Rural Bioethics: the Alaska Context 1. Size, Population, and (In
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

REGIONAL SUBSISTENCE BIBLIOGRAPHY Volume IV Southcentral Alaska Number I
REGIONAL SUBSISTENCE BIBLIOGRAPHY Volume IV Southcentral Alaska Number I Jan H. Overturf Alaska Department of Fish and Game Division of Subsistence Technical Paper No. 97 Juneau, Alaska 1984 Cover Drawing by Tim Sczawinski CONTENTS Acknowledgments .............................................. V Introduction ................................................. vii Abbreviations ................................................ xix Southcentral Regional Bibliography ........................... 1 Keyword Index ................................................ 111 Author Index ................................................. 131 iii ACKNOWLEDGEMENTS In compiling this bibliography I received help and suggestions from many sources. The help was eagerly sought after and accepted. I would like to thank the entire staff of the Alaska Department of Fish and Game Subsistence Division, Anchorage Office. Especially helpful were Dr. James A. Fall, Ron Stanek, Lee Stratton and Carolyn Reed. All of these people opened their professional research libraries for my perusal and supplied me with a nearly steady stream of papers to be read, referenced and included in the bibliography. Dr. James Fall was particularly supportive of the project. His enthusiasm and comments were greatly appreciated, and his final review of the rough draft was essential. Dr. William B. Workman of the University of Alaska, Anchorage, generously opened his research library supplying many important recent publications and hard-to- find papers. Dr. Robert Wolfe, Research Director, ADFG -
Geography of Alaska (4 Cr.) Alaska Field Study Spring Semester / May Term, 2013
NCE317A / ENV490A The Cultural and Environmental Geography of Alaska (4 cr.) Alaska Field Study Spring Semester / May Term, 2013 Instructor Dr. David Block, Associate Professor Emeritus, Environmental Science & Geography [email protected] 262-524-9111 (home) Office Hour: Maxon 303, Wed 3-4pm Course Description The purpose of this academic field study experience is to explore the environmental resources and cultural heritage of America’s final frontier – Alaska! Preparatory classes ground students in an understanding of Alaska’s history, physical landscape, Native American heritage, and current natural resource base. The environmental and economic impacts of such activities as commercial fishing, logging, mining, and tourism serve as a central theme for the course. The two week May Term itinerary includes cultural activities in Sitka, Fairbanks and Anchorage involving Tlingit, Athabascan, and other Alaskan Native groups, plus environmental field investigations of Kenai Fiords National Park, Prince William Sound, the historic Yukon mining region, and Mendenhall Glacier. NCEP Program Goals 1. Knowledge: Students will understand the historic, cultural, economic and political forces shaping contemporary society and articulate their own place in the world; understand the connections between power, privilege and acquisition of knowledge both locally and globally; understand how language frames our thinking and perspectives; and/or understand the interconnection and interdependence of global systems. 2. Attitudes: Students will develop cultural self-awareness; develop appreciation for and interest in learning about other cultures; recognize the value of seeing the world through the eyes of others; and/or recognize the value of active citizenship and individual responsibility both within and beyond U.S. borders. -

Aviation Access to Remote Locations in Alaska
Federal Aviation Administration Study for the House and Senate Appropriations Committees May 2001 Aviation Access to Remote Locations In Alaska Recommendations to Increase Aviation Access to Medical Facilities House Report 106-940 accompanying H.R. 4475, FY 2001 DOT Appropriations Table of Contents Glossary .........................................................................................................................................................ii Overview ....................................................................................................................................................... 1 Requirement for this Study............................................................................................................................ 1 Background on Alaska .................................................................................................................................. 2 Communities in Alaska..................................................................................................................... 2 Transportation in Alaska .................................................................................................................. 3 Factors Influencing Aviation Access in Remote Alaskan Communities........................................... 3 NIOSH/NTSB/NWS/FAA Safety Study ............................................................................................ 6 Medical Facilities of the Indian Health Service ............................................................................... -
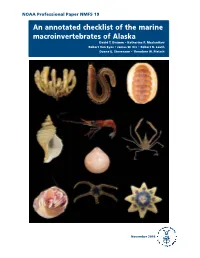
An Annotated Checklist of the Marine Macroinvertebrates of Alaska David T
NOAA Professional Paper NMFS 19 An annotated checklist of the marine macroinvertebrates of Alaska David T. Drumm • Katherine P. Maslenikov Robert Van Syoc • James W. Orr • Robert R. Lauth Duane E. Stevenson • Theodore W. Pietsch November 2016 U.S. Department of Commerce NOAA Professional Penny Pritzker Secretary of Commerce National Oceanic Papers NMFS and Atmospheric Administration Kathryn D. Sullivan Scientific Editor* Administrator Richard Langton National Marine National Marine Fisheries Service Fisheries Service Northeast Fisheries Science Center Maine Field Station Eileen Sobeck 17 Godfrey Drive, Suite 1 Assistant Administrator Orono, Maine 04473 for Fisheries Associate Editor Kathryn Dennis National Marine Fisheries Service Office of Science and Technology Economics and Social Analysis Division 1845 Wasp Blvd., Bldg. 178 Honolulu, Hawaii 96818 Managing Editor Shelley Arenas National Marine Fisheries Service Scientific Publications Office 7600 Sand Point Way NE Seattle, Washington 98115 Editorial Committee Ann C. Matarese National Marine Fisheries Service James W. Orr National Marine Fisheries Service The NOAA Professional Paper NMFS (ISSN 1931-4590) series is pub- lished by the Scientific Publications Of- *Bruce Mundy (PIFSC) was Scientific Editor during the fice, National Marine Fisheries Service, scientific editing and preparation of this report. NOAA, 7600 Sand Point Way NE, Seattle, WA 98115. The Secretary of Commerce has The NOAA Professional Paper NMFS series carries peer-reviewed, lengthy original determined that the publication of research reports, taxonomic keys, species synopses, flora and fauna studies, and data- this series is necessary in the transac- intensive reports on investigations in fishery science, engineering, and economics. tion of the public business required by law of this Department. -

Alaska History
Alaska History Social Studies Grade(s) 10th, Duration 1 Semester, 1 Credit NCAA Approved Required Course Description Alaska History at Mt.Edgecumbe High School is a one credit course that includes units on geography, cultures, Russian America and the American Period of Alaska History. In the geography unit we will build and study maps and graphs. In the cultures unit we will define culture and separate it into its component parts in order to better understand the different ways that Alaskans live. The Russian America Unit (1741-1867) will include field trips, primary source readings and lead up to a team research project. In the American Period of Alaska History (1867- Present), each student will select a topic and present their research to the class. Finally all students will identify connections between the different topics that we have presented by writing cause-effect statements. Scope And Sequence Timeframe Unit Instructional Topics 3 Week(s) Introduction & Geography of Alaska 1. Map Reading 2. Map Making 3. Graphing 4. Making Timelines to Scale 5. Building of the Alaska Pipeline 3 Week(s) Cultures of Alaska 1. Prehistoric & Protohistoric Alaska 2. What is Culture ? 3. Alaska Native Cultures 4. Researching an Alaska Culture of your choice 5. Culture Sharing 3 Week(s) Russian America 1741 - 1867 1. The Age of Discovery and its Origins 2. Overview of Russian America 3. Exploration and First Contact 4. Growth of the Russian American Colony 5. Battle of Sitka 6. Life in New Archangel 7. Researching Russian America 8. Presenting Russian America 9. Sale of Russian America 1 Month(s) American Period 1867 - Present 1. -
Alaska Roads Historic Overview
Alaska Roads Historic Overview Applied Historic Context of Alaska’s Roads Prepared for Alaska Department of Transportation and Public Facilities February 2014 THIS PAGE INTENTIONALLY LEFT BLANK Alaska Roads Historic Overview Applied Historic Context of Alaska’s Roads Prepared for Alaska Department of Transportation and Public Facilities Prepared by www.meadhunt.com and February 2014 Cover image: Valdez-Fairbanks Wagon Road near Valdez. Source: Clifton-Sayan-Wheeler Collection; Anchorage Museum, B76.168.3 THIS PAGE INTENTIONALLY LEFT BLANK Table of Contents Table of Contents Page Executive Summary .................................................................................................................................... 1 1. Introduction .................................................................................................................................... 3 1.1 Project background ............................................................................................................. 3 1.2 Purpose and limitations of the study ................................................................................... 3 1.3 Research methodology ....................................................................................................... 5 1.4 Historic overview ................................................................................................................. 6 2. The National Stage ........................................................................................................................ -

Lesson Plan – Geography of Alaska
LESSON PLAN – GEOGRAPHY OF ALASKA TITLE: Geography of Alaska Time: 60 minutes LEARNER POPULATION: grade level 5 CURRICULAR CONTEXT: part of Social Studies, U.S. History, Alaska OBJECTIVES: By the end of this activity: 1) Students will be able to identify different regions in Alaska. 2) Students will be able to become aware of misconceptions about Alaska. 3) Students will be able to identify places, rivers and mountains on a map of Alaska. 4) Students will be able to identify different Native Alaskan tribes. CONCEPTS/INFORMATION: • Alaskan geography • Working with maps • Misconceptions about Alaska • Native Alaskan groups INSTRUCTIONAL SEQUENCE: 1) Start out with challenging students on what they know about Alaska. Use the sheet “Common Misconceptions about Alaska.” 2) Educate students about the climate in Alaska and about Native Alaskan groups by using the Background Information sheet on Alaska, and by using photos of Alaskan objects, such as the snow goggles or the miniature snow shoes, that are at the Pardee Home Museum. 3) Hand out the blank map of Alaska. Students research in an atlas or on the Internet and fill in place names, rivers, names of mountains, as well as territories of Native Alaskan groups. INSTRUCTIONAL MATERIALS: Background Information Alaska; “Common Misconceptions” sheet; blank map, atlas, Internet, pencils; photos of objects from Pardee Home Museum. EXTENSION/CLOSURE: 1) Students do more in-depth research on Native Alaskan groups. Background Information Alaska The state of Alaska comprises an area of approximately 663,267 square miles which makes it the largest state in the United States. However, only 626,932 people live in Alaska which ranks it 47th among U.S. -
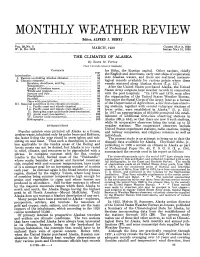
MONTHLY WEATHER REVIEW Editor, ALFRED J
MONTHLY WEATHER REVIEW Editor, ALFRED J. HENRY ~ ____~~~~ ~ . ~ __ VOL. 58,No. 3 1930 CLOSEDMAY 3, 1930 W. B. No. 1012 MARCH, ISSUED MAY31, 1930 ____ THE CLIMATES OF ALASKA By EDITHM. FITTON [C‘lark University School of Geography] CONTENTS for Sitka, the Russian capital. Other nations, chiefly Introduction_____---_---------------------------------. the English and Americans, early sent ships of espIoration I. Factirs controlling Alaskan climates- - - - - -.-. - :g into Alaskan waters, and there are ecatt.ered meteoro- 11. Climatic elements- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - ST logical records available for various points where these Sunshine, cloudiness, and fog-- -_--__-----__--- 87 vessels winte,red along Alaskan shores (7, P. 137). Temperature- - - - - __ _____ - - - - - - - - - _____ - _____ 59 Alter the United States purchased Alaska, the United Length of frostless season.. - - - - - - - - - __ - - - - -.- - - States Army surgeons kept weather records in connection Winds and pressure _____._____________________:: January and July _-___-----.--________________91 with the post hospitals. “In 1878 and 1579, soon after Precipitation - - - -.- - - - - - - - - - - - - - - - - - - - - - - - - - - 93 the orga,nization of the United Stat,e,s Weather Bureau, SnowfaU_____________________~_________-_____96 first under the Signal Corps of t’heArmy, later as a’bureau Days with precipitatioil- - - - - - - - - - - - - - - - - - - - - - - 111. Seasonal conditions in the cliniatic provinces-_ - - - - 9”; of the nePartlne11t of &Ticulture, a feltrfirst-class observ- I A. Pacific coast and islsnds (marine) - - - - -_- - - - 98 ing stations, together mth several volunt,ary stations of I B. Pacific coast and islands (rain shadow)------ 99 lamer order, were established in Masl<a” (1, p, 133). 11. Bering Sea coast and islands (semi-ice marine) - 99 1917 appropriationof $l~,~~operlilit,ted the estab- 111. Arctic coast (ice-marine) - - - - - - - - - - - - - __ - - - an IV. -

Alaska Peninsula
DEPARTMENT OF THE INTERIOR UNITED STATES GEOLOGICAL SURVEY GEORGE OTIS SMITH, DIRECTOK BULLETIN 467 GEOLOGY AND MINERAL RESOURCES OF PARTS OF THE ALASKA PENINSULA BY WALLACE W. ATWOOD WASHINGTON GOVERNMENT PRINTING OFFICE 1911 CONTENTS. Page. Preface, by Alfred H. Brooks ............................................. 7 Introduction............................................................. 9 Location and extent of area considered................................. 9 Previous explorations and surveys..................................... 9 Acknowledgments.........................................;.......... 12 Character of the country.................................................. 13 Geography........................................................... 13 Mountains....................................................... 1.3 Lowlands........................................ ................ 14 Coasts ........-........-....-.---..-----------..---....---.----.- 14 Drainage..................................-.------ -- -- --- ---- 15 Climate.............................................................. 15 Vegetation............................................................ 17 Settlement........................................................... 18 Commercial development.............................................. 19 Transportation .....................................................*.. 22 Geology ................................................................. 23 General features...................................................... 23 Age -

The Cold War Context of Fort Greely, Alaska
LIBERTY UNIVERSITY THE IMPORTANCE OF BEING ANCILLARY: THE COLD WAR CONTEXT OF FORT GREELY, ALASKA A THESIS SUBMITTED TO THE FACULTY OF THE HISTORY DEPARTMENT IN CANDIDACY FOR THE DEGREE OF MASTER OF HISTORY BY CATHERINE R. HARDEE LYNCHBURG, VIRGINIA MAY 2014 Table of Contents Introduction....................................................................................................................................1 Chapter 1 - World War II on the Last Frontier .........................................................................5 Chapter 2 - Fighting a Cold War in Cold Weather..................................................................16 Chapter 3 - Testing and Training at Fort Greely.....................................................................37 Chapter 4 - Cold War Science at Fort Greely...........................................................................61 Conclusion....................................................................................................................................86 Bibliography.................................................................................................................................90 Introduction Summer in Alaska has another name to locals: road construction. Between the widespread construction zones that can keep traffic halted for up to thirty minutes at a time and the hundreds of massive RVs that creep along the scenic highways oblivious to the dozens of cars inching along behind waiting, frustrated, for an opportunity to pass, road trips during -
MONTHLY WEATHER REVIEW Editor, ALFRED J
MONTHLY WEATHER REVIEW Editor, ALFRED J. HENRY ~ ____~~~~ ~ . ~ __ VOL. 58,No. 3 1930 CLOSEDMAY 3, 1930 W. B. No. 1012 MARCH, ISSUED MAY31, 1930 ____ THE CLIMATES OF ALASKA By EDITHM. FITTON [C‘lark University School of Geography] CONTENTS for Sitka, the Russian capital. Other nations, chiefly Introduction_____---_---------------------------------. the English and Americans, early sent ships of espIoration I. Factirs controlling Alaskan climates- - - - - -.-. - :g into Alaskan waters, and there are ecatt.ered meteoro- 11. Climatic elements- - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - - ST logical records available for various points where these Sunshine, cloudiness, and fog-- -_--__-----__--- 87 vessels winte,red along Alaskan shores (7, P. 137). Temperature- - - - - __ _____ - - - - - - - - - _____ - _____ 59 Alter the United States purchased Alaska, the United Length of frostless season.. - - - - - - - - - __ - - - - -.- - - States Army surgeons kept weather records in connection Winds and pressure _____._____________________:: January and July _-___-----.--________________91 with the post hospitals. “In 1878 and 1579, soon after Precipitation - - - -.- - - - - - - - - - - - - - - - - - - - - - - - - - - 93 the orga,nization of the United Stat,e,s Weather Bureau, SnowfaU_____________________~_________-_____96 first under the Signal Corps of t’heArmy, later as a’bureau Days with precipitatioil- - - - - - - - - - - - - - - - - - - - - - - 111. Seasonal conditions in the cliniatic provinces-_ - - - - 9”; of the nePartlne11t of &Ticulture, a feltrfirst-class observ- I A. Pacific coast and islsnds (marine) - - - - -_- - - - 98 ing stations, together mth several volunt,ary stations of I B. Pacific coast and islands (rain shadow)------ 99 lamer order, were established in Masl<a” (1, p, 133). 11. Bering Sea coast and islands (semi-ice marine) - 99 1917 appropriationof $l~,~~operlilit,ted the estab- 111. Arctic coast (ice-marine) - - - - - - - - - - - - - __ - - - an IV. -

The Face of Alaska: a Look at Land Cover and the Potential Drivers of Change
The Face of Alaska: A look at land cover and the potential drivers of change By Benjamin M. Jones, Research Geographer, Alaska Science Center, U.S. Geological Survey Open-File Report 2008-1161 U.S. Department of the Interior U.S. Geological Survey U.S. Department of the Interior DIRK KEMPTHORNE, Secretary U.S. Geological Survey Mark D. Myers, Director U.S. Geological Survey, Reston, Virginia: 2008 For product and ordering information: World Wide Web: http://www.usgs.gov/pubprod Telephone: 1-888-ASK-USGS For more information on the USGS—the Federal source for science about the Earth, its natural and living resources, natural hazards, and the environment: World Wide Web: http://www.usgs.gov Telephone: 1-888-ASK-USGS Suggested citation: Jones, B.M., 2008, The Face of Alaska: A look at land cover and the potential drivers of change: U.S. Geological Survey, Open-File Report 2008-1161, 39 p. Any use of trade, product, or firm names is for descriptive purposes only and does not imply endorsement by the U.S. Government. Although this report is in the public domain, permission must be secured from the individual copyright owners to reproduce any copyrighted material contained within this report. ii Contents Abstract................................................................................................................................................................................1 Introduction .........................................................................................................................................................................2