REVIEW ARTICLE Osteoarthritis of the Wrist
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Wrist Fracture – Advice Following Removal of Your Cast
Wrist Fracture – advice following removal of your cast A plaster cast usually prevents a fracture from moving, but allows your fingers to move. The cast also reduces pain. What to expect It usually takes four to six weeks for new bone to form to heal your fracture. When the cast is removed most people find that their wrist is stiff, weak and uncomfortable to start with. It may also be prone to swelling and the skin dry or flaky, this is quite normal. It is normal to get some pain after your fracture. If you need painkillers you should take them as prescribed as this will allow you to do your exercises and use your wrist for light activities. You can ask a Pharmacist about over the counter painkillers. If your pain is severe, continuous or excessive you should contact your GP. The new bone gradually matures and becomes stronger over the next few months. It is likely to be tender and may hurt if you bang it. The muscles will be weak initially, but they should gradually build up as you start to use your hand and wrist. When can I start to use my hand and wrist? It is important to try and use your hand and wrist as normally as possible. Start with light activities like fastening buttons, washing your face, eating, turning the pages of books over etc. Build up as pain allows. Avoid lifting a kettle for 4 weeks If I have been given a Wrist splint You may have been given a wrist splint to wear. -

2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4Th SESSION 1
2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4th SESSION 1: Carpal Ligament 1 Stable Central Column Theory of Carpal Mechanics Michael Sandow FRACS Wakefield Orthopaedic Clinic Adelaide, Australia Background: The carpus is a complicated and functionally challenged mechanical system and advancements in the understanding have been compromised by the recognition that there is no standard carpal mechanical system and no typical wrist. This paper cover component of a larger project that seeks to develop a kinetic model of wrist mechanics to allow reverse analysis of the specific biomechanical controls or rule of a specific patient's carpus, and then use those to create a forward mathematical model to reproduce the unique individual's anatomical motion based on the extracted rules. Objectives and Methods: Based on previous observations, the carpus essentially moves with only 2 degrees of freedom - pitch (flexion / extension) and yaw (radial deviation / ulnar deviation), while largely preventing roll (pronation / supination). The object of this paper is therefore to present the background and justification to support the rules based motion (RBM) concept states that the motion of a mechanical system, such as the wrist, is the net interplay of 4 rules - morphology, constraint, interaction and load. The Stable Central Column Theory (SCCT) of wrist mechanics applies the concept of RBM to the carpus, and by using a reverse engineering computational analysis model, identified a consistent pattern of isometric constraints, creating a "Two-Gear Four-Bar" linkage. This study assessed the motion of the carpus using a 3D dynamic visualization model, and the hypothesis was that the pattern and direction of motion of the proximal row, and the distal row with respect the immediately cephalad carpal bones or radius would be very similar in all directions of wrist motion. -

Study Guide Medical Terminology by Thea Liza Batan About the Author
Study Guide Medical Terminology By Thea Liza Batan About the Author Thea Liza Batan earned a Master of Science in Nursing Administration in 2007 from Xavier University in Cincinnati, Ohio. She has worked as a staff nurse, nurse instructor, and level department head. She currently works as a simulation coordinator and a free- lance writer specializing in nursing and healthcare. All terms mentioned in this text that are known to be trademarks or service marks have been appropriately capitalized. Use of a term in this text shouldn’t be regarded as affecting the validity of any trademark or service mark. Copyright © 2017 by Penn Foster, Inc. All rights reserved. No part of the material protected by this copyright may be reproduced or utilized in any form or by any means, electronic or mechanical, including photocopying, recording, or by any information storage and retrieval system, without permission in writing from the copyright owner. Requests for permission to make copies of any part of the work should be mailed to Copyright Permissions, Penn Foster, 925 Oak Street, Scranton, Pennsylvania 18515. Printed in the United States of America CONTENTS INSTRUCTIONS 1 READING ASSIGNMENTS 3 LESSON 1: THE FUNDAMENTALS OF MEDICAL TERMINOLOGY 5 LESSON 2: DIAGNOSIS, INTERVENTION, AND HUMAN BODY TERMS 28 LESSON 3: MUSCULOSKELETAL, CIRCULATORY, AND RESPIRATORY SYSTEM TERMS 44 LESSON 4: DIGESTIVE, URINARY, AND REPRODUCTIVE SYSTEM TERMS 69 LESSON 5: INTEGUMENTARY, NERVOUS, AND ENDOCRINE S YSTEM TERMS 96 SELF-CHECK ANSWERS 134 © PENN FOSTER, INC. 2017 MEDICAL TERMINOLOGY PAGE III Contents INSTRUCTIONS INTRODUCTION Welcome to your course on medical terminology. You’re taking this course because you’re most likely interested in pursuing a health and science career, which entails proficiencyincommunicatingwithhealthcareprofessionalssuchasphysicians,nurses, or dentists. -

PE1897 Wrist and Hand Stretches
Patient and Family Education Wrist and Hand Stretches How can I help my child do the stretches? Use these exercises to help stretch the You play an important role in your child’s therapy. Older children may need wrist and hand. reminders to do their stretches every day. You may need to help position your younger child for the stretches. Or you may need to help stretch your child’s hand or arm. Be sure to pay attention to your child’s alignment and posture to make sure each stretch is performed correctly. How often should my child do the stretches? These stretches should be done twice a day, or as instructed by your therapist: ______________________________________________________________ Stretches Wrist extension Hold arm out in front Use opposite hand to bend wrist up with fingers straight Option to straighten elbow for increased stretch Hold for 30 seconds or _______ Repeat 2 times or ___________ VHI Wrist extension Sit with elbows on table Place palms together Slowly lower wrists to table Hold for 30 seconds or ______ Repeat 2 times or __________ VHI Wrist flexion Hold arm out in front Use opposite hand to bend wrist down Option to straighten elbow for increased stretch Option to curl fingers for increased stretch Hold for 30 seconds or ______ VHI Repeat 2 times or __________ 1 of 2 Wrist and Hand Stretches Wrist radial/ulnar deviation To Learn More Hold arm at side of body with palm • Occupational/Physical facing forward Therapy 206-987-2113 Use opposite hand to straighten wrist toward the thumb side Do not allow the wrist to flex forward to extend backward Free Interpreter Hold for 30 seconds or ______ Services Repeat 2 times or __________ • In the hospital, ask BioEx Systems Inc.* your child’s nurse. -

Upper Extremity Injuries in Pediatric Athletes
Review Article Page 1 of 10 Upper extremity injuries in pediatric athletes Kristen M. Sochol, Daniel A. Charen, Jaehon Kim Department of Orthopedics at Mount Sinai Hospital, New York, NY, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: All authors; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final approval of manuscript: All authors. Correspondence to: Kristen M. Sochol, MD. Department of Orthopedics at Mount Sinai Hospital, 5E 98th St, New York, NY 10029, USA. Email: [email protected]. Abstract: Upper extremity injuries in the pediatric patient are common, but are often more difficult to diagnose compared to their adult counterparts due to the gradual progression of cartilage ossification. Common pediatric upper extremity injuries include fractures and soft tissue trauma. Less prevalent injuries include sport specific overuse injuries. Fractures in the pediatric population are best described using the Salter-Harris classification, which has management and prognostic implications. Most pediatric upper extremity injuries can be managed with an initial trial of immobilization and early range of motion, followed by surgical intervention if necessary. Children have a robust healing response to bony and soft tissue injuries, and have good outcomes with appropriate management. Keywords: Pediatric athletes; upper extremity; Salter-Harris; overuse; injury Received: 14 February 2018; Accepted: 08 May 2018; Published: 15 May 2018. doi: 10.21037/aoj.2018.05.04 View this article at: http://dx.doi.org/10.21037/aoj.2018.05.04 Introduction joints are constrained by a network of ligaments that are primarily named after their attachment sites. -

Hand, Elbow, Wrist Pain
Physical and Sports Therapy Hand, Elbow, Wrist Pain The hand is a wondrously complex structure of tiny bones, muscles, ligaments, and tendons which work together to perform tasks. The wrist and elbow are stabilizing joints that support the steady use of the hand and provide attachment points for the muscles that control the hand and wrist. All three of these areas are prone to injury from overuse or trauma. Their complexity requires the skills of an expert for proper rehabilitation from injury. Some Hand, Wrist, and Elbow Issues Include: Tennis/Golfer’s Elbow: Tendonitis, or inflammation of the tendons, at the muscular attachments near the elbow. Symptoms typically include tenderness on the sides of the elbow, which increase with use of the wrist and hand, such as shaking hands or picking up a gallon of milk. Tendonitis responds well to therapy, using eccentric exercise, stretching, and various manual therapy techniques. Carpal Tunnel Syndrome: Compression of the Median Nerve at the hand/base of your wrist. Symptoms include pain, numbness, and tingling of the first three fingers. The condition is well-known for waking people at night. Research supports the use of therapy, particularly in the early phase, for alleviation of the compression through stretching and activity modification. Research indicates that the longer symptoms are present before initiating treatment, the worse the outcome for therapy and surgical intervention due to underlying physiological changes of the nerve. What can Physical or Occupational therapy do for Hand, Wrist, or Elbow pain? Hand, wrist, and elbow injuries are commonly caused by trauma, such as a fall or overuse. -

Wrist and Hand Examina[On
Wrist and Hand Examinaon Daniel Lueders, MD Assistant Professor Physical Medicine and Rehabilitaon Objecves • Understand the osseous, ligamentous, tendinous, and neural anatomy of the wrist and hand • Outline palpable superficial landmarks in the wrist and hand • Outline evaluaon of and differen.aon between nerves to the wrist and hand • Describe special tes.ng of wrist and hand Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Wrist Anatomy • Radius • Ulna • Carpal bones Inspec.on • Ecchymosis • Erythema • Deformity • Laceraon Inspec.on • Common Finger Deformies • Swan Neck Deformity • Boutonniere Deformity • Hypertrophic nodules • Heberden’s, Bouchard’s Inspec.on • Swan Neck Deformity • PIP hyperextension, DIP flexion • Pathology is at PIP joint • Insufficiency of volar/palmar plate and suppor.ng structures • Distally, the FDP tendon .ghtens from PIP extension causing secondary DIP flexion • Alternavely, extensor tendon rupture produces similar deformity Inspec.on • Boutonniere Deformity • PIP flexion, DIP hyperextension • Pathology is at PIP joint • Commonly occurs from insufficiency of dorsal and lateral suppor.ng structures at PIP joint • Lateral bands migrate volar/palmar, creang increased flexion moment • Results in PIP “buTon hole” effect dorsally Inspec.on • Nodules • Osteoarthri.c • Hypertrophic changes of OA • PIP - Bouchard’s nodule • DIP - Heberden’s nodule • Rheumatoid Arthri.s • MCP joints affected most • Distal radioulnar joint can also be affected -
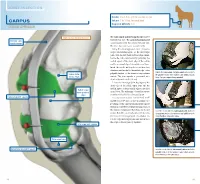
Carpus Volume: 7 to 10 Ml for Each Joint Degree of Difficulty: 1/3 Dorsal Approach
JOINT INJECTION needle: 1 to 1.5 in. (2.5 to 3.8 cm), 20 ga Carpus volume: 7 to 10 ml for each joint Degree of difficulty: 1/3 Dorsal approach right carpus, dorsomedial view The radiocarpal and intercarpal joints can be extensor carpi entered with ease. The carpometacarpal joint radialis tendon communicates with the intercarpal joint and, therefore, does not require separate entry. Using the dorsal approach, enter the radio- carpal (antebrachiocarpal) or the intercarpal joints with the limb held and the carpus flexed. Locate the radiocarpal joint by palpating the medial aspect of the distal edge of the radius and the proximal edge of the radial carpal bone. Insert the needle midway between these two structures and medial to the medial edge of the palpate the radiocarpal and intercarpal joints medial to palpable tendon of the extensor carpi radialis radius (distal the palpable tendon of the extensor carpi radialis muscle. medial edge) muscle. The joint capsule is penetrated at a Note: The right carpus is being palpated. depth of about 0.5 inch (1.3 cm). Locate the intercarpal joint by palpating the distal edge of the radial carpal bone and the medial aspect of the proximal edge of the third radial carpal bone (proximal carpal bone. The technique of needle insertion edge) is similar to that for the radiocarpal joint. radiocarpal joint capsule It is important to point out that Ford et al47 and Moyer et al48 showed that the palmar out- pouchings of the carpometacarpal joint capsule extend into the fibers of the proximal portion of the suspensory ligament. -

Readingsample
Color Atlas of Human Anatomy Vol. 1: Locomotor System Bearbeitet von Werner Platzer 6. durchges. Auflage 2008. Buch. ca. 480 S. ISBN 978 3 13 533306 9 Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 130 Upper Limb: Bones, Ligaments, Joints Radiocarpal and Midcarpal Joints Ligaments in the Region of the Wrist (A–E) (A–E) Four groups of ligaments can be distin- The radiocarpal or wrist joint is an ellip- guished: soid joint formed on one side by the radius (1) and the articular disk (2) and on the Ligaments which unite the forearm bones with other by the proximal row of carpal bones.Not the carpal bones (violet). These include the all the carpal bones of the proximal row are ulnar collateral ligament (8), the radial col- in continual contact with the socket- lateral ligament (9), the palmar radiocarpal shaped articular facet of the radius and the ligament (10), the dorsal radiocarpal liga- disk. The triquetrum (3), only makes close ment (11), and the palmar ulnocarpal liga- contact with the disk during ulnar abduc- ment (12). tion and loses contact on radial abduction. Ligaments which unite the carpal bones with The capsule of the wrist joint is lax, dorsally one another,orintercarpal ligaments (red). These comprise the radiate carpal ligament Upper Limb relatively thin, and is reinforced by numer- ous ligaments. -

Bones and Joints of the Upper Limb: Forearm and Hand
Unit 4: Bones and joints of the upper limb: forearm and hand Chapter 6 (Upper limb) GENERAL OBJECTIVES: - recognize, name and correctly orient forearm and hand bones - understand movements in elbow, wrist and hand joints SPECIFIC OBJECTIVES: Bones of the forearm and hand Identify the bony features on each part of the following bones: RADIUS - Upper End - Shaft - Lower End ULNA - Upper End - Shaft - Lower End Deduce (from the shape of the articular surfaces) the movements at (i) the elbow joint and (ii) the radioulnar joints. Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Identify the following bones CARPALS - Proximal Row - Distal Row METACARPALS PHALANGES Identify the attachments of the Flexor Retinaculum and define the "Carpal Tunnel". Deduce (from the shape of the articular surfaces) the movements at (i) the wrist joint (ii) the carpometacarpal joint of the thumb (iii) metacarpophalangeal joints (iv) interphalangeal joints Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Joints of the forearm and hand Elbow Joint Articular Surfaces (Humeroulnar & Humeroradial) Fibrous Capsule & Joint Cavity Synovial Membrane Collateral Ligaments ( Medial & Lateral) Special Structures: Olecranon Bursa Other Bursae, Pads of Fat Movements at the Elbow Joint: Flexion/Extension Stability Carrying Angle Radioulnar Joints Proximal Radioulnar Joint Annular Ligament Distal Radioulnar -

Trapezius Origin: Occipital Bone, Ligamentum Nuchae & Spinous Processes of Thoracic Vertebrae Insertion: Clavicle and Scapul
Origin: occipital bone, ligamentum nuchae & spinous processes of thoracic vertebrae Insertion: clavicle and scapula (acromion Trapezius and scapular spine) Action: elevate, retract, depress, or rotate scapula upward and/or elevate clavicle; extend neck Origin: spinous process of vertebrae C7-T1 Rhomboideus Insertion: vertebral border of scapula Minor Action: adducts & performs downward rotation of scapula Origin: spinous process of superior thoracic vertebrae Rhomboideus Insertion: vertebral border of scapula from Major spine to inferior angle Action: adducts and downward rotation of scapula Origin: transverse precesses of C1-C4 vertebrae Levator Scapulae Insertion: vertebral border of scapula near superior angle Action: elevates scapula Origin: anterior and superior margins of ribs 1-8 or 1-9 Insertion: anterior surface of vertebral Serratus Anterior border of scapula Action: protracts shoulder: rotates scapula so glenoid cavity moves upward rotation Origin: anterior surfaces and superior margins of ribs 3-5 Insertion: coracoid process of scapula Pectoralis Minor Action: depresses & protracts shoulder, rotates scapula (glenoid cavity rotates downward), elevates ribs Origin: supraspinous fossa of scapula Supraspinatus Insertion: greater tuberacle of humerus Action: abduction at the shoulder Origin: infraspinous fossa of scapula Infraspinatus Insertion: greater tubercle of humerus Action: lateral rotation at shoulder Origin: clavicle and scapula (acromion and adjacent scapular spine) Insertion: deltoid tuberosity of humerus Deltoid Action: -

Anatomy and Physiology II
Anatomy and Physiology II Review Bones of the Upper Extremities Muscles of the Upper Extremities Anatomy and Physiology II Review Bones of the Upper Extremities Questions From Shoulder Girdle Lecture • Can you name the following structures? A – F • Acromion F – B B • Spine of the Scapula G – C • Medial (Vertebral) Border H – E C • Lateral (Axillary) Border – A • Superior Angle E I – D • Inferior Angle – G • Head of the Humerus D – H • Greater Tubercle of Humerus – I • Deltoid Tuberosity Questions From Shoulder Girdle Lecture • Would you be able to find the many of the same landmarks on this view (angles, borders, etc)? A • Can you name the following? – D • Coracoid process of scapula C – C D B • Lesser Tubercle – A • Greater Tubercle – B • Bicipital Groove (Intertubercular groove) Questions From Upper Extremities Lecture • Can you name the following structures? – B • Lateral epicondyle – A • Medial epicondyle A B Questions From Upper Extremities Lecture • Can you name the following landmarks? – C • Olecranon process – A • Head of the radius – B D • Medial epicondyle B A – D C • Lateral epicondyle Questions From Upper Extremities Lecture • Can you name the following bones and landmarks? – Which bone is A pointing to? • Ulna – Which bone is B pointing A to? • Radius E – C B • Styloid process of the ulna – D • Styloid process of the radius C – E D • Interosseous membrane of forearm Questions From Upper Extremities Lecture • Can you name the following bony landmarks? – Which landmark is A pointing to? • Lateral epicondyle of humerus – Which