (ng/g creatinine) Common Range of Positive Results Aflatoxin M1 4.13 1.3 - 3 Aflatoxin M1 (AFM1) is the main metabolite of aflatoxin B1, which is a mycotoxin produced by the mold species Aspergillus. Aflatoxins are some of the most carcinogenic substances in the environment. Aflatoxin susceptibility is dependent on multiple different factors such as age, sex, and diet. Aflatoxin can be found in beans, corn, rice, tree nuts, wheat, milk, eggs, and meat. In cases of lung aspergilloma, aflatoxin has been found in human tissue specimens. Aflatoxin can lead to liver damage, cancer, mental impairment, abdominal pain, hemorrhaging, coma, and death. Aflatoxin has been shown to inhibit leucocyte proliferation. Clinical signs of aflatoxicosis are non-pruritic macular rash, headache, gastrointestinal dysfunction (often extreme), lower extremity edema, anemia, and jaundice. Treatment should include fluid support to prevent dehydration. The toxicity of Aflotoxin is increased in the presence of Ochratoxin and Zearalenone. The drug Oltipraz can increase glutathione conjugation of aflatoxin while inhibiting the toxic effect of P450 oxidation, reducing liver toxicity and promoting safer elimination. A diet of carrots, parsnips, celery, and parsley may reduce the carcinogenic effects of aflatoxin . Bentonite clay is reported to reduce the absorption of aflatoxins found in food. Supplementation with chlorophyllin, zinc, and vitamins A, E, and C has been used to treat aflatoxicosis. (PMID: 11724948, 12628519, 27017951, 26596546, 15027811, 15531656, 12573908, 20381597, 27470613, 18286403, 10050868, 7585637, 16762476, 16019795, 18286403) Testing performed by The Great Plains Laboratory, Inc., Lenexa, Kansas. -

Urinary Mycotoxins
Internal medicine review Urinary Mycotoxins: A Review of Contaminated Buildings and Food in Search of a Biomarker Separating Sick Patients from Controls October 2019 Urinary Mycotoxins: A Review of Contaminated Buildings and Food in Search of a Biomarker Separating Sick Patients from Controls Author Abstract: Ritchie C. Shoemaker MD Beginning in 2010, there have been an increasing number of patients Center for Research on Biotoxin with a chronic multisystem illness who have been using measurements Associated Illnesses, Pocomoke, of mycotoxins in urine to diagnose a putative illness for which Md antifungals in various forms (oral, IV, sublingual and intranasal) are being used as therapy. Many of these patients and providers believe David Lark B.App.Sci; CIEC; that the illness is caused by fungi living in the human body, making CMC toxins, or has been acquired by exposure to the interior of water- EnviroBiomics, Inc., San damaged buildings (WDB). This practice persists despite the absence Antonio, Tx, USA & of (i) an accepted case definition; (ii) any validated control groups; (iii) MouldLab, Newcastle, NSW any rigorous case/control studies; (iv) any prospective, placebo- Australia controlled studies; (v) any confirmation of active fungal infection; (vi) any confirmation that urinary mycotoxins are not simply derived from Correspondence diet; and presence (vii) of a sharp repudiation from the CDC of this Ritchie C. Shoemaker practice and the use of antifungals in 2015; and presence (viii) of a [email protected] robust literature -

Substrate Specificities and Synthesis of Type a and B Trichothecen
toxins Article UDP-Glucosyltransferases from Rice, Brachypodium, and Barley: Substrate Specificities and Synthesis of Type A and B Trichothecene-3-O-β-D-glucosides Herbert Michlmayr 1,2,* ID , Elisabeth Varga 3 ID , Alexandra Malachová 3, Philipp Fruhmann 4,5 ID , Marta Pi ˛atkowska 3, Christian Hametner 4, Jana Šofrová 3,6, Günther Jaunecker 7, Georg Häubl 7, Marc Lemmens 8, Franz Berthiller 3 ID and Gerhard Adam 1 ID 1 Department of Applied Genetics and Cell Biology, University of Natural Resources and Life Sciences, Vienna, (BOKU), Konrad Lorenz Str. 24, 3430 Tulln, Austria; [email protected] 2 Department of Food Chemistry and Toxicology, University of Vienna, Währinger Str. 38, 1090 Vienna, Austria 3 Christian Doppler Laboratory for Mycotoxin Metabolism and Center for Analytical Chemistry, Department of Agrobiotechnology (IFA-Tulln), BOKU, Konrad Lorenz Str. 20, 3430 Tulln, Austria; [email protected] (E.V.); [email protected] (A.M.); [email protected] (M.P.); [email protected] (J.Š.); [email protected] (F.B.) 4 Institute of Applied Synthetic Chemistry, Vienna University of Technology, Getreidemarkt 9/163, 1060 Vienna, Austria; [email protected] (P.F.); [email protected] (C.H.) 5 CEST Kompetenzzentrum für elektrochemische Oberflächentechnologie GmbH, Viktor-Kaplan-Str. 2, 2700 Wiener Neustadt, Austria 6 Department of Chemistry and Biochemistry, Mendel University in Brno, Zemˇedˇelská 1, 613 00 Brno, Czech Republic 7 Romerlabs Division Holding GmbH, Technopark 1, 3430 Tulln, Austria; [email protected] (G.J.); [email protected] (G.H.) 8 Biotechnology in Plant Production, IFA-Tulln, BOKU, Konrad Lorenz Str. -

Advances in Deoxynivalenol Toxicity Mechanisms: the Brain As a Target
Toxins 2012, 4, 1120-1138; doi:10.3390/toxins4111120 OPEN ACCESS toxins ISSN 2072-6651 www.mdpi.com/journal/toxins Review Advances in Deoxynivalenol Toxicity Mechanisms: The Brain as a Target Marion S. Bonnet 1, Julien Roux 2, Lourdes Mounien 1, Michel Dallaporta 1 and Jean-Denis Troadec 1,* 1 Laboratory of Physiology and Pathophysiology of Somatomotor and Autonomic Nervous System, Faculty of Sciences and Technology, Escadrille Normandie-Niemen Avenue, Aix-Marseilles University, Marseilles 13397, France; E-Mails: [email protected] (M.S.B.); [email protected] (L.M.); [email protected] (M.D.) 2 Biomeostasis, Contract Research Organization, Faculty of Sciences and Technology, Escadrille Normandie-Niemen Avenue, Marseilles 13397, France; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel: +33-491-288-948; Fax: +33-491-288-885. Received: 18 September 2012; in revised form: 18 October 2012 / Accepted: 19 October 2012 / Published: 1 November 2012 Abstract: Deoxynivalenol (DON), mainly produced by Fusarium fungi, and also commonly called vomitoxin, is a trichothecene mycotoxin. It is one of the most abundant trichothecenes which contaminate cereals consumed by farm animals and humans. The extent of cereal contamination is strongly associated with rainfall and moisture at the time of flowering and with grain storage conditions. DON consumption may result in intoxication, the severity of which is dose-dependent and may lead to different symptoms including anorexia, vomiting, reduced weight gain, neuroendocrine changes, immunological effects, diarrhea, leukocytosis, hemorrhage or circulatory shock. During the last two decades, many studies have described DON toxicity using diverse animal species as a model.