Module Two: Anatomy of the Athlete
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Tenosynovitis of the Deep Digital Flexor Tendon in Horses R
TENOSYNOVITIS OF THE DEEP DIGITAL FLEXOR TENDON IN HORSES R. W. Van Pelt, W. F. Riley, Jr. and P. J. Tillotson* INTRODUCTION sheaths, statistical comparisons were made be- tween certain values determined for synovial TENOSYNOVITIS of the deep digital flexor ten- effusions from tarsal synovial sheaths of don (thoroughpin) in horses is manifested by affected horses and synovial fluids from the distention of its tarsal synovial sheath due to tibiotarsal joints of control formation of an excessive synovial effusion. Un- horses. less tenosynovitis is acute, signs of inflamma- Control Horses tion, pain or lameness are absent (1). Tendinitis Five healthy horses ranging in age from can and does occur in conjunction with inflam- four to nine years were used as controls. Four mation of the tarsal synovial sheath. of the horses were Thoroughbreds and one As tendons function they are frequently sub- horse was of Quarter Horse breeding. All jected to considerable strain, peritendinous control horses were geldings. Synovial fluid pressure, and friction between the parietal and samples were obtained from the tibiotarsal joint. visceral layers of the tendon sheath (2). Acute direct trauma or trauma that is multiple and Hematologic Determinations minor can precipitate tenosynovitis. In acute Blood samples for determination of serum tenosynovitis of the deep digital flexor tendon, sugar content (measured as total reducing sub- the ensuing inflammatory reaction affects the stances) were obtained from the jugular vein tarsal synovial sheath, which responds to in- prior to aspiration of the tarsal synovial sheath flammation by formation of an excessive syno- in affected horses and the tibiotarsal joint in vial effusion. -
Lecture Notes on Human Anatomy. Part One, Fourth Edition. PUB DATE Sep 89 NOTE 79P.; for Related Documents, See SE 051 219-221
DOCUMENT RESUME ED 315 320 SE 051 218 AUTHOR Conrey, Kathleen TITLE Lecture Notes on Human Anatomy. Part One, Fourth Edition. PUB DATE Sep 89 NOTE 79p.; For related documents, see SE 051 219-221. Black and white illustrations will not reproduce clearly. AVAILABLE FROM Aramaki Design and Publications, 12077 Jefferson Blvd., Culver City, CA 90506 ($7.75). PUB TYPE Guides - Classroom Use - Materials (For Learner) (051) EDRS PRICE MF01 Plus Postage. PC Not Available from EDRS. DESCRIPTORS *Anatomy; *Biological Sciences; *College Science; Higher Education; *Human Body; *Lecture Method; Science Education; Secondary Education; Secondary School Science; Teaching Guides; Teaching Methods ABSTRACT During the process of studying the specific course content of human anatomy, students are being educated to expand their vocabulary, deal successfully with complex tasks, anduse a specific way of thinking. This is the first volume in a set of notes which are designed to accompany a lecture series in human anatomy. This volume Includes discussions of anatomical planes and positions, body cavities, and architecture; studies of the skeleton including bones and joints; studies of the musculature of the body; and studiesof the nervous system including the central, autonomic, motor and sensory systems. (CW) *****1.**k07********Y*******t1.****+***********,****A*******r****** % Reproductions supplied by EDRS are the best that can be made from the original document. **************************************************************A**t***** "PERMISSION TO REPRODUCE -

38.3 Joints and Skeletal Movement.Pdf
1198 Chapter 38 | The Musculoskeletal System Decalcification of Bones Question: What effect does the removal of calcium and collagen have on bone structure? Background: Conduct a literature search on the role of calcium and collagen in maintaining bone structure. Conduct a literature search on diseases in which bone structure is compromised. Hypothesis: Develop a hypothesis that states predictions of the flexibility, strength, and mass of bones that have had the calcium and collagen components removed. Develop a hypothesis regarding the attempt to add calcium back to decalcified bones. Test the hypothesis: Test the prediction by removing calcium from chicken bones by placing them in a jar of vinegar for seven days. Test the hypothesis regarding adding calcium back to decalcified bone by placing the decalcified chicken bones into a jar of water with calcium supplements added. Test the prediction by denaturing the collagen from the bones by baking them at 250°C for three hours. Analyze the data: Create a table showing the changes in bone flexibility, strength, and mass in the three different environments. Report the results: Under which conditions was the bone most flexible? Under which conditions was the bone the strongest? Draw a conclusion: Did the results support or refute the hypothesis? How do the results observed in this experiment correspond to diseases that destroy bone tissue? 38.3 | Joints and Skeletal Movement By the end of this section, you will be able to do the following: • Classify the different types of joints on the basis of structure • Explain the role of joints in skeletal movement The point at which two or more bones meet is called a joint, or articulation. -

Transition Phase Towards Psoriatic Arthritis: Clinical and Ultrasonographic Characterisation of Psoriatic Arthralgia
Psoriatic arthritis RMD Open: first published as 10.1136/rmdopen-2019-001067 on 23 October 2019. Downloaded from ORIGINAL ARTICLE Transition phase towards psoriatic arthritis: clinical and ultrasonographic characterisation of psoriatic arthralgia Alen Zabotti ,1 Dennis G McGonagle,2 Ivan Giovannini,1 Enzo Errichetti,3 Francesca Zuliani,1 Anna Zanetti,4 Ilaria Tinazzi,5 Orazio De Lucia,6 Alberto Batticciotto ,7 Luca Idolazzi,8 Garifallia Sakellariou,9 Sara Zandonella Callegher,1 Stefania Sacco,1 Luca Quartuccio,1 Annamaria Iagnocco,10 Salvatore De Vita1 To cite: Zabotti A, ABSTRACT McGonagle DG, Giovannini I, Objective Non-specific musculoskeletal pain is common Key messages et al. Transition phase in subjects destined to develop psoriatic arthritis (PsA). towards psoriatic arthritis: We evaluated psoriatic patients with arthralgia (PsOAr) What is already known about this subject? clinical and ultrasonographic compared with psoriasis alone (PsO) and healthy controls ► Patients with psoriasis have a period of non-specific characterisation of psoriatic joint symptoms (ie, arthralgia) before psoriatic ar- arthralgia. RMD Open (HCs) using ultrasonography (US) to investigate the anatomical basis for joint symptoms in PsOAr and the thritis (PsA) development, but the anatomical basis 2019;5:e001067. doi:10.1136/ for such arthralgia remains to be defined. rmdopen-2019-001067 link between these imaging findings and subsequent PsA transition. What does this study add? Methods A cross-sectional prevalence analysis of ► Tenosynovitis could be an important contributor to Received 25 July 2019 clinical and US abnormalities (including inflammatory non-specific musculoskeletal symptoms in psoriatic Revised 3 October 2019 and structural lesions) in PsOAr (n=61), PsO (n=57) and patients with arthralgia (PsOAr). -

Gen Anat-Joints
JOINTS Joint is a junction between two or more bones Classification •Functional Based on the range and type of movement they permit •Structural On the basis of their anatomic structure Functional Classification • Synarthrosis No movement e.g. Fibrous joint • Amphiarthrosis Slight movement e.g. Cartilagenous joint • Diarthrosis Movement present Cavity present Also called as Synovial joint eg.shoulder joint Structural Classification Based on type of connective tissue binding the two adjacent articulating bones Presence or absence of synovial cavity in between the articulating bone • Fibrous • Cartilagenous • Synovial Fibrous Joint Bones are connected to each other by fibrous (connective ) tissue No movement No synovial cavity • Suture • Syndesmosis • Gomphosis Sutural Joints • A thin layer of dens fibrous tissue binds the adjacent bones • These appear between the bones which ossify in membrane • Present between the bones of skull e.g . coronal suture, sagittal suture • Schindylesis: – rigid bone fits in to a groove on a neighbouring bone e.g. Vomer and sphenoid Gomphosis • Peg and socket variety • Cone shaped root of tooth fits in to a socket of jaw • Immovable • Root is attached to the socket by fibrous tissue (periodontal ligament). Syndesmosis • Bony surfaces are bound together by interosseous ligament or membrane • Membrane permits slight movement • Functionally classified as amphiarthrosis e.g. inferior tibiofibular joint Cartilaginous joint • Bones are held together by cartilage • Absence of synovial cavity . Synchondrosis . Symphysis Synchondrosis • Primary cartilaginous joint • Connecting material between two bones is hyaline cartilage • Temporary joint • Immovable joint • After a certain age cartilage is replaced by bone (synostosis) • e.g. Epiphyseal plate connecting epiphysis and diphysis of a long bone, joint between basi-occiput and basi-sphenoid Symphysis • Secondary cartilaginous joint (fibrocartilaginous joint) • Permanent joint • Occur in median plane of the body • Slightly movable • e.g. -

Section 1 Upper Limb Anatomy 1) with Regard to the Pectoral Girdle
Section 1 Upper Limb Anatomy 1) With regard to the pectoral girdle: a) contains three joints, the sternoclavicular, the acromioclavicular and the glenohumeral b) serratus anterior, the rhomboids and subclavius attach the scapula to the axial skeleton c) pectoralis major and deltoid are the only muscular attachments between the clavicle and the upper limb d) teres major provides attachment between the axial skeleton and the girdle 2) Choose the odd muscle out as regards insertion/origin: a) supraspinatus b) subscapularis c) biceps d) teres minor e) deltoid 3) Which muscle does not insert in or next to the intertubecular groove of the upper humerus? a) pectoralis major b) pectoralis minor c) latissimus dorsi d) teres major 4) Identify the incorrect pairing for testing muscles: a) latissimus dorsi – abduct to 60° and adduct against resistance b) trapezius – shrug shoulders against resistance c) rhomboids – place hands on hips and draw elbows back and scapulae together d) serratus anterior – push with arms outstretched against a wall 5) Identify the incorrect innervation: a) subclavius – own nerve from the brachial plexus b) serratus anterior – long thoracic nerve c) clavicular head of pectoralis major – medial pectoral nerve d) latissimus dorsi – dorsal scapular nerve e) trapezius – accessory nerve 6) Which muscle does not extend from the posterior surface of the scapula to the greater tubercle of the humerus? a) teres major b) infraspinatus c) supraspinatus d) teres minor 7) With regard to action, which muscle is the odd one out? a) teres -

CVM 6100 Veterinary Gross Anatomy
2010 CVM 6100 Veterinary Gross Anatomy General Anatomy & Carnivore Anatomy Lecture Notes by Thomas F. Fletcher, DVM, PhD and Christina E. Clarkson, DVM, PhD 1 CONTENTS Connective Tissue Structures ........................................3 Osteology .........................................................................5 Arthrology .......................................................................7 Myology .........................................................................10 Biomechanics and Locomotion....................................12 Serous Membranes and Cavities .................................15 Formation of Serous Cavities ......................................17 Nervous System.............................................................19 Autonomic Nervous System .........................................23 Abdominal Viscera .......................................................27 Pelvis, Perineum and Micturition ...............................32 Female Genitalia ...........................................................35 Male Genitalia...............................................................37 Head Features (Lectures 1 and 2) ...............................40 Cranial Nerves ..............................................................44 Connective Tissue Structures Histologic types of connective tissue (c.t.): 1] Loose areolar c.t. — low fiber density, contains spaces that can be filled with fat or fluid (edema) [found: throughout body, under skin as superficial fascia and in many places as deep fascia] -

Review Vasculature of the Normal and Arthritic Synovial Joint
Histol Histopathol (2001) 16: 277-284 001: 10.14670/HH-16.277 Histology and http://www.ehu.es/histol-histopathol Histopathology Cellular and Molecular Biology Review Vasculature of the normal and arthritic synovial jOint L. Haywood and D.A. Walsh Academic Rheumatology, Nottingham University Clinical Sciences Building, City Hospital, Nottingham, UK Summary. The vasculature of the normal and arthritic synovium as the major nutrient supply for articular knee is described. The joint contains a number of cartilage (Walsh et aI. , 1997). Arterio-venous shunts different tissues, many of which are heterogeneous and have been identified in the synovium and offer a each with varying degrees of vascularization. In the potential mechanism for the control of synovial blood normal joint the vasculature is highly organised, some flow (Lindstrom and Branemark, 1962). tissues are highly vascular with well defined vascular Joints can be classified into groups, according to organisation, whilst other tissues are avascular. During their location, range and nature of motion or anatomy. arthritis vascular turnover is increased. This vascular Synovial joints are present throughout the skeleton and plasticity leads to redistribution of the vascular bed and vary in size. However, due to accessibility and relatively may compromise its functional ability. The normal joint large size in man and experimental animals the knee is is able to regulate its blood flow, but this ability may be the most extensively studied synovial joint. Knee compromised by the inflammation and increased arthritis is a major source of distress and disability in synovial fluid volume that are associated with joint man. This paper focuses on the vasculature of the knee. -

RADIOULNAR JOINTS the Radius and Ulna Articulate by –
RADIOULNAR JOINTS The radius and ulna articulate by – • Synovial 1. Superior radioulnar joint 2. Inferior radioulnar joint • Non synovial Middle radioulnar union Superior Radioulnar Joint This articulation is a trochoid or pivot-joint between • the circumference of the head of the radius • ring formed by the radial notch of the ulna and the annular ligament. The Annular Ligament (orbicular ligament) This ligament is a strong band of fibers, which encircles the head of the radius, and retains it in contact with the radial notch of the ulna. It forms about four-fifths of the osseo- fibrous ring, and is attached to the anterior and posterior margins of the radial notch a few of its lower fibers are continued around below the cavity and form at this level a complete fibrous ring. Its upper border blends with the capsule of elbow joint while from its lower border a thin loose synovial membrane passes to be attached to the neck of the radius The superficial surface of the annular ligament is strengthened by the radial collateral ligament of the elbow, and affords origin to part of the Supinator. Its deep surface is smooth, and lined by synovial membrane, which is continuous with that of the elbow-joint. Quadrate ligament A thickened band which extends from the inferior border of the annular ligament below the radial notch to the neck of the radius is known as the quadrate ligament. Movements The movements allowed in this articulation are limited to rotatory movements of the head of the radius within the ring formed by the annular ligament and the radial notch of the ulna • rotation forward being called pronation • rotation backward, supination Middle Radioulnar Union The shafts of the radius and ulna are connected by Oblique Cord and Interosseous Membrane The Oblique Cord (oblique ligament) The oblique cord is a small, flattened band, extending downward and laterally, from the lateral side of the ulnar tuberosity to the radius a little below the radial tuberosity. -
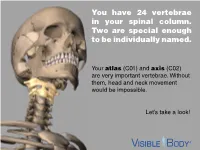
You Have 24 Vertebrae in Your Spinal Column. Two Are Special Enough to Be Individually Named
You have 24 vertebrae in your spinal column. Two are special enough to be individually named. Your atlas (C01) and axis (C02) are very important vertebrae. Without them, head and neck movement would be impossible. Let’s take a look! The atlas and axis are the most superior bones in the cervical vertebrae. The atlas is the top-most vertebra, sitting just below the skull. The axis is below it. Together, the atlas and axis support the skull, facilitate head and neck movement, and protect the spinal cord. (Think of the atlas and axis as best buds for life. You will never find one without the other.) www.visiblebody.com There are many types of vertebral joints, but the atlas and axis form the only craniovertebral joints in the human body. A craniovertebral joint is a joint that permits movement between the cervical vertebrae and the neurocranium. The atlanto-occipital joint (pictured) connects the atlas to the occipital bone. It flexes the neck, allowing you to nod your head. The atlanto-axial joint connects the axis to the atlas. It permits rotational movement of the head. www.visiblebody.com The atlanto-axial joint is a compound synovial joint. This pivot joint allows for rotation of the head and neck. Watch this joint in action! A pivot joint is made by the end of one articulating bone rotating in a ring formed by another bone and its ligaments. www.visiblebody.com The atlas and axis are part of the seven cervical vertebrae. These vertebrae have a few unique features: They are the smallest of the vertebrae. -

Structural Kinesiology (PDF)
Kinesiology & Body Mechanics • Kinesiology - study of motion or human movement • Anatomic kinesiology - study of human Chapter 1 musculoskeletal system & musculotendinous system Foundations of Structural Kinesiology • Biomechanics - application of mechanical physics to human motion Manual of Structural Kinesiology R.T. Floyd, EdD, ATC, CSCS Manual of Manual of Structural Kinesiology Foundations of Structural Kinesiology 1-1 Structural Kinesiology Foundations of Structural Kinesiology 1-2 Kinesiology & Body Mechanics Kinesiology & Body Mechanics • Structural kinesiology - study of muscles as • Muscles vary greatly in size, shape, & they are involved in science of movement structure from one part of body to another • Both skeletal & muscular structures are • More than 600 muscles are found in human involved body • Bones are different sizes & shapes − particularly at the joints, which allow or limit movement Manual of Manual of Structural Kinesiology Foundations of Structural Kinesiology 1-3 Structural Kinesiology Foundations of Structural Kinesiology 1-4 Who needs Kinesiology? Why Kinesiology? • Anatomists, coaches, strength and • should have an adequate knowledge & understanding of all large muscle groups to conditioning specialists, personal teach others how to strengthen, improve, & trainers, nurses, physical educators, maintain these parts of human body physical therapists, physicians, athletic • should not only know how & what to do in trainers, massage therapists & others in relation to conditioning & training but also know health-related -

Tendon — Function-Related Structure, Simple Healing Process and Mysterious Ageing J
Folia Morphol. Vol. 77, No. 3, pp. 416–427 DOI: 10.5603/FM.a2018.0006 R E V I E W A R T I C L E Copyright © 2018 Via Medica ISSN 0015–5659 www.fm.viamedica.pl Tendon — function-related structure, simple healing process and mysterious ageing J. Zabrzyński1, Ł. Łapaj2, Ł. Paczesny3, A. Zabrzyńska4, D. Grzanka5 1Department of Orthopaedic Surgery, Multidisciplinary Hospital, Inowroclaw, Poland 2Department of General, Oncologic Orthopaedics and Traumatology, Karol Marcinkowski Medical University, Poznan, Poland 3Department of Orthopaedic Surgery, Orvit Clinic, Torun, Poland 4Division of Radiology, Dr Blazek’s District Hospital, Inowroclaw, Poland 5Department of Clinical Pathomorphology, University Hospital No. 1, Bydgoszcz, Poland [Received: 5 November 2017; Accepted: 5 January 2018] Tendons are connective tissue structures of paramount importance to human ability of locomotion. The understanding of their physiology and pathology is gaining importance as advances in regenerative medicine are being made today. So far, very few studies were conducted to extend the knowledge about pathology, healing response and management of tendon lesions. In this paper we summarise actual knowledge on structure, process of healing and ageing of the tendons. The structure of tendon is optimised for the best performance of the tissue. Despite the simplicity of the healing response, nume- rous studies showed that the problems with full recovery are common and much more significant than we thought; that is why we discussed the issue of immo- bilisation and mechanical stimulation during healing process. The phenomenon of tendons’ ageing is poorly understood. Although it seems to be a natural and painless process, it is completely different from degeneration in tendinopathy.