Distal Radioulnar Joint
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4Th SESSION 1
2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4th SESSION 1: Carpal Ligament 1 Stable Central Column Theory of Carpal Mechanics Michael Sandow FRACS Wakefield Orthopaedic Clinic Adelaide, Australia Background: The carpus is a complicated and functionally challenged mechanical system and advancements in the understanding have been compromised by the recognition that there is no standard carpal mechanical system and no typical wrist. This paper cover component of a larger project that seeks to develop a kinetic model of wrist mechanics to allow reverse analysis of the specific biomechanical controls or rule of a specific patient's carpus, and then use those to create a forward mathematical model to reproduce the unique individual's anatomical motion based on the extracted rules. Objectives and Methods: Based on previous observations, the carpus essentially moves with only 2 degrees of freedom - pitch (flexion / extension) and yaw (radial deviation / ulnar deviation), while largely preventing roll (pronation / supination). The object of this paper is therefore to present the background and justification to support the rules based motion (RBM) concept states that the motion of a mechanical system, such as the wrist, is the net interplay of 4 rules - morphology, constraint, interaction and load. The Stable Central Column Theory (SCCT) of wrist mechanics applies the concept of RBM to the carpus, and by using a reverse engineering computational analysis model, identified a consistent pattern of isometric constraints, creating a "Two-Gear Four-Bar" linkage. This study assessed the motion of the carpus using a 3D dynamic visualization model, and the hypothesis was that the pattern and direction of motion of the proximal row, and the distal row with respect the immediately cephalad carpal bones or radius would be very similar in all directions of wrist motion. -
Lecture Notes on Human Anatomy. Part One, Fourth Edition. PUB DATE Sep 89 NOTE 79P.; for Related Documents, See SE 051 219-221
DOCUMENT RESUME ED 315 320 SE 051 218 AUTHOR Conrey, Kathleen TITLE Lecture Notes on Human Anatomy. Part One, Fourth Edition. PUB DATE Sep 89 NOTE 79p.; For related documents, see SE 051 219-221. Black and white illustrations will not reproduce clearly. AVAILABLE FROM Aramaki Design and Publications, 12077 Jefferson Blvd., Culver City, CA 90506 ($7.75). PUB TYPE Guides - Classroom Use - Materials (For Learner) (051) EDRS PRICE MF01 Plus Postage. PC Not Available from EDRS. DESCRIPTORS *Anatomy; *Biological Sciences; *College Science; Higher Education; *Human Body; *Lecture Method; Science Education; Secondary Education; Secondary School Science; Teaching Guides; Teaching Methods ABSTRACT During the process of studying the specific course content of human anatomy, students are being educated to expand their vocabulary, deal successfully with complex tasks, anduse a specific way of thinking. This is the first volume in a set of notes which are designed to accompany a lecture series in human anatomy. This volume Includes discussions of anatomical planes and positions, body cavities, and architecture; studies of the skeleton including bones and joints; studies of the musculature of the body; and studiesof the nervous system including the central, autonomic, motor and sensory systems. (CW) *****1.**k07********Y*******t1.****+***********,****A*******r****** % Reproductions supplied by EDRS are the best that can be made from the original document. **************************************************************A**t***** "PERMISSION TO REPRODUCE -

38.3 Joints and Skeletal Movement.Pdf
1198 Chapter 38 | The Musculoskeletal System Decalcification of Bones Question: What effect does the removal of calcium and collagen have on bone structure? Background: Conduct a literature search on the role of calcium and collagen in maintaining bone structure. Conduct a literature search on diseases in which bone structure is compromised. Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of bones that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium back to decalcified bones. Test the hypothesis: Test the prediction by removing calcium from chicken bones by placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified bone by placing the decalcified chicken bones into a jar of water with calcium supplements added. Test the prediction by denaturing the collagen from the bones by baking them at 250°C for three hours. Analyze the data: Create a table showing the changes in bone flexibility, strength, and mass in the three different environments. Report the results: Under which conditions was the bone most flexible? Under which conditions was the bone the strongest? Draw a conclusion: Did the results support or refute the hypothesis? How do the results observed in this experiment correspond to diseases that destroy bone tissue? 38.3 | Joints and Skeletal Movement By the end of this section, you will be able to do the following: • Classify the different types of joints on the basis of structure • Explain the role of joints in skeletal movement The point at which two or more bones meet is called a joint, or articulation. -

REVIEW ARTICLE Osteoarthritis of the Wrist
REVIEW ARTICLE Osteoarthritis of the Wrist Krista E. Weiss, Craig M. Rodner, MD From Harvard College, Cambridge, MA and Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Osteoarthritis of the wrist is one of the most common conditions encountered by hand surgeons. It may result from a nonunited or malunited fracture of the scaphoid or distal radius; disruption of the intercarpal, radiocarpal, radioulnar, or ulnocarpal ligaments; avascular necrosis of the carpus; or a developmental abnormality. Whatever the cause, subsequent abnormal joint loading produces a spectrum of symptoms, from mild swelling to considerable pain and limitations of motion as the involved joints degenerate. A meticulous clinical and radiographic evaluation is required so that the pain-generating articulation(s) can be identi- fied and eliminated. This article reviews common causes of wrist osteoarthritis and their surgical treatment alternatives. (J Hand Surg 2007;32A:725–746. Copyright © 2007 by the American Society for Surgery of the Hand.) Key words: Wrist, osteoarthritis, arthrodesis, carpectomy, SLAC. here are several different causes, both idio- of events is analogous to SLAC wrist and has pathic and traumatic, of wrist osteoarthritis. been termed scaphoid nonunion advanced collapse Untreated cases of idiopathic carpal avascular (SNAC). Wrist osteoarthritis can also occur second- T 1 2 necrosis, as in Kienböck’s or Preiser’s disease, may ary to an intra-articular fracture of the distal radius or result in radiocarpal arthritis. Congenital wrist abnor- ulna or from an extra-articular fracture resulting in malities, such as Madelung’s deformity,3,4 can lead malunion and abnormal joint loading. -
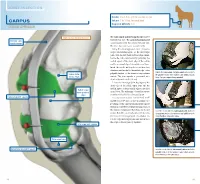
Carpus Volume: 7 to 10 Ml for Each Joint Degree of Difficulty: 1/3 Dorsal Approach
JOINT INJECTION needle: 1 to 1.5 in. (2.5 to 3.8 cm), 20 ga Carpus volume: 7 to 10 ml for each joint Degree of difficulty: 1/3 Dorsal approach right carpus, dorsomedial view The radiocarpal and intercarpal joints can be extensor carpi entered with ease. The carpometacarpal joint radialis tendon communicates with the intercarpal joint and, therefore, does not require separate entry. Using the dorsal approach, enter the radio- carpal (antebrachiocarpal) or the intercarpal joints with the limb held and the carpus flexed. Locate the radiocarpal joint by palpating the medial aspect of the distal edge of the radius and the proximal edge of the radial carpal bone. Insert the needle midway between these two structures and medial to the medial edge of the palpate the radiocarpal and intercarpal joints medial to palpable tendon of the extensor carpi radialis radius (distal the palpable tendon of the extensor carpi radialis muscle. medial edge) muscle. The joint capsule is penetrated at a Note: The right carpus is being palpated. depth of about 0.5 inch (1.3 cm). Locate the intercarpal joint by palpating the distal edge of the radial carpal bone and the medial aspect of the proximal edge of the third radial carpal bone (proximal carpal bone. The technique of needle insertion edge) is similar to that for the radiocarpal joint. radiocarpal joint capsule It is important to point out that Ford et al47 and Moyer et al48 showed that the palmar out- pouchings of the carpometacarpal joint capsule extend into the fibers of the proximal portion of the suspensory ligament. -

Readingsample
Color Atlas of Human Anatomy Vol. 1: Locomotor System Bearbeitet von Werner Platzer 6. durchges. Auflage 2008. Buch. ca. 480 S. ISBN 978 3 13 533306 9 Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 130 Upper Limb: Bones, Ligaments, Joints Radiocarpal and Midcarpal Joints Ligaments in the Region of the Wrist (A–E) (A–E) Four groups of ligaments can be distin- The radiocarpal or wrist joint is an ellip- guished: soid joint formed on one side by the radius (1) and the articular disk (2) and on the Ligaments which unite the forearm bones with other by the proximal row of carpal bones.Not the carpal bones (violet). These include the all the carpal bones of the proximal row are ulnar collateral ligament (8), the radial col- in continual contact with the socket- lateral ligament (9), the palmar radiocarpal shaped articular facet of the radius and the ligament (10), the dorsal radiocarpal liga- disk. The triquetrum (3), only makes close ment (11), and the palmar ulnocarpal liga- contact with the disk during ulnar abduc- ment (12). tion and loses contact on radial abduction. Ligaments which unite the carpal bones with The capsule of the wrist joint is lax, dorsally one another,orintercarpal ligaments (red). These comprise the radiate carpal ligament Upper Limb relatively thin, and is reinforced by numer- ous ligaments. -

Bones and Joints of the Upper Limb: Forearm and Hand
Unit 4: Bones and joints of the upper limb: forearm and hand Chapter 6 (Upper limb) GENERAL OBJECTIVES: - recognize, name and correctly orient forearm and hand bones - understand movements in elbow, wrist and hand joints SPECIFIC OBJECTIVES: Bones of the forearm and hand Identify the bony features on each part of the following bones: RADIUS - Upper End - Shaft - Lower End ULNA - Upper End - Shaft - Lower End Deduce (from the shape of the articular surfaces) the movements at (i) the elbow joint and (ii) the radioulnar joints. Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Identify the following bones CARPALS - Proximal Row - Distal Row METACARPALS PHALANGES Identify the attachments of the Flexor Retinaculum and define the "Carpal Tunnel". Deduce (from the shape of the articular surfaces) the movements at (i) the wrist joint (ii) the carpometacarpal joint of the thumb (iii) metacarpophalangeal joints (iv) interphalangeal joints Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Joints of the forearm and hand Elbow Joint Articular Surfaces (Humeroulnar & Humeroradial) Fibrous Capsule & Joint Cavity Synovial Membrane Collateral Ligaments ( Medial & Lateral) Special Structures: Olecranon Bursa Other Bursae, Pads of Fat Movements at the Elbow Joint: Flexion/Extension Stability Carrying Angle Radioulnar Joints Proximal Radioulnar Joint Annular Ligament Distal Radioulnar -

Gen Anat-Joints
JOINTS Joint is a junction between two or more bones Classification •Functional Based on the range and type of movement they permit •Structural On the basis of their anatomic structure Functional Classification • Synarthrosis No movement e.g. Fibrous joint • Amphiarthrosis Slight movement e.g. Cartilagenous joint • Diarthrosis Movement present Cavity present Also called as Synovial joint eg.shoulder joint Structural Classification Based on type of connective tissue binding the two adjacent articulating bones Presence or absence of synovial cavity in between the articulating bone • Fibrous • Cartilagenous • Synovial Fibrous Joint Bones are connected to each other by fibrous (connective ) tissue No movement No synovial cavity • Suture • Syndesmosis • Gomphosis Sutural Joints • A thin layer of dens fibrous tissue binds the adjacent bones • These appear between the bones which ossify in membrane • Present between the bones of skull e.g . coronal suture, sagittal suture • Schindylesis: – rigid bone fits in to a groove on a neighbouring bone e.g. Vomer and sphenoid Gomphosis • Peg and socket variety • Cone shaped root of tooth fits in to a socket of jaw • Immovable • Root is attached to the socket by fibrous tissue (periodontal ligament). Syndesmosis • Bony surfaces are bound together by interosseous ligament or membrane • Membrane permits slight movement • Functionally classified as amphiarthrosis e.g. inferior tibiofibular joint Cartilaginous joint • Bones are held together by cartilage • Absence of synovial cavity . Synchondrosis . Symphysis Synchondrosis • Primary cartilaginous joint • Connecting material between two bones is hyaline cartilage • Temporary joint • Immovable joint • After a certain age cartilage is replaced by bone (synostosis) • e.g. Epiphyseal plate connecting epiphysis and diphysis of a long bone, joint between basi-occiput and basi-sphenoid Symphysis • Secondary cartilaginous joint (fibrocartilaginous joint) • Permanent joint • Occur in median plane of the body • Slightly movable • e.g. -
RADIOULNAR JOINTS the Radius and Ulna Articulate by –
RADIOULNAR JOINTS The radius and ulna articulate by – • Synovial 1. Superior radioulnar joint 2. Inferior radioulnar joint • Non synovial Middle radioulnar union Superior Radioulnar Joint This articulation is a trochoid or pivot-joint between • the circumference of the head of the radius • ring formed by the radial notch of the ulna and the annular ligament. The Annular Ligament (orbicular ligament) This ligament is a strong band of fibers, which encircles the head of the radius, and retains it in contact with the radial notch of the ulna. It forms about four-fifths of the osseo- fibrous ring, and is attached to the anterior and posterior margins of the radial notch a few of its lower fibers are continued around below the cavity and form at this level a complete fibrous ring. Its upper border blends with the capsule of elbow joint while from its lower border a thin loose synovial membrane passes to be attached to the neck of the radius The superficial surface of the annular ligament is strengthened by the radial collateral ligament of the elbow, and affords origin to part of the Supinator. Its deep surface is smooth, and lined by synovial membrane, which is continuous with that of the elbow-joint. Quadrate ligament A thickened band which extends from the inferior border of the annular ligament below the radial notch to the neck of the radius is known as the quadrate ligament. Movements The movements allowed in this articulation are limited to rotatory movements of the head of the radius within the ring formed by the annular ligament and the radial notch of the ulna • rotation forward being called pronation • rotation backward, supination Middle Radioulnar Union The shafts of the radius and ulna are connected by Oblique Cord and Interosseous Membrane The Oblique Cord (oblique ligament) The oblique cord is a small, flattened band, extending downward and laterally, from the lateral side of the ulnar tuberosity to the radius a little below the radial tuberosity. -
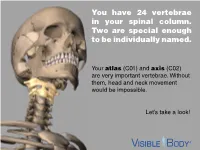
You Have 24 Vertebrae in Your Spinal Column. Two Are Special Enough to Be Individually Named
You have 24 vertebrae in your spinal column. Two are special enough to be individually named. Your atlas (C01) and axis (C02) are very important vertebrae. Without them, head and neck movement would be impossible. Let’s take a look! The atlas and axis are the most superior bones in the cervical vertebrae. The atlas is the top-most vertebra, sitting just below the skull. The axis is below it. Together, the atlas and axis support the skull, facilitate head and neck movement, and protect the spinal cord. (Think of the atlas and axis as best buds for life. You will never find one without the other.) www.visiblebody.com There are many types of vertebral joints, but the atlas and axis form the only craniovertebral joints in the human body. A craniovertebral joint is a joint that permits movement between the cervical vertebrae and the neurocranium. The atlanto-occipital joint (pictured) connects the atlas to the occipital bone. It flexes the neck, allowing you to nod your head. The atlanto-axial joint connects the axis to the atlas. It permits rotational movement of the head. www.visiblebody.com The atlanto-axial joint is a compound synovial joint. This pivot joint allows for rotation of the head and neck. Watch this joint in action! A pivot joint is made by the end of one articulating bone rotating in a ring formed by another bone and its ligaments. www.visiblebody.com The atlas and axis are part of the seven cervical vertebrae. These vertebrae have a few unique features: They are the smallest of the vertebrae. -

Structural Kinesiology (PDF)
Kinesiology & Body Mechanics • Kinesiology - study of motion or human movement • Anatomic kinesiology - study of human Chapter 1 musculoskeletal system & musculotendinous system Foundations of Structural Kinesiology • Biomechanics - application of mechanical physics to human motion Manual of Structural Kinesiology R.T. Floyd, EdD, ATC, CSCS Manual of Manual of Structural Kinesiology Foundations of Structural Kinesiology 1-1 Structural Kinesiology Foundations of Structural Kinesiology 1-2 Kinesiology & Body Mechanics Kinesiology & Body Mechanics • Structural kinesiology - study of muscles as • Muscles vary greatly in size, shape, & they are involved in science of movement structure from one part of body to another • Both skeletal & muscular structures are • More than 600 muscles are found in human involved body • Bones are different sizes & shapes − particularly at the joints, which allow or limit movement Manual of Manual of Structural Kinesiology Foundations of Structural Kinesiology 1-3 Structural Kinesiology Foundations of Structural Kinesiology 1-4 Who needs Kinesiology? Why Kinesiology? • Anatomists, coaches, strength and • should have an adequate knowledge & understanding of all large muscle groups to conditioning specialists, personal teach others how to strengthen, improve, & trainers, nurses, physical educators, maintain these parts of human body physical therapists, physicians, athletic • should not only know how & what to do in trainers, massage therapists & others in relation to conditioning & training but also know health-related -

Functional Anatomy
Hamill_ch05_137-186.qxd 11/2/07 3:55 PM Page 137 SECTION II Functional Anatomy CHAPTER 5 Functional Anatomy of the Upper Extremity CHAPTER 6 Functional Anatomy of the Lower Extremity CHAPTER 7 Functional Anatomy of the Trunk Hamill_ch05_137-186.qxd 11/2/07 3:55 PM Page 138 Hamill_ch05_137-186.qxd 11/2/07 3:55 PM Page 139 CHAPTER 5 Functional Anatomy of the Upper Extremity OBJECTIVES After reading this chapter, the student will be able to: 1. Describe the structure, support, and movements of the joints of the shoulder girdle, shoulder joint, elbow, wrist, and hand. 2. Describe the scapulohumeral rhythm in an arm movement. 3. Identify the muscular actions contributing to shoulder girdle, elbow, wrist, and hand movements. 4. Explain the differences in muscle strength across the different arm movements. 5. Identify common injuries to the shoulder, elbow, wrist, and hand. 6. Develop a set of strength and flexibility exercises for the upper extremity. 7. Identify the upper extremity muscular contributions to activities of daily living (e.g., rising from a chair), throwing, swimming, and swinging a golf club). 8. Describe some common wrist and hand positions used in precision or power. The Shoulder Complex Anatomical and Functional Characteristics Anatomical and Functional Characteristics of the Joints of the Wrist and Hand of the Joints of the Shoulder Combined Movements of the Wrist and Combined Movement Characteristics Hand of the Shoulder Complex Muscular Actions Muscular Actions Strength of the Hand and Fingers Strength of the Shoulder Muscles