Bacterial Skin Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Smelly Foot Rash
CLINICAL Smelly foot rash Paulo Morais Ligia Peralta Keywords: skin diseases, infectious Case study A previously healthy Caucasian girl, 6 years of age, presented with pruritic rash on both heels of 6 months duration. The lesions appeared as multiple depressions 1–2 mm in diameter that progressively increased in size. There was no history of trauma or insect bite. She reported local pain when walking, worse with moisture and wearing sneakers. On examination, multiple small crater- like depressions were present, some Figure 1. Heel of patient coalescing into a larger lesion on both heels (Figure 1). There was an unpleasant ‘cheesy’ protective/occluded footwear for prolonged odour and a moist appearance. Wood lamp periods.1–4 examination and potassium hydroxide testing for fungal hyphae were negative. Answer 2 Question 1 Pitted keratolysis is frequently seen during What is the diagnosis? summer and rainy seasons, particularly in tropical regions, although it occurs Question 2 worldwide.1,3,4 It is caused by Kytococcus What causes this condition? sedentarius, Dermatophilus congolensis, or species of Corynebacterium, Actinomyces or Question 3 Streptomyces.1–4 Under favourable conditions How would you confirm the diagnosis? (ie. hyperhidrosis, prolonged occlusion and increased skin surface pH), these bacteria Question 4 proliferate and produce proteinases that destroy What are the differential diagnoses? the stratum corneum, creating pits. Sulphur containing compounds produced by the bacteria Question 5 cause the characteristic malodor. What is your management strategy? Answer 3 Answer 1 Pitted keratolysis is usually a clinical Based on the typical clinical picture and the negative diagnosis with typical hyperhidrosis, malodor ancillary tests, the diagnosis of pitted keratolysis (PK) (bromhidrosis) and occasionally, tenderness, is likely. -

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Study Sheet #1
Pathogens 1. Acinetobacter a. A. calcoaceticus i. Animals, Man – Opportunistic Infections 2. Actinobacillus a. A. actinomycetemocomitans i. Animals – Opportunistic Infection ii. Man – Opportunistic Infection b. A. equuli i. Equine – Actinobacillosis c. A. lignieresii i. Bovine – Actinobacillosis d. A. pleuropneumoniae i. Porcine – Pleuropneumonia 3. Aeromonas a. A. hydrophilia i. Animals, Man – Opportunistic Infection 4. Alcaligenes a. Alcaligenes species i. Animals, Man – Opportunistic Infection 5. Bacillus a. B. anthracis i. Animals, Man – Anthrax b. B. cereus i. Man – Food Poisoning 6. Bordetella a. B. bronchiseptica i. Canine – Tracheobronchitis (Kennel Cough) ii. Porcine – Atrophic Rhinitis b. B. pertussis i. Man – Pertussis (Whooping Cough) 7. Brucella a. B. abortus i. Bovine –Abortion, Orchitis b. B. canis i. Canine - Abortion, Orchitis c. B. melitensis i. Ovine - Abortion, Orchitis d. B. ovis i. Ovine - Abortion, Orchitis e. B. suis i. Porcine - Abortion, Orchitis 8. Burkholderia a. B. mallei i. Equine – Glanders b. B. pseudomallei 9. Campylobacter a. C. fetus fetus i. Ovine – Epizootic abortion b. C. fetus veneralis i. Bovine – Campylobacteriosis c. C. jejuni i. Man – Enteritis d. i. Animal, Man – Melioidosis 10. Clostridium a. C. botulimum i. Animals, Man – Botulism b. C. chauvoei i. Bovine – Blackleg c. C. perfringens i. Ovine – Enterotoxemia ii. Man – Gas Gangrene d. C. tetani i. Animals, Man – Tetanus 11. Corynebacterium a. C. diphtheriae i. Man – Diphtheria b. C. psuedotuberculosis i. Ovine – Caseous lymphadenitis c. C. renale i. Bovine – Contagious pyelonephritis 12. Dermatophilus a. D. congolensis i. Animals, Man – Dermatophilosis 13. Erysipelothrix a. E. rhusiopathiae i. Porcine – Erysipelas ii. Man – Erysipeloid 14. Enterococcus species a. Opportunistic pathogens of humans and domestic animals b. -

Bacterial Infections and Infectious Dermatologic Emergencies.Pdf
Learning Objectives Common Bacterial Infections recognition treatment complications Infectious Dermatologic Emergencies Necrotizing Fasciitis Toxic Shock Syndromes Normal Skin Flora Major function is to prevent skin infections Provides ecological competition for pathogens Hydrolyzes the lipids in sebum into free fatty acids which are toxic to many bacteria- linoleic and linolenic acid are more inhibitory of Staph Aureus Antimicrobial Peptides from lamellar bodies, Cathelicidins, and Defensins function to control overgrowth of pathogens Normal Skin Flora Aerobic Cocci Staphylococcus epidermidis Most common coccus on human skin All body sites, especially intertriginous areas Staphylococcus aureus More common in Atopic Dermatitis, Diabetes Mellitus, Hemodialysis, IVDU, Liver Disease, and HIV resident or contaminant? anterior nares- 20-35% perineum- 20% axillae and toe webs- 5-10% Normal Skin Flora Aerobic Coryneform Bacteria Corynebacterium minutissimum- intertriginous sites Erythrasma Anaerobic Coryneform Bacteria Propionibacterium acnes- sebaceous glands, hair follicles Acne vulgaris Gram Negative Bacteria Acinetobacter species- axillae, perineum, antecubital fossae - Requires moisture and maceration which increases pH and CO2 levels Yeast Pityrosporum ovale/Malassezia furfur- sebaceous sites Tinea Versicolor Introduction Strep and Staph cause the majority of skin infections in immunocompetent patients Immunodeficiency and underlying systemic disease result in severe infections which tend to be refractory to -

Disease Transmission
Rudolph Virchow Wild Pig Diseases: Father of modern Current Issues and pathology Potential Concerns First used the term “zoonosis” S. W. Jack, DVM, MS, PhD Mississippi State University College of Veterinary Medicine Strong advocate of Pathobiology/Population Medicine “one medicine” Tenet of population medicine: Disease Transmission Most new problems are introduced •Source Accidental vs. malicious •Susceptible host 75% of emerging diseases in humans •Means of transmission are ZOONOTIC 80% zoonotic diseases involve wildlife 1 Source of the agent Susceptible Host Diseased animals Emigration (natural) Means Offal & other waste Importation (transportation) Means Vectors / fomites / environment Stressors (Population density, weather, REMEMBER : humans ARE animals ! ! + nutrition, other disease, etc) Disease Impact Means of Transmission Wildlife Direct contact Means Vectors / fomites / environment Public Agriculture/ Health Environment 2 Diseases of Swine More than Zoonotic Impact Abscesses Eclampsia Porcine Cytomegalovirus Infection (PCMV) Muscle Tearing Rabies Tetanus Bovine (Porcine) Spongiform Encephalopathy (BSE) Actinobacillosis Electrocution Japanese B Porcine Dermatitis and Nephropathy Syndrome (PDNS) Mycoplasma Arthritis Rectal Stricture Encephalitis Virus (JE) Bovine Viral Diarrhoea Virus (BVD) Actinobacillus Pleuropneumonia (App) Encephalomyocarditis Thin Sow Syndrome Porcine Enteropathy Mycotoxicosis Reproduction Jaw and Snout Brucellosis Agalactia Endometritis Deviation Porcine Epidemic Diarrhoea (PED) Navel Bleeding Retroviruses -
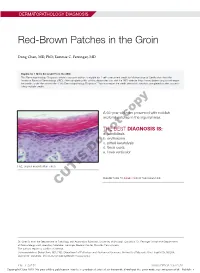
Red-Brown Patches in the Groin
DERMATOPATHOLOGY DIAGNOSIS Red-Brown Patches in the Groin Dong Chen, MD, PhD; Tammie C. Ferringer, MD Eligible for 1 MOC SA Credit From the ABD This Dermatopathology Diagnosis article in our print edition is eligible for 1 self-assessment credit for Maintenance of Certification from the American Board of Dermatology (ABD). After completing this activity, diplomates can visit the ABD website (http://www.abderm.org) to self-report the credits under the activity title “Cutis Dermatopathology Diagnosis.” You may report the credit after each activity is completed or after accumu- lating multiple credits. A 66-year-old man presented with reddish arciform patchescopy in the inguinal area. THE BEST DIAGNOSIS IS: a. candidiasis b. noterythrasma c. pitted keratolysis d. tinea cruris Doe. tinea versicolor H&E, original magnification ×600. PLEASE TURN TO PAGE 419 FOR THE DIAGNOSIS CUTIS Dr. Chen is from the Department of Pathology and Anatomical Sciences, University of Missouri, Columbia. Dr. Ferringer is from the Departments of Dermatology and Laboratory Medicine, Geisinger Medical Center, Danville, Pennsylvania. The authors report no conflict of interest. Correspondence: Dong Chen, MD, PhD, Department of Pathology and Anatomical Sciences, University of Missouri, One Hospital Dr, MA204, DC018.00, Columbia, MO 65212 ([email protected]). 416 I CUTIS® WWW.MDEDGE.COM/CUTIS Copyright Cutis 2018. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. DERMATOPATHOLOGY DIAGNOSIS DISCUSSION THE DIAGNOSIS: Erythrasma rythrasma usually involves intertriginous areas surface (Figure 1) compared to dermatophyte hyphae that (eg, axillae, groin, inframammary area). Patients tend to be parallel to the surface.2 E present with well-demarcated, minimally scaly, red- Pitted keratolysis is a superficial bacterial infection brown patches. -

The Power of Homeopathy in Animal Diseases
Balaji Deekshitulu P V, IJAR, 2019; 4:27 Review Article IJAR (2019) 4:27 International Journal of Animal Research (ISSN:2575-7822) The Power of Homeopathy in Animal Diseases Dr Balaji Deekshitulu P V Homeopathy Physician and Counseling Psychologist, Sri Balaji Homeopathy & Personal Counseling Center, Tirupati, A.P, India.cell:8885391722 / 7207255557. ABSTRACT Homeopathy a medicine (remedy) is selected which would pro- *Correspondence to Author: duce in a healthy body the same symptoms found in the sick Dr Balaji Deekshitulu P V animal (“like cures like”). This substance is selected from herbs, Homeopathy Physician and Coun- minerals, and natural compounds which are then diluted beyond seling Psychologist, Sri Balaji the point of possible toxicity.This review article explains that Ho- Homeopathy & Personal Coun- meopathy Treat met is best treatment in animals also. seling Center, Tirupati, A.P, India. cell:8885391722 / 7207255557. Keywords: Diseases, Homeopathy, Animals How to cite this article: Balaji Deekshitulu P V, The Power of Homeopathy in Animal Diseases. International Journal of Animal Re- search, 2019; 4:27. eSciPub LLC, Houston, TX USA. Website: https://escipub.com/ https://escipub.com/international-journal-of-animal-research/ 1 Balaji Deekshitulu P V, IJAR, 2019; 4:27 Introduction • Belladonna: Sudden and high fever, redness, pain, dilated pupils and panting. Homeopathy has been found one of the best holistic and safest treatments for many people. • Borax: For fear of thunderstorms and This has been found true for animals and plants fireworks as well. Veterinary homeopathy is a safe, • Bryonia: Colic, all symptoms worse with effective and powerful form of medicine. Most motion and better by resting or staying veterinarians choose homeopathy due to the perfectly still, thirst for large amounts of chronic and recurring nature of many ailments water, vomiting bile after eating, in animals. -
Serological Patterns of Actinobacillus Pleuropneumoniae, Mycoplasma
Wallgren et al. Acta Vet Scand (2016) 58:71 DOI 10.1186/s13028-016-0252-1 Acta Veterinaria Scandinavica RESEARCH Open Access Serological patterns of Actinobacillus pleuropneumoniae, Mycoplasma hyopneumoniae, Pasteurella multocida and Streptococcus suis in pig herds affected by pleuritis Per Wallgren1,2*, Erik Nörregård3, Benedicta Molander3, Maria Persson1 and Carl‑Johan Ehlorsson3 Abstract Background: Respiratory illness is traditionally regarded as the disease of the growing pig, and has historically mainly been associated to bacterial infections with focus on Mycoplasma hyopneumoniae and Actinobacillus pleuro- pneumoniae. These bacteria still are of great importance, but continuously increasing herd sizes have complicated the scenario and the influence of secondary invaders may have been increased. The aim of this study was to evaluate the presence of A. pleuropneumoniae and M. hyopneumoniae, as well as that of the secondary invaders Pasteurella multocida and Streptococcus suis by serology in four pig herds (A–D) using age segregated rearing systems with high incidences of pleuritic lesions at slaughter. Results: Pleuritic lesions registered at slaughter ranged from 20.5 to 33.1 % in the four herds. In herd A, the levels of serum antibodies to A. pleuropneumoniae exceeded A450 > 1.5, but not to any other microbe searched for. The seroconversion took place early during the fattening period. Similar levels of serum antibodies to A. pleuropneumoniae were also recorded in herd B, with a subsequent increase in levels of antibodies to P. multocida. Pigs seroconverted to both agents during the early phase of the fattening period. In herd C, pigs seroconverted to P. multocida during the early phase of the fattening period and thereafter to A. -

Prioritization of Health Services
PRIORITIZATION OF HEALTH SERVICES A Report to the Governor and the 74th Oregon Legislative Assembly Oregon Health Services Commission Office for Oregon Health Policy and Research Department of Administrative Services 2007 TABLE OF CONTENTS List of Figures . iii Health Services Commission and Staff . .v Acknowledgments . .vii Executive Summary . ix CHAPTER ONE: A HISTORY OF HEALTH SERVICES PRIORITIZATION UNDER THE OREGON HEALTH PLAN Enabling Legislatiion . 3 Early Prioritization Efforts . 3 Gaining Waiver Approval . 5 Impact . 6 CHAPTER TWO: PRIORITIZATION OF HEALTH SERVICES FOR 2008-09 Charge to the Health Services Commission . .. 25 Biennial Review of the Prioritized List . 26 A New Prioritization Methodology . 26 Public Input . 36 Next Steps . 36 Interim Modifications to the Prioritized List . 37 Technical Changes . 38 Advancements in Medical Technology . .42 CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES Practice Guidelines . 47 Age-Related Macular Degeneration (AMD) . 47 Chronic Anal Fissure . 48 Comfort Care . 48 Complicated Hernias . 49 Diagnostic Services Not Appearing on the Prioritized List . 49 Non-Prenatal Genetic Testing . 49 Tuberculosis Blood Test . 51 Early Childhood Mental Health . 52 Adjustment Reactions In Early Childhood . 52 Attention Deficit and Hyperactivity Disorders in Early Childhood . 53 Disruptive Behavior Disorders In Early Childhood . 54 Mental Health Problems In Early Childhood Related To Neglect Or Abuse . 54 Mood Disorders in Early Childhood . 55 Erythropoietin . 55 Mastocytosis . 56 Obesity . 56 Bariatric Surgery . 56 Non-Surgical Management of Obesity . 58 PET Scans . 58 Prenatal Screening for Down Syndrome . 59 Prophylactic Breast Removal . 59 Psoriasis . 59 Reabilitative Therapies . 60 i TABLE OF CONTENTS (Cont’d) CHAPTER THREE: CLARIFICATIONS TO THE PRIORITIZED LIST OF HEALTH SERVICES (CONT’D) Practice Guidelines (Cont’d) Sinus Surgery . -

SALMONELLA in the LYMPH NODES of CATTLE PRESENTED for HARVEST by Sara Elizabeth Gragg, M.S. a Dissertation in ANIMAL SCIENCE Su
SALMONELLA IN THE LYMPH NODES OF CATTLE PRESENTED FOR HARVEST By Sara Elizabeth Gragg, M.S. A Dissertation In ANIMAL SCIENCE Submitted to the Graduate Faculty of Texas Tech University in Partial Fulfillment of the Requirements for the Degree of DOCTOR OF PHILOSOPHY Approved Dr. Mindy Brashears Chair of Committee Dr. Guy H. Loneragan Dr. J. Chance Brooks Dr. Mark Miller Dr. Michael San Francisco Dominick Casadonte Dean of the Graduate School December, 2012 Copyright 2012, Sara Elizabeth Gragg Texas Tech University, Sara Elizabeth Gragg, December 2012 ACKNOWLEDGEMENTS To my advisor, Dr. Mindy Brashears, I thank you for the opportunity to learn from you both personally and professionally over the previous fifteen years. You have provided me with amazing opportunities and have been an outstanding role model. I have the utmost respect for you and am truly blessed to call you my mentor and my friend. To my committee, Drs. Mindy Brashears, Guy Loneragan, Chance Brooks, Mark Miller and Michael San Francisco, I look up to each of you and appreciate the guidance and support you have provided throughout my education at Texas Tech University. Thank you, Drs. Guy Loneragan and Kendra Nightingale, for the expertise and opportunities that you have shared with me. I have learned a great deal from each of you and consider you both great mentors of mine. I gratefully acknowledge the numerous graduate students, staff members and student workers who contributed significantly to the success of my research and made my graduate education memorable. Your friendship and support have been invaluable. A special thank you to Dr. -

Download Erythasma
ERYTHASMA What is it? Erythasma is a common skin condition that affects the following areas – the groin, under the arms and between the toes What does it look like? Erythrasma appears as well-defined scaly red, pink or brown patches. The most commonly affected areas are the groin, armpits, between the toes and in other skin folds. It can sometimes become generalized and affect larger areas on the body. The patches can sometimes be itchy or have an odor. What causes it? Erythrasma is an infection of the skin caused by an overgrowth of a bacterium called Corynebacterium minutissimum. It can affect healthy adults, but it more frequently affects older people with obesity, excessive sweating (hyperhidrosis [link]), diabetes mellitus or people who live in tropical climates. Infection is facilitated under conditions of moisture and occlusion. How is it diagnosed? Erythrasma is diagnosed based on the history and physical appearance of the lesions. A special lamp called a Wood’s lamp can be used to help confirm the diagnosis, as erythrasma glows bright pink under the lamp. How is it treated? Erythrasma can be treated with either topical (applied directly to the skin) or oral therapies. For patients with localised disease, a topical antibiotic such as clindamycin or erythromycin can be used. On the hand, it can be difficult to treat extensive areas with creams and so oral antibiotics (clindamycin or erythromycin) may be preferred. It is important to note that recurrence is common. What can be done to prevent it? In order to avoid recurrences, it is important to keep the skin as dry as possible and optimise pre-disposing conditions such as keeping diabetes well-controlled.