Ligaments and Joints of the Upper Limb
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Considered a Bone of Both Shoulder Girdle and Shoulder Joint. the Shoulder Girdle Is Comprised of the Clavicle and the Scapula
Considered a bone of both shoulder girdle and shoulder joint. The shoulder girdle is comprised of the clavicle and the scapula. The shoulder joint consists of the scapula and the humerus. The primary function of the shoulder girdle is to position itself to accommodate movements of the shoulder joint. 1 Superior angle—top point Inferior angle—bottom point Vertebral border—side closest to vertebral column Axillary border—side closest to arm Subscapular fossa—anterior fossa Glenoid fossa, glenoid labrum, glenoid cavity --The glenoid fossa is the shallow cavity where the humeral head goes. The glenoid labrum is the cartilage that goes around the glenoid fossa. So the glenoid fossa and glenoid labrum together comprise the glenoid cavity. Supraspinous fossa—posterior, fossa above the spine Spine of the scapula—the back projection Infraspinous fossa—posterior depression/fossa below spine Coracoid process—anterior projection head Acromion process—posterior projection head above spine 2 Scapulothoracic “joint” = NOT a true joint; there are no ligaments or articular capsule. The scapula just rests on the muscle over top the rib cage, which allows for passive movements. Sternoclavicular joint=where the clavicle (collarbone) and the sternum (breastbone) articulate; movement is slight in all directions and of a gliding, rotational type Acromioclavicular joint = where the clavicle and scapula (acromion process) articulate; AKA: AC Joint; movement is a slight gliding when elevation and depression take place. Glenohumeral joint = the shoulder joint 3 4 All 3 true joints: Sternoclavicular, AC and glenohumeral (GH) all work together to move arm in all directions. The GH allows the arm to go out to the side and be abducted, then the AC and Sternoclavicular joints kick in to allow the arm to go above shoulder level by allowing the shoulderblade to move up to increase the range of motion (ROM). -

2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4Th SESSION 1
2019 IWIW Meeting Abstracts, Las Vegas, Wed. Sept. 4th SESSION 1: Carpal Ligament 1 Stable Central Column Theory of Carpal Mechanics Michael Sandow FRACS Wakefield Orthopaedic Clinic Adelaide, Australia Background: The carpus is a complicated and functionally challenged mechanical system and advancements in the understanding have been compromised by the recognition that there is no standard carpal mechanical system and no typical wrist. This paper cover component of a larger project that seeks to develop a kinetic model of wrist mechanics to allow reverse analysis of the specific biomechanical controls or rule of a specific patient's carpus, and then use those to create a forward mathematical model to reproduce the unique individual's anatomical motion based on the extracted rules. Objectives and Methods: Based on previous observations, the carpus essentially moves with only 2 degrees of freedom - pitch (flexion / extension) and yaw (radial deviation / ulnar deviation), while largely preventing roll (pronation / supination). The object of this paper is therefore to present the background and justification to support the rules based motion (RBM) concept states that the motion of a mechanical system, such as the wrist, is the net interplay of 4 rules - morphology, constraint, interaction and load. The Stable Central Column Theory (SCCT) of wrist mechanics applies the concept of RBM to the carpus, and by using a reverse engineering computational analysis model, identified a consistent pattern of isometric constraints, creating a "Two-Gear Four-Bar" linkage. This study assessed the motion of the carpus using a 3D dynamic visualization model, and the hypothesis was that the pattern and direction of motion of the proximal row, and the distal row with respect the immediately cephalad carpal bones or radius would be very similar in all directions of wrist motion. -

THE STUDY of CORACOACROMIAL LIGAMENT MORPHOLOGY and ITS CLINICAL ASPECTS Sowmya S *1, Sharmada Kl 2, Meenakshi Parthasarathy 3
International Journal of Anatomy and Research, Int J Anat Res 2020, Vol 8(1.2):7342-45. ISSN 2321-4287 Original Research Article DOI: https://dx.doi.org/10.16965/ijar.2019.377 THE STUDY OF CORACOACROMIAL LIGAMENT MORPHOLOGY AND ITS CLINICAL ASPECTS Sowmya S *1, Sharmada Kl 2, Meenakshi Parthasarathy 3. *1 Associate professor, Dept of Anatomy, Bowring & Lady Curzon Medical College & Research Institute, Karnataka, India, [email protected] 2 Tutor, Dept of Anatomy, Bowring & Lady Curzon Medical College & Research Institute, Karnataka, India, [email protected] 3 Professor, Dept of Anatomy, Bowring & Lady Curzon Medical College & Research Institute, Karnataka, India, [email protected] ABSTRACT Background: The coracoacromial ligament (CAL) as an integral component of the coracoacromial arch, plays an important role in shoulder biomechanics, joint stability, and proprioception thus maintains static restraint due to its dynamic interactions with ligaments, muscles and bony elements around the shoulder joint. Age-dependent changes due to chronic stress and cellular degradation cause thickening and stiffening of the CAL that may contribute to a spectrum of shoulder pathology from capsular tightness to rotator cuff tear arthropathy and impingement syndrome. Objectives: This study conducted to observe the different types of CAL and its relationship with coracoacromial veil. Materials and Methods: The study conducted on 50 upper limbs at Bowring & Lady Curzon medical college & research institute and Bangalore medical college & research institute. The upper limbs were dissected at the shoulder joint complex and acromion process and coracoid process were appreciated and coracoacromial ligaments were appreciated for their types and morphometry. Results and Conclusion: Four types of CAL were observed in this study. -
Mobilization for the Neurologically Involved Child
MOBILIZATION FOR THE NEUROLOGICALLY INVOLVED CHILD Assessment and Application Strategies For Pediatric PTs and OTs Sandy Brooks-Scott M.S., PPT, PCS www.clinicians-view.com Chapter I Pathology and Resultant Immobility Mobility is a worthy goal. However, before it can be achieved in a child with neurological dysfunction, certain prerequisites must be in place: normal bony alignment; normal muscle strength, flexibility and endurance; a coordinating nervous system; an efficient cardiorespi ratory system; and normal connective tissue flexibility. Immobility after initial neurological insult affects all these systems, making assessment and treatment of all systems interfering with efficient mobility a paramount goal of the therapist. Neurological Damage-Original Insult The motor result of the neurological insult is dependent upon the age, the location, and the extent of the insult (Brann 1988; Costello et al. 1988; Nelson 1988; Pape and Wigglesworth 1979). The most widely discussed reason for brain damage in the pre-, peri- or initial postnatal stages is a change in blood pressure, causing the vessels in the developing organ to hemorrhage or become ischemic (Pape and Wigglesworth 1979). Nelson (1988) notes that most infants who live through severe asphyxia at birth do not develop cerebral palsy or mental retardation. Brann (1988), in his discussion of the effects of acute total and prolonged partial asphyxia, clearly demonstrates that the neurological changes and motor outcomes vary depending on the acuteness, duration, and severity of the asphyxia. Because a child will not have autoregulatory mechanisms to control blood pressure until 3 months of age, excessive heat loss, abnormal partial pressures of oxygen and carbon dioxide, or fluid imbalances can affect a newborn's blood pressure, producing ischemic hypoxia and neural damage. -
Skeleton of the Upper Limb
SKELETON OF THE UPPER LIMB L E C T U R E 2 D E N T I S T R Y 2016 RNDR. MICHAELA RAČANSKÁ, PH.D. Skeleton of the upper limb (ossa membri superioris) Thirty-four bones form the skeletal framework of each upper limb I. Shoulder girdle (cingulum membri superioris) Collar bone, clavicle – clavicula Shoulder blade – scapula II. Bones of free part of the upper limb (ossa membri superioris liberi) Arm bone – humerus Radius – radius Ulna – ulna Carpal bones – ossa carpi 8 Metacarpal bones – ossa metacarpi 5 Phalanges, hand digits – ossa digitorum manus 14 Sesamoid - 2 Clavicula (collar bone) Connects upper limb with the trunk Connection with the shoulder blade Connection with the breast bone Clavicula (collar bone) Medial end (sternal end) extremitas sternalis (facies articularis sternalis) sternal articular facet tuberositas costalis Costal tuberosity (impressio ligamenti costoclavicularis) (impression for costoclavicular ligament) Lateral (acromial) end extremitas acromialis (facies articularis acromialis) tuberositas coracoidea (tuberculum conoideum et linea trapezoidea) conoid tubercle + trapezoid line Side orientation Left one –superior view Left one –inferior view Fracture of the collar bone X-ray of a left clavicle fracture https://en.wikipedia.org/wiki/Clavicle_fracture Scapula Connection to humerus, clavicle Margo: superior medialis lateralis angulus: superior, inferior, lateralis facies: costalis, dorsalis Facies costalis scapulae Lineae musculares (transverae) Fossa subscapularis Incisura scapulae (ligamentum transversum scapulae) Processus -

REVIEW ARTICLE Osteoarthritis of the Wrist
REVIEW ARTICLE Osteoarthritis of the Wrist Krista E. Weiss, Craig M. Rodner, MD From Harvard College, Cambridge, MA and Department of Orthopaedic Surgery, University of Connecticut Health Center, Farmington, CT. Osteoarthritis of the wrist is one of the most common conditions encountered by hand surgeons. It may result from a nonunited or malunited fracture of the scaphoid or distal radius; disruption of the intercarpal, radiocarpal, radioulnar, or ulnocarpal ligaments; avascular necrosis of the carpus; or a developmental abnormality. Whatever the cause, subsequent abnormal joint loading produces a spectrum of symptoms, from mild swelling to considerable pain and limitations of motion as the involved joints degenerate. A meticulous clinical and radiographic evaluation is required so that the pain-generating articulation(s) can be identi- fied and eliminated. This article reviews common causes of wrist osteoarthritis and their surgical treatment alternatives. (J Hand Surg 2007;32A:725–746. Copyright © 2007 by the American Society for Surgery of the Hand.) Key words: Wrist, osteoarthritis, arthrodesis, carpectomy, SLAC. here are several different causes, both idio- of events is analogous to SLAC wrist and has pathic and traumatic, of wrist osteoarthritis. been termed scaphoid nonunion advanced collapse Untreated cases of idiopathic carpal avascular (SNAC). Wrist osteoarthritis can also occur second- T 1 2 necrosis, as in Kienböck’s or Preiser’s disease, may ary to an intra-articular fracture of the distal radius or result in radiocarpal arthritis. Congenital wrist abnor- ulna or from an extra-articular fracture resulting in malities, such as Madelung’s deformity,3,4 can lead malunion and abnormal joint loading. -

Sternoclavicular Joint Allograft Reconstruction Using the Sternal Docking Technique
JSES Open Access 2 (2018) 190−193 Contents lists available at ScienceDirect JSES Open Access journal homepage: www.elsevier.com/locate/jses Sternoclavicular joint allograft reconstruction using the sternal docking technique JoaquinD1XX Sanchez-SoteloD2X*X, YaserD3XX Baghdadi,D4XXNgocD5XX Tram V. NguyenD6XX Department of Orthopedic Surgery, Mayo Clinic, Rochester, MN, USA ARTICLE INFO Background: The sternoclavicular joint may become unstable as a result of trauma or medial clavicle resec- tion for arthritis. Allograft reconstruction with the figure-of-8 configuration is commonly used. This study Keywords: was conducted to determine the outcome of sternoclavicular joint reconstruction using an alternative graft Sternoclavicular joint configuration. instability Methods: Between 2005 and 2013, 19 sternoclavicular joint reconstructions were performed using a semite- semitendinous allograft ndinous allograft in a sternal docking configuration. The median age at surgery was 44 years (range, 15-79 allograft reconstruction years). Indications included instability in 16 (anterior, 13; posterior, 3) or medial clavicle resection for osteo- clavicle arthritis in 3. The median follow-up time was 3 years (range, 1-9 years). sternoclavicular docking technique Results: Two reconstructions (10.5%) underwent revision surgery, 1 additional patient had occasional subjec- tive instability, and the remaining 16 (84%) were considered stable. Sternoclavicular joint reconstruction led Level of evidence: Level IV, Case Series, < Treatment Study to improved pain (visual analog scale for pain subsided from 5 to 1 point, P .01), with pain being rated as mild or none for 15 shoulders. At the most recent follow-up, the median 11-item version of the Disabilities of the Arm, Shoulder and Hand and American Shoulder and Elbow Surgeons scores were 11 (interquartile range [IQR], 0-41) and 88 (IQR, 62-100) respectively. -
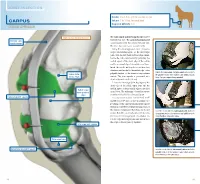
Carpus Volume: 7 to 10 Ml for Each Joint Degree of Difficulty: 1/3 Dorsal Approach
JOINT INJECTION needle: 1 to 1.5 in. (2.5 to 3.8 cm), 20 ga Carpus volume: 7 to 10 ml for each joint Degree of difficulty: 1/3 Dorsal approach right carpus, dorsomedial view The radiocarpal and intercarpal joints can be extensor carpi entered with ease. The carpometacarpal joint radialis tendon communicates with the intercarpal joint and, therefore, does not require separate entry. Using the dorsal approach, enter the radio- carpal (antebrachiocarpal) or the intercarpal joints with the limb held and the carpus flexed. Locate the radiocarpal joint by palpating the medial aspect of the distal edge of the radius and the proximal edge of the radial carpal bone. Insert the needle midway between these two structures and medial to the medial edge of the palpate the radiocarpal and intercarpal joints medial to palpable tendon of the extensor carpi radialis radius (distal the palpable tendon of the extensor carpi radialis muscle. medial edge) muscle. The joint capsule is penetrated at a Note: The right carpus is being palpated. depth of about 0.5 inch (1.3 cm). Locate the intercarpal joint by palpating the distal edge of the radial carpal bone and the medial aspect of the proximal edge of the third radial carpal bone (proximal carpal bone. The technique of needle insertion edge) is similar to that for the radiocarpal joint. radiocarpal joint capsule It is important to point out that Ford et al47 and Moyer et al48 showed that the palmar out- pouchings of the carpometacarpal joint capsule extend into the fibers of the proximal portion of the suspensory ligament. -

Subacromial Decompression in the Shoulder
Subacromial Decompression Geoffrey S. Van Thiel, Matthew T. Provencher, Shane J. Nho, and Anthony A. Romeo PROCEDURE 2 22 Indications P ITFALLS ■ Impingement symptoms refractory to at least • There are numerous possible 3 months of nonoperative management causes of shoulder pain that can ■ In conjunction with arthroscopic treatment of a mimic impingement symptoms. All potential causes should be rotator cuff tear thoroughly evaluated prior to ■ Relative indication: type II or III acromion with undertaking operative treatment clinical fi ndings of impingement of isolated impingement syndrome. Examination/Imaging Subacromial Decompression PHYSICAL EXAMINATION ■ Assess the patient for Controversies • Complete shoulder examination with range of • Subacromial decompression in motion and strength the treatment of rotator cuff • Tenderness with palpation over anterolateral pathology has been continually acromion and supraspinatus debated. Prospective studies • Classic Neer sign with anterolateral shoulder have suggested that there is no difference in outcomes with and pain on forward elevation above 90° when without subacromial the greater tuberosity impacts the anterior decompression. acromion (and made worse with internal rotation) • Subacromial decompression • Positive Hawkins sign: pain with internal rotation, performed in association with a forward elevation to 90°, and adduction, which superior labrum anterior- causes impingement against the coracoacromial posterior (SLAP) repair can potentially increase ligament postoperative stiffness. ■ The impingement test is positive if the patient experiences pain relief with a subacromial injection of lidocaine. ■ Be certain to evaluate for acromioclavicular (AC) joint pathology, and keep in mind that there are several causes of shoulder pain that can mimic impingement syndrome. P ITFALLS IMAGING • Ensure that an axillary lateral ■ Standard radiographs should be ordered, view is obtained to rule out an os acromiale. -

Readingsample
Color Atlas of Human Anatomy Vol. 1: Locomotor System Bearbeitet von Werner Platzer 6. durchges. Auflage 2008. Buch. ca. 480 S. ISBN 978 3 13 533306 9 Zu Inhaltsverzeichnis schnell und portofrei erhältlich bei Die Online-Fachbuchhandlung beck-shop.de ist spezialisiert auf Fachbücher, insbesondere Recht, Steuern und Wirtschaft. Im Sortiment finden Sie alle Medien (Bücher, Zeitschriften, CDs, eBooks, etc.) aller Verlage. Ergänzt wird das Programm durch Services wie Neuerscheinungsdienst oder Zusammenstellungen von Büchern zu Sonderpreisen. Der Shop führt mehr als 8 Millionen Produkte. 130 Upper Limb: Bones, Ligaments, Joints Radiocarpal and Midcarpal Joints Ligaments in the Region of the Wrist (A–E) (A–E) Four groups of ligaments can be distin- The radiocarpal or wrist joint is an ellip- guished: soid joint formed on one side by the radius (1) and the articular disk (2) and on the Ligaments which unite the forearm bones with other by the proximal row of carpal bones.Not the carpal bones (violet). These include the all the carpal bones of the proximal row are ulnar collateral ligament (8), the radial col- in continual contact with the socket- lateral ligament (9), the palmar radiocarpal shaped articular facet of the radius and the ligament (10), the dorsal radiocarpal liga- disk. The triquetrum (3), only makes close ment (11), and the palmar ulnocarpal liga- contact with the disk during ulnar abduc- ment (12). tion and loses contact on radial abduction. Ligaments which unite the carpal bones with The capsule of the wrist joint is lax, dorsally one another,orintercarpal ligaments (red). These comprise the radiate carpal ligament Upper Limb relatively thin, and is reinforced by numer- ous ligaments. -

Bone Limb Upper
Shoulder Pectoral girdle (shoulder girdle) Scapula Acromioclavicular joint proximal end of Humerus Clavicle Sternoclavicular joint Bone: Upper limb - 1 Scapula Coracoid proc. 3 angles Superior Inferior Lateral 3 borders Lateral angle Medial Lateral Superior 2 surfaces 3 processes Posterior view: Acromion Right Scapula Spine Coracoid Bone: Upper limb - 2 Scapula 2 surfaces: Costal (Anterior), Posterior Posterior view: Costal (Anterior) view: Right Scapula Right Scapula Bone: Upper limb - 3 Scapula Glenoid cavity: Glenohumeral joint Lateral view: Infraglenoid tubercle Right Scapula Supraglenoid tubercle posterior anterior Bone: Upper limb - 4 Scapula Supraglenoid tubercle: long head of biceps Anterior view: brachii Right Scapula Bone: Upper limb - 5 Scapula Infraglenoid tubercle: long head of triceps brachii Anterior view: Right Scapula (with biceps brachii removed) Bone: Upper limb - 6 Posterior surface of Scapula, Right Acromion; Spine; Spinoglenoid notch Suprspinatous fossa, Infraspinatous fossa Bone: Upper limb - 7 Costal (Anterior) surface of Scapula, Right Subscapular fossa: Shallow concave surface for subscapularis Bone: Upper limb - 8 Superior border Coracoid process Suprascapular notch Suprascapular nerve Posterior view: Right Scapula Bone: Upper limb - 9 Acromial Clavicle end Sternal end S-shaped Acromial end: smaller, oval facet Sternal end: larger,quadrangular facet, with manubrium, 1st rib Conoid tubercle Trapezoid line Right Clavicle Bone: Upper limb - 10 Clavicle Conoid tubercle: inferior -

Bones and Joints of the Upper Limb: Forearm and Hand
Unit 4: Bones and joints of the upper limb: forearm and hand Chapter 6 (Upper limb) GENERAL OBJECTIVES: - recognize, name and correctly orient forearm and hand bones - understand movements in elbow, wrist and hand joints SPECIFIC OBJECTIVES: Bones of the forearm and hand Identify the bony features on each part of the following bones: RADIUS - Upper End - Shaft - Lower End ULNA - Upper End - Shaft - Lower End Deduce (from the shape of the articular surfaces) the movements at (i) the elbow joint and (ii) the radioulnar joints. Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Identify the following bones CARPALS - Proximal Row - Distal Row METACARPALS PHALANGES Identify the attachments of the Flexor Retinaculum and define the "Carpal Tunnel". Deduce (from the shape of the articular surfaces) the movements at (i) the wrist joint (ii) the carpometacarpal joint of the thumb (iii) metacarpophalangeal joints (iv) interphalangeal joints Indicate the bony attachments of the major ligaments which help to maintain the stability of these joints (while allowing their mobility). Joints of the forearm and hand Elbow Joint Articular Surfaces (Humeroulnar & Humeroradial) Fibrous Capsule & Joint Cavity Synovial Membrane Collateral Ligaments ( Medial & Lateral) Special Structures: Olecranon Bursa Other Bursae, Pads of Fat Movements at the Elbow Joint: Flexion/Extension Stability Carrying Angle Radioulnar Joints Proximal Radioulnar Joint Annular Ligament Distal Radioulnar