Bacterial Skin Infections
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Smelly Foot Rash
CLINICAL Smelly foot rash Paulo Morais Ligia Peralta Keywords: skin diseases, infectious Case study A previously healthy Caucasian girl, 6 years of age, presented with pruritic rash on both heels of 6 months duration. The lesions appeared as multiple depressions 1–2 mm in diameter that progressively increased in size. There was no history of trauma or insect bite. She reported local pain when walking, worse with moisture and wearing sneakers. On examination, multiple small crater- like depressions were present, some Figure 1. Heel of patient coalescing into a larger lesion on both heels (Figure 1). There was an unpleasant ‘cheesy’ protective/occluded footwear for prolonged odour and a moist appearance. Wood lamp periods.1–4 examination and potassium hydroxide testing for fungal hyphae were negative. Answer 2 Question 1 Pitted keratolysis is frequently seen during What is the diagnosis? summer and rainy seasons, particularly in tropical regions, although it occurs Question 2 worldwide.1,3,4 It is caused by Kytococcus What causes this condition? sedentarius, Dermatophilus congolensis, or species of Corynebacterium, Actinomyces or Question 3 Streptomyces.1–4 Under favourable conditions How would you confirm the diagnosis? (ie. hyperhidrosis, prolonged occlusion and increased skin surface pH), these bacteria Question 4 proliferate and produce proteinases that destroy What are the differential diagnoses? the stratum corneum, creating pits. Sulphur containing compounds produced by the bacteria Question 5 cause the characteristic malodor. What is your management strategy? Answer 3 Answer 1 Pitted keratolysis is usually a clinical Based on the typical clinical picture and the negative diagnosis with typical hyperhidrosis, malodor ancillary tests, the diagnosis of pitted keratolysis (PK) (bromhidrosis) and occasionally, tenderness, is likely. -

Chapter 3 Bacterial and Viral Infections
GBB03 10/4/06 12:20 PM Page 19 Chapter 3 Bacterial and viral infections A mighty creature is the germ gain entry into the skin via minor abrasions, or fis- Though smaller than the pachyderm sures between the toes associated with tinea pedis, His customary dwelling place and leg ulcers provide a portal of entry in many Is deep within the human race cases. A frequent predisposing factor is oedema of His childish pride he often pleases the legs, and cellulitis is a common condition in By giving people strange diseases elderly people, who often suffer from leg oedema Do you, my poppet, feel infirm? of cardiac, venous or lymphatic origin. You probably contain a germ The affected area becomes red, hot and swollen (Ogden Nash, The Germ) (Fig. 3.1), and blister formation and areas of skin necrosis may occur. The patient is pyrexial and feels unwell. Rigors may occur and, in elderly Bacterial infections people, a toxic confusional state. In presumed streptococcal cellulitis, penicillin is Streptococcal infection the treatment of choice, initially given as ben- zylpenicillin intravenously. If the leg is affected, Cellulitis bed rest is an important aspect of treatment. Where Cellulitis is a bacterial infection of subcutaneous there is extensive tissue necrosis, surgical debride- tissues that, in immunologically normal individu- ment may be necessary. als, is usually caused by Streptococcus pyogenes. A particularly severe, deep form of cellulitis, in- ‘Erysipelas’ is a term applied to superficial volving fascia and muscles, is known as ‘necrotiz- streptococcal cellulitis that has a well-demarcated ing fasciitis’. This disorder achieved notoriety a few edge. -

WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T
(12) INTERNATIONAL APPLICATION PUBLISHED UNDER THE PATENT COOPERATION TREATY (PCT) (19) World Intellectual Property Organization International Bureau (10) International Publication Number (43) International Publication Date WO 2014/134709 Al 12 September 2014 (12.09.2014) P O P C T (51) International Patent Classification: (81) Designated States (unless otherwise indicated, for every A61K 31/05 (2006.01) A61P 31/02 (2006.01) kind of national protection available): AE, AG, AL, AM, AO, AT, AU, AZ, BA, BB, BG, BH, BN, BR, BW, BY, (21) International Application Number: BZ, CA, CH, CL, CN, CO, CR, CU, CZ, DE, DK, DM, PCT/CA20 14/000 174 DO, DZ, EC, EE, EG, ES, FI, GB, GD, GE, GH, GM, GT, (22) International Filing Date: HN, HR, HU, ID, IL, IN, IR, IS, JP, KE, KG, KN, KP, KR, 4 March 2014 (04.03.2014) KZ, LA, LC, LK, LR, LS, LT, LU, LY, MA, MD, ME, MG, MK, MN, MW, MX, MY, MZ, NA, NG, NI, NO, NZ, (25) Filing Language: English OM, PA, PE, PG, PH, PL, PT, QA, RO, RS, RU, RW, SA, (26) Publication Language: English SC, SD, SE, SG, SK, SL, SM, ST, SV, SY, TH, TJ, TM, TN, TR, TT, TZ, UA, UG, US, UZ, VC, VN, ZA, ZM, (30) Priority Data: ZW. 13/790,91 1 8 March 2013 (08.03.2013) US (84) Designated States (unless otherwise indicated, for every (71) Applicant: LABORATOIRE M2 [CA/CA]; 4005-A, rue kind of regional protection available): ARIPO (BW, GH, de la Garlock, Sherbrooke, Quebec J1L 1W9 (CA). GM, KE, LR, LS, MW, MZ, NA, RW, SD, SL, SZ, TZ, UG, ZM, ZW), Eurasian (AM, AZ, BY, KG, KZ, RU, TJ, (72) Inventors: LEMIRE, Gaetan; 6505, rue de la fougere, TM), European (AL, AT, BE, BG, CH, CY, CZ, DE, DK, Sherbrooke, Quebec JIN 3W3 (CA). -

Bacterial Skin Infections
BACTERIAL SKIN INFECTIONS SPEAKER: DR LUIZ ALBERTO BOMJARDIM PÔRTO DERMATOLOGIST BRAZIL MRSA INFECTIONS • Concept: Methicillin- resistant Staphylococcus aureus • Epidemiology: Gradual increase of resistance. • Nosocomial MRSA risk factors: Hospitalization, ICU, invasive procedures, previous antibiotic therapy, health professionals, diabetes mellitus, EV drugs, immunosuppression and chronic diseases. MRSA INFECTIONS • Community MARSA risk factors: Children, EV drugs, indigenous, homosexual men, military, prisoners and athletes. • Microorganisms more virulent by genetic characteristics. MRSA INFECTIONS • Clinic caracteristics: -Abscess, cellulitis, folliculitis, impetigo, infected wounds, external otitis, paronychia and colonization of the skin in cases of atopic dermatitis. - Increased morbidity. • Propedeutics: Culture blood, tissue or secretion. MRSA INFECTIONS • Treatment: - Pathology-specific treatment. - Prefer non-beta-lactam antibiotics, such as: clindamycin, sulfamethoxazole- trimethoprim and tetracyclines. - On suspicion of MARSA infection, start empirical antibiotics and stagger specific antibiotics by culture with antibiograma. MRSA INFECTIONS • Treatment: - Decolonization: systemic antibiotic therapy, topical 2% mupirocin, personal hygiene with antiseptic or antimicrobial solutions (iodine-povidine, chlorhexidine or triclosan). MRSA INFECTIONS • Prevention: - Avoid skin-to-skin contact and share personal belongings / clothing. - Hand washing. - Use of alcohol gels. - Cover wounds. - Isolation contact of MARSA carriers. - Early -

Bacterial Infections and Infectious Dermatologic Emergencies.Pdf
Learning Objectives Common Bacterial Infections recognition treatment complications Infectious Dermatologic Emergencies Necrotizing Fasciitis Toxic Shock Syndromes Normal Skin Flora Major function is to prevent skin infections Provides ecological competition for pathogens Hydrolyzes the lipids in sebum into free fatty acids which are toxic to many bacteria- linoleic and linolenic acid are more inhibitory of Staph Aureus Antimicrobial Peptides from lamellar bodies, Cathelicidins, and Defensins function to control overgrowth of pathogens Normal Skin Flora Aerobic Cocci Staphylococcus epidermidis Most common coccus on human skin All body sites, especially intertriginous areas Staphylococcus aureus More common in Atopic Dermatitis, Diabetes Mellitus, Hemodialysis, IVDU, Liver Disease, and HIV resident or contaminant? anterior nares- 20-35% perineum- 20% axillae and toe webs- 5-10% Normal Skin Flora Aerobic Coryneform Bacteria Corynebacterium minutissimum- intertriginous sites Erythrasma Anaerobic Coryneform Bacteria Propionibacterium acnes- sebaceous glands, hair follicles Acne vulgaris Gram Negative Bacteria Acinetobacter species- axillae, perineum, antecubital fossae - Requires moisture and maceration which increases pH and CO2 levels Yeast Pityrosporum ovale/Malassezia furfur- sebaceous sites Tinea Versicolor Introduction Strep and Staph cause the majority of skin infections in immunocompetent patients Immunodeficiency and underlying systemic disease result in severe infections which tend to be refractory to -
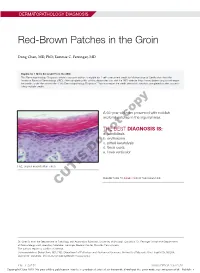
Red-Brown Patches in the Groin
DERMATOPATHOLOGY DIAGNOSIS Red-Brown Patches in the Groin Dong Chen, MD, PhD; Tammie C. Ferringer, MD Eligible for 1 MOC SA Credit From the ABD This Dermatopathology Diagnosis article in our print edition is eligible for 1 self-assessment credit for Maintenance of Certification from the American Board of Dermatology (ABD). After completing this activity, diplomates can visit the ABD website (http://www.abderm.org) to self-report the credits under the activity title “Cutis Dermatopathology Diagnosis.” You may report the credit after each activity is completed or after accumu- lating multiple credits. A 66-year-old man presented with reddish arciform patchescopy in the inguinal area. THE BEST DIAGNOSIS IS: a. candidiasis b. noterythrasma c. pitted keratolysis d. tinea cruris Doe. tinea versicolor H&E, original magnification ×600. PLEASE TURN TO PAGE 419 FOR THE DIAGNOSIS CUTIS Dr. Chen is from the Department of Pathology and Anatomical Sciences, University of Missouri, Columbia. Dr. Ferringer is from the Departments of Dermatology and Laboratory Medicine, Geisinger Medical Center, Danville, Pennsylvania. The authors report no conflict of interest. Correspondence: Dong Chen, MD, PhD, Department of Pathology and Anatomical Sciences, University of Missouri, One Hospital Dr, MA204, DC018.00, Columbia, MO 65212 ([email protected]). 416 I CUTIS® WWW.MDEDGE.COM/CUTIS Copyright Cutis 2018. No part of this publication may be reproduced, stored, or transmitted without the prior written permission of the Publisher. DERMATOPATHOLOGY DIAGNOSIS DISCUSSION THE DIAGNOSIS: Erythrasma rythrasma usually involves intertriginous areas surface (Figure 1) compared to dermatophyte hyphae that (eg, axillae, groin, inframammary area). Patients tend to be parallel to the surface.2 E present with well-demarcated, minimally scaly, red- Pitted keratolysis is a superficial bacterial infection brown patches. -

Download Erythasma
ERYTHASMA What is it? Erythasma is a common skin condition that affects the following areas – the groin, under the arms and between the toes What does it look like? Erythrasma appears as well-defined scaly red, pink or brown patches. The most commonly affected areas are the groin, armpits, between the toes and in other skin folds. It can sometimes become generalized and affect larger areas on the body. The patches can sometimes be itchy or have an odor. What causes it? Erythrasma is an infection of the skin caused by an overgrowth of a bacterium called Corynebacterium minutissimum. It can affect healthy adults, but it more frequently affects older people with obesity, excessive sweating (hyperhidrosis [link]), diabetes mellitus or people who live in tropical climates. Infection is facilitated under conditions of moisture and occlusion. How is it diagnosed? Erythrasma is diagnosed based on the history and physical appearance of the lesions. A special lamp called a Wood’s lamp can be used to help confirm the diagnosis, as erythrasma glows bright pink under the lamp. How is it treated? Erythrasma can be treated with either topical (applied directly to the skin) or oral therapies. For patients with localised disease, a topical antibiotic such as clindamycin or erythromycin can be used. On the hand, it can be difficult to treat extensive areas with creams and so oral antibiotics (clindamycin or erythromycin) may be preferred. It is important to note that recurrence is common. What can be done to prevent it? In order to avoid recurrences, it is important to keep the skin as dry as possible and optimise pre-disposing conditions such as keeping diabetes well-controlled. -
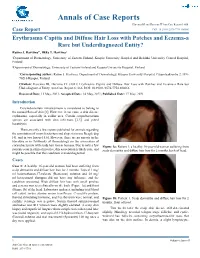
Erythrasma Capitis and Diffuse Hair Loss with Patches and Eczema-A Rare but Underdiagnozed Entity? Rauno J
Annals of Case Reports Harvima RJ and Harvima IT Ann Case Report 6: 666. Case Report DOI: 10.29011/2574-7754.100666 Erythrasma Capitis and Diffuse Hair Loss with Patches and Eczema-a Rare but Underdiagnozed Entity? Rauno J. Harvima1*, Ilkka T. Harvima2 1Department of Dermatology, University of Eastern Finland, Kuopio University Hospital and Helsinki University Central Hospital, Finland 2Department of Dermatology, University of Eastern Finland and Kuopio University Hospital, Finland *Corresponding author: Rauno J. Harvima, Department of Dermatology, Kuopio University Hospital, Puijonlaaksontie 2, FIN- 70210 Kuopio, Finland Citation: Harvima RJ, Harvima IT. (2021) Erythrasma Capitis and Diffuse Hair Loss with Patches and Eczema-a Rare but Underdiagnozed Entity. Ann Case Report 6: 666. DOI: 10.29011/2574-7754.100666 Received Date: 11 May, 2021; Accepted Date: 14 May, 2021; Published Date: 17 May, 2021 Introduction Corynebacterium minutissimum is considered to belong to the normal flora of skin [1]. However, it can cause a skin disease erythrasma, especially in axillar area. Certain corynebacterium species are associated with skin infections [2,3], and pitted keratolysis. There are only a few reports published for animals regarding the association of corynebacterium and alopecia in one Beagle dog [4], and in two horses [5,6]. However, there are no reports in the literature or in Textbooks of Dermatology on the association of corynebacterium with scalp hair loss in humans. Due to only a few Figure 1a: Patient 1, a healthy 16-year-old woman suffering from patients seen in clinical practice, this association is likely rare, and scalp dermatitis and diffuse hair loss for 2 months, back of head. -

Infectious Diseases of the Philippines
INFECTIOUS DISEASES OF THE PHILIPPINES Stephen Berger, MD Infectious Diseases of the Philippines - 2013 edition Infectious Diseases of the Philippines - 2013 edition Stephen Berger, MD Copyright © 2013 by GIDEON Informatics, Inc. All rights reserved. Published by GIDEON Informatics, Inc, Los Angeles, California, USA. www.gideononline.com Cover design by GIDEON Informatics, Inc No part of this book may be reproduced or transmitted in any form or by any means without written permission from the publisher. Contact GIDEON Informatics at [email protected]. ISBN-13: 978-1-61755-582-4 ISBN-10: 1-61755-582-7 Visit http://www.gideononline.com/ebooks/ for the up to date list of GIDEON ebooks. DISCLAIMER: Publisher assumes no liability to patients with respect to the actions of physicians, health care facilities and other users, and is not responsible for any injury, death or damage resulting from the use, misuse or interpretation of information obtained through this book. Therapeutic options listed are limited to published studies and reviews. Therapy should not be undertaken without a thorough assessment of the indications, contraindications and side effects of any prospective drug or intervention. Furthermore, the data for the book are largely derived from incidence and prevalence statistics whose accuracy will vary widely for individual diseases and countries. Changes in endemicity, incidence, and drugs of choice may occur. The list of drugs, infectious diseases and even country names will vary with time. Scope of Content: Disease designations may reflect a specific pathogen (ie, Adenovirus infection), generic pathology (Pneumonia - bacterial) or etiologic grouping (Coltiviruses - Old world). Such classification reflects the clinical approach to disease allocation in the Infectious Diseases Module of the GIDEON web application. -

COMMON FUNGUS INFECTIONS of the SKIN by I
255 Postgrad Med J: first published as 10.1136/pgmj.23.259.255 on 1 May 1947. Downloaded from COMMON FUNGUS INFECTIONS OF THE SKIN By I. R. MARRE, M.R.C.S., L.R.C.P. Skin Physician to the Acton, Evelina and Metropolitan Hospitals. The common superficial mycoses of the skin produce a vigorous reaction, frequently going are caused by a number of different organisms, on to pustulation. and I -propose to give a short general descrip- The Achoria are responsible for the produc- tion of the types of fungi usually responsible tion of favus, characterized by the occurrence for these infections, before proceeding to the of yellowish, cup-shaped scutula. It com- question of diagnosis and treatment. monly affects the scalp, but may affect the hair, There are three groups to be considered:- glabrous skin or nails. The usual organism is I. Ringworm fungi. A. Schonleini, but the group is nowadays 2. Monilia. usually placed in the endothrix trichophyta.' The epidermophyta never affect the hair. 3. Other fungi. They are commonly responsible (especially the I. Ringworm fungi. This is a very large E. inguinale) for infection of the crural region by copyright. class, but we need refer only to the following (Tinea cruris or Dhobie Itch), between the types:- toes and in the nails. (a) Microspora. 2. Monilia. These are a group of yeast-like (b) Trichophyta. fungi, of which the usual one is M. albicans. (c) Achoria. Unlike the ringworm fungi, the manifestations (d) Epidermophyta. of which are usually fairly localized, monilia are capable of serious generalized and systemic http://pmj.bmj.com/ The microspora have small spores in mosaic infections. -

Daniel Zelac, MD Scripps Clinic Conflicts of Interest – None
Daniel Zelac, MD Scripps Clinic Conflicts of Interest – None Many of the photographs and diagrams contained in this talk can be referenced in Clinical Dermatology, 5th Edition By Thomas P. Habif, MD Please do not reproduce or distribute further (referenced in talk as “Habif 5th”) Atopic Dermatitis Perleche Allergic Dermatitis Lip Licker’s Dermatitis Herpes Impetigo Aphthous Ulcerative Disease Actinic Chelitis Squamous Cell Carcinoma Skinsight.com AKA ( cheilosis, angular stomatitis) noted for fissures and inflammation of the labial commisures. Primary causes – chemical irritant, nutritional deficiencies(B2, Fe, Zinc) Can be associated with Plummer-Vinson syndrome (esophogeal web, iron deficiency anemia, glossitis, cheilitis) TreatmentSecondary –causes – Overlying infection, Candida or Bacterial correction of underlying medical or physical problem Treatment of any secondary bacterial or fungal infection Allergic Contact Dermatitis – Scaling eczematous inflammatory reaction affecting areas in direct contact or neighboring regions to agents typically used in or around the oral cavity EastMaui.com Mango- has within it’s tree sap a compound called ‘Urushiol’ Contact with the sap externally can Principles of Pediatric Dermatology cause the same reaction in people as poison ivy. Toothpastes and Mouthwashes • Flavorings Mints( Spearmint, Peppermint, Menthol, Carvone) Cinnamal (cinnamon) Anethole (star anise) • Antiseptic Propolis • Plaque control Hexylresorcinol • Anti-Inflammatory Azulene • Florides • Preservatives Parabens Dental Floss • Colophony Rosin- from pine and spruce trees (colophonium, colophony, resinterethinae, tall oil, abietic acid, methyl abietate alcohol, abietic alcohol, abietyl alcohol) Dermnet nz.com Lip Licker’s Dermatitis- Herpes Simplex- Candidiasis Inverse Psoriasis Hailey-Hailey Disease Erythrasma (bacterial infection (C. minutissimum)) Tinea Corporis Hidradenitis Suppurativa Tinea Corporis Hidradenitis Suppurativa • Cause - bacterial infection (C. -

The Erythrasma Microorganism in Situ: Studies Using the Skin Surface Biopsy Technique
J Clin Pathol: first published as 10.1136/jcp.25.9.799 on 1 September 1972. Downloaded from J. clin. Path., 1972, 25, 799-803 The erythrasma microorganism in situ: studies using the skin surface biopsy technique R. MARKS, N. D. RAMNARAIN, B. BHOGAL, AND N. T. MOORE From the Institute of Dermatology, St. John's Hospital for Diseases of the Skin, London, and the Depart- ment of Crystallography, Birkbeck College, London SYNOPSIS The skin surface biopsy technique has been used to investigate the erythrasma organism in situ in the stratum corneum in 11 patients. Staining by PAS and Gram stain showed the presence of a large number of organisms arranged haphazardly in some areas and in microcolonies in others. With the scanning electron microscope it was possible to see that smooth filamentous chains of microorganisms had penetrated horn cells and caused disturbance of the surface structure of these cells. Enzyme histochemical tests showed that the erythrasma microorganism possessed a strong react- ivity for NAD diaphorase and other mitochondrial enzymes. The reactivity was focal confirming a complex subcellular organization of organelles. It is suggested that the erythrasma microorganism secretes a mucopolysaccharide sheath in some circumstances. copyright. Erythrasma is a chronic scaly dermatosis affecting all 11 patients were men, the average age was 48 and the body flexures and intertriginous areas of adults. the age range 24 to 63. In nine the groins were Previously it was believed to be due either to a type involved, in four the toe webs were involved, and in of dermatophyte (Microsporum minutissimum) or an four the axillae were involved.