Manual Therapy of the Upper and Lower Extremities Including High Velocity/ Low Amplitude Thrust Techniques
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4Th SESSION 1
2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4th SESSION 1: Carpal Ligament 1 Stable Central Column Theory of Carpal Mechanics Michael Sandow FRACS Wakefield Orthopaedic Clinic Adelaide, Australia Background: The carpus is a complicated and functionally challenged mechanical system and advancements in the understanding have been compromised by the recognition that there is no standard carpal mechanical system and no typical wrist. This paper cover component of a larger project that seeks to develop a kinetic model of wrist mechanics to allow reverse analysis of the specific biomechanical controls or rule of a specific patient's carpus, and then use those to create a forward mathematical model to reproduce the unique individual's anatomical motion based on the extracted rules. Objectives and Methods: Based on previous observations, the carpus essentially moves with only 2 degrees of freedom - pitch (flexion / extension) and yaw (radial deviation / ulnar deviation), while largely preventing roll (pronation / supination). The object of this paper is therefore to present the background and justification to support the rules based motion (RBM) concept states that the motion of a mechanical system, such as the wrist, is the net interplay of 4 rules - morphology, constraint, interaction and load. The Stable Central Column Theory (SCCT) of wrist mechanics applies the concept of RBM to the carpus, and by using a reverse engineering computational analysis model, identified a consistent pattern of isometric constraints, creating a "Two-Gear Four-Bar" linkage. This study assessed the motion of the carpus using a 3D dynamic visualization model, and the hypothesis was that the pattern and direction of motion of the proximal row, and the distal row with respect the immediately cephalad carpal bones or radius would be very similar in all directions of wrist motion. -

REVIEW ARTICLE Osteoarthritis of the Wrist
REVIEW ARTICLE Osteoarthritis of the Wrist Krista E. Weiss, Craig M. Rodner, MD From Harvard College, Cambridge, MA and Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Osteoarthritis of the wrist is one of the most common conditions encountered by hand surgeons. It may result from a nonunited or malunited fracture of the scaphoid or distal radius; disruption of the intercarpal, radiocarpal, radioulnar, or ulnocarpal ligaments; avascular necrosis of the carpus; or a developmental abnormality. Whatever the cause, subsequent abnormal joint loading produces a spectrum of symptoms, from mild swelling to considerable pain and limitations of motion as the involved joints degenerate. A meticulous clinical and radiographic evaluation is required so that the pain-generating articulation(s) can be identi- fied and eliminated. This article reviews common causes of wrist osteoarthritis and their surgical treatment alternatives. (J Hand Surg 2007;32A:725–746. Copyright © 2007 by the American Society for Surgery of the Hand.) Key words: Wrist, osteoarthritis, arthrodesis, carpectomy, SLAC. here are several different causes, both idio- of events is analogous to SLAC wrist and has pathic and traumatic, of wrist osteoarthritis. been termed scaphoid nonunion advanced collapse Untreated cases of idiopathic carpal avascular (SNAC). Wrist osteoarthritis can also occur second- T 1 2 necrosis, as in Kienböck’s or Preiser’s disease, may ary to an intra-articular fracture of the distal radius or result in radiocarpal arthritis. Congenital wrist abnor- ulna or from an extra-articular fracture resulting in malities, such as Madelung’s deformity,3,4 can lead malunion and abnormal joint loading. -
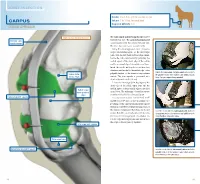
Carpus Volume: 7 to 10 Ml for Each Joint Degree of Difficulty: 1/3 Dorsal Approach
JOINT INJECTION needle: 1 to 1.5 in. (2.5 to 3.8 cm), 20 ga Carpus volume: 7 to 10 ml for each joint Degree of difficulty: 1/3 Dorsal approach right carpus, dorsomedial view The radiocarpal and intercarpal joints can be extensor carpi entered with ease. The carpometacarpal joint radialis tendon communicates with the intercarpal joint and, therefore, does not require separate entry. Using the dorsal approach, enter the radio- carpal (antebrachiocarpal) or the intercarpal joints with the limb held and the carpus flexed. Locate the radiocarpal joint by palpating the medial aspect of the distal edge of the radius and the proximal edge of the radial carpal bone. Insert the needle midway between these two structures and medial to the medial edge of the palpate the radiocarpal and intercarpal joints medial to palpable tendon of the extensor carpi radialis radius (distal the palpable tendon of the extensor carpi radialis muscle. medial edge) muscle. The joint capsule is penetrated at a Note: The right carpus is being palpated. depth of about 0.5 inch (1.3 cm). Locate the intercarpal joint by palpating the distal edge of the radial carpal bone and the medial aspect of the proximal edge of the third radial carpal bone (proximal carpal bone. The technique of needle insertion edge) is similar to that for the radiocarpal joint. radiocarpal joint capsule It is important to point out that Ford et al47 and Moyer et al48 showed that the palmar out- pouchings of the carpometacarpal joint capsule extend into the fibers of the proximal portion of the suspensory ligament. -

Readingsample
Color Atlas of Human Anatomy Vol. 1: Locomotor System Bearbeitet von Werner Platzer 6. durchges. Auflage 2008. Buch. ca. 480 S. ISBN 978 3 13 533306 9 Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 130 Upper Limb: Bones, Ligaments, Joints Radiocarpal and Midcarpal Joints Ligaments in the Region of the Wrist (A–E) (A–E) Four groups of ligaments can be distin- The radiocarpal or wrist joint is an ellip- guished: soid joint formed on one side by the radius (1) and the articular disk (2) and on the Ligaments which unite the forearm bones with other by the proximal row of carpal bones.Not the carpal bones (violet). These include the all the carpal bones of the proximal row are ulnar collateral ligament (8), the radial col- in continual contact with the socket- lateral ligament (9), the palmar radiocarpal shaped articular facet of the radius and the ligament (10), the dorsal radiocarpal liga- disk. The triquetrum (3), only makes close ment (11), and the palmar ulnocarpal liga- contact with the disk during ulnar abduc- ment (12). tion and loses contact on radial abduction. Ligaments which unite the carpal bones with The capsule of the wrist joint is lax, dorsally one another,orintercarpal ligaments (red). These comprise the radiate carpal ligament Upper Limb relatively thin, and is reinforced by numer- ous ligaments. -

Bones and Joints of the Upper Limb: Forearm and Hand
Unit 4: Bones and joints of the upper limb: forearm and hand Chapter 6 (Upper limb) GENERAL OBJECTIVES: - recognize, name and correctly orient forearm and hand bones - understand movements in elbow, wrist and hand joints SPECIFIC OBJECTIVES: Bones of the forearm and hand Identify the bony features on each part of the following bones: RADIUS - Upper End - Shaft - Lower End ULNA - Upper End - Shaft - Lower End Deduce (from the shape of the articular surfaces) the movements at (i) the elbow joint and (ii) the radioulnar joints. Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Identify the following bones CARPALS - Proximal Row - Distal Row METACARPALS PHALANGES Identify the attachments of the Flexor Retinaculum and define the "Carpal Tunnel". Deduce (from the shape of the articular surfaces) the movements at (i) the wrist joint (ii) the carpometacarpal joint of the thumb (iii) metacarpophalangeal joints (iv) interphalangeal joints Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Joints of the forearm and hand Elbow Joint Articular Surfaces (Humeroulnar & Humeroradial) Fibrous Capsule & Joint Cavity Synovial Membrane Collateral Ligaments ( Medial & Lateral) Special Structures: Olecranon Bursa Other Bursae, Pads of Fat Movements at the Elbow Joint: Flexion/Extension Stability Carrying Angle Radioulnar Joints Proximal Radioulnar Joint Annular Ligament Distal Radioulnar -

Functional Anatomy
Hamill_ch05_137-186.qxd 11/2/07 3:55 PM Page 137 SECTION II Functional Anatomy CHAPTER 5 Functional Anatomy of the Upper Extremity CHAPTER 6 Functional Anatomy of the Lower Extremity CHAPTER 7 Functional Anatomy of the Trunk Hamill_ch05_137-186.qxd 11/2/07 3:55 PM Page 138 Hamill_ch05_137-186.qxd 11/2/07 3:55 PM Page 139 CHAPTER 5 Functional Anatomy of the Upper Extremity OBJECTIVES After reading this chapter, the student will be able to: 1. Describe the structure, support, and movements of the joints of the shoulder girdle, shoulder joint, elbow, wrist, and hand. 2. Describe the scapulohumeral rhythm in an arm movement. 3. Identify the muscular actions contributing to shoulder girdle, elbow, wrist, and hand movements. 4. Explain the differences in muscle strength across the different arm movements. 5. Identify common injuries to the shoulder, elbow, wrist, and hand. 6. Develop a set of strength and flexibility exercises for the upper extremity. 7. Identify the upper extremity muscular contributions to activities of daily living (e.g., rising from a chair), throwing, swimming, and swinging a golf club). 8. Describe some common wrist and hand positions used in precision or power. The Shoulder Complex Anatomical and Functional Characteristics Anatomical and Functional Characteristics of the Joints of the Wrist and Hand of the Joints of the Shoulder Combined Movements of the Wrist and Combined Movement Characteristics Hand of the Shoulder Complex Muscular Actions Muscular Actions Strength of the Hand and Fingers Strength of the Shoulder Muscles -

Synovial Joints • Typically Found at the Ends of Long Bones • Examples of Diarthroses • Shoulder Joint • Elbow Joint • Hip Joint • Knee Joint
Chapter 8 The Skeletal System Articulations Lecture Presentation by Steven Bassett Southeast Community College © 2015 Pearson Education, Inc. Introduction • Bones are designed for support and mobility • Movements are restricted to joints • Joints (articulations) exist wherever two or more bones meet • Bones may be in direct contact or separated by: • Fibrous tissue, cartilage, or fluid © 2015 Pearson Education, Inc. Introduction • Joints are classified based on: • Function • Range of motion • Structure • Makeup of the joint © 2015 Pearson Education, Inc. Classification of Joints • Joints can be classified based on their range of motion (function) • Synarthrosis • Immovable • Amphiarthrosis • Slightly movable • Diarthrosis • Freely movable © 2015 Pearson Education, Inc. Classification of Joints • Synarthrosis (Immovable Joint) • Sutures (joints found only in the skull) • Bones are interlocked together • Gomphosis (joint between teeth and jaw bones) • Periodontal ligaments of the teeth • Synchondrosis (joint within epiphysis of bone) • Binds the diaphysis to the epiphysis • Synostosis (joint between two fused bones) • Fusion of the three coxal bones © 2015 Pearson Education, Inc. Figure 6.3c The Adult Skull Major Sutures of the Skull Frontal bone Coronal suture Parietal bone Superior temporal line Inferior temporal line Squamous suture Supra-orbital foramen Frontonasal suture Sphenoid Nasal bone Temporal Lambdoid suture bone Lacrimal groove of lacrimal bone Ethmoid Infra-orbital foramen Occipital bone Maxilla External acoustic Zygomatic -

Ligaments of Elbow –Hinge: Sagittal Plane So Need Lateral and Medial Ligaments
Ligaments of Elbow –hinge: sagittal plane so need lateral and medial ligaments Ulnar Collateral ligament –on medial side; arising from medial epicondyle and stops excess valgus movement (lateral movement) - 3 BANDS: anterior (insert into coronoid process of ulnar) and posterior (insert into olecranon process of ulnar) and oblique Radial Collateral ligament –on lateral side; arising from medial epicondyle to stop excessive varus deviation (medial movement) - inserting: blends with annular ligament (doesn’t attach to radius so doesn’t limit rotation) - Articular capsule s lax anteriorly and posteriorly Fat pads –take impact of flex/ext; olecranon, radial and coronoid Olecranon bursa –between skin and olecranon process to reduce friction Movements at elbow joint- Flexion –mostly between humerus and ulnar (radial contact at close-packed positon Extension –oblique angle of trochlear; carrying angle –with elbow extension there is naturally slight forearm supination Biceps and triceps cross 2 joints- Likely to be stretched Work on both joints - distal joint more so than proximal joint Radioulnar Joint At each end of radius between radial notch on ulna and head of radius (proximal), and the ulnar notch on the radius and the ulnar head (distal) Pronation and supination (pivot motion) –linked motion via interosseous membrane which transmits forces - Proximal end only 20% through to radius (fall on elbow –most force transmitted to ulnar) - Distal end 80% through to radius (fall on wrist –most force onto radius) - Fracture at one end may -

Distal Radioulnar Joint
The joints Dr. Amja Shatarat, dept.of Anatomy, School of Medicne, The Uni. of Jordan 1- Type: Synovial hinge joint 2- Articulation: A-Between the trochlea and capitulum of the humerus and B-The trochlear notch of the ulna and the head of the radius 3-The articular surfaces are covered with hyaline cartilage. 4-Capsule: Anteriorly, it is attached above to the humerus Posteriorly, it is attached along the upper margins of above to the margins of the the coronoid and radial olecranon fossa of the fossae and to the front of humerus and below to the the medial and lateral upper margin and sides of epicondyles and below to the olecranon process of the margin of the coronoid the ulna and to the anular process of the ulna and to ligament. the anular ligament, which surrounds the head of the radius. important 5-Synovial membrane: This lines the capsule and covers fatty pads in the floors of the coronoid, radial, and olecranon fossae; it is continuous below with the synovial membrane of the proximal radioulnar joint. 6-Ligaments: a. The medial ligament is also triangular and The medial ligament is also triangular and consists principally of three strong bands: which connects different parts of the medial side of the humerus (medial epicondyle) and different parts of the upper end of the ulna. b. The lateral ligament: is triangular and is attached by its apex to the lateral epicondyle of the humerus and by its base to the upper margin of the anular ligament. 7-Important Relations ■■ Anteriorly: The brachialis, the tendon of the biceps, the median nerve, and the brachial artery ■■ Posteriorly: The triceps muscle, a small bursa intervening ■■ ■■ Laterally: The common extensor tendon and the supinator. -

Ligaments and Joints of the Upper Limb
This document was created by Alex Yartsev ([email protected]); if I have used your data or images and forgot to reference you, please email me. Ligaments and Joints of the Upper Limb Sternoclavicular joint Type of joint Saddle type synovial joint; but it functions like a ball-and-socket joint Interclavicular ligament ATYPICAL: fibrocartilage cover articular surfaces Articulating surfaces Articular disc Sternal facet of clavicle, clavicular facet of manubrium There is also an ARTICULAR DISC Articular capsule Surrounds the joint, including the clavicular epiphysis Attached to the articular disc Lined with synovial membrane, contains synovial fluid Ligaments Anterior and posterior sternoclavicular ligaments Interclavcular ligament Costoclavicular ligament Anterior sternoclavicular ligament Stability factors Costoclavicular ligament Not many muscles around, and the surfaces are incongruous, so the joint relies on the ligaments for stability. Anterior and posterior sternoclavicular ligaments reinforce it anteriorly and posteriorly Interclavicular ligament reinforces it superiorly Costoclavicular ligament reinforces it inferiorly Articular disc limits medial displacement Posterior sternoclavicular ligament Movements Articular disc: attached to the anterior and posterior Flexion, extension, rotation, anterior and posterior sternoclavicular ligaments movement, circumduction Blood supply Internal thoracic and subscapular arteries Nerve supply Nerve to subclavius Anterior sternoclavicular ligament Medial supraclavicular nerve All joint -

Prosthetic Arm Activities
Section II: Review Anatomy of the Human Arm Anatomical Terms of Location Three basic reference planes are used in human anatomy: Sagittal Plane – being a plane parallel to the sagittal suture (a dense, fibrous connective tissue joint between the two parietal bones of the skull), divides the body into sinister and dexter (left and right) portions. o The midsagittal or median plane is the midline; i.e. it would pass through the mid line structures such as the navel or spine Coronal or Frontal Plane – divides the body into dorsal and ventral (back and front, or posterior and anterior) portions. Transverse Plane – divides the body into the cranial and caudal (head and tail) portions. The following is a list of more commonly used terms which describe the position of anatomical structures: Anterior: to the front or in front; also called ventral Posterior: to the rear or behind Superior: above Inferior: below Lateral: away from the median plane or midline Medial: towards the median plane or midline Distal: away from the trunk or root of the limb Proximal: close to the trunk or root of a limb Superficial: close to the surface of the body or skin Deep: away from the body surface or skin MESA Day Prosthetic Arm Curriculum 3 These materials are for the internal use of California MESA staff and teachers only and should not be forwarded or used outside of MESA. Overview of the Anatomy of Human Arm The human arm contains bones, joints, muscles, nerves and blood vessels. The skeletal anatomy of the arm consists of bones of the upper extremity and the bones of the hand. -

Wrist & Hand Movement Coordination Deficits ICD-9-CM Codes
Wrist & Hand Movement Coordination Deficits ICD-9-CM codes: 842.01 Carpal sprains 842.02 Radiocarpal sprains ICF codes: Activities and Participation code: d4300 Lifting; d4301 Carrying in the hands; d4401 Grasping; d4452 Reaching; d4453 Turning or twisting the hands or arms Body Structure code: s73023 Ligaments and fasciae of the hand Body Functions code: b7601 Control of complex voluntary movements Common Historical Findings: Carpal ligaments and fasciae involvement: Effusion and pain Trauma, e.g. fall unto outstretched hand with wrist extended Wrist pain – worse at endrange of one motion more than others Common Impairment Findings - Related to the Reported Activity Limitation or Participation Restriction: Effusion if acute. Stiffness if longstanding End range pain with particular motion Restricted accessory movements of distal radioulnar, ulnomeniscotriquetral, radiocarpal, or intercarpal articulations Weak grip and/or pinch strength Physical Examination Procedures: Pain at end range of certain motions If pain and motion abnormality is with pronation - primarily assess distal radioulnar joint If pain and motion abnormality is with supination - primarily assess ulnomeniscotriquetral joints If pain and motion abnormality is with extension - primarily assess radiocarpal joints If pain and motion abnormality is with flexion - primarily assess intercarpal joints Cuong Pho DPT, Joe Godges DPT Loma Linda U DPT Program KPSoCal Ortho PT Residency Wrist Accessory Movement Test Wrist Accessory Movement Test Distal Radioulnar Joint Ulnomeniscotriquetral