Complete Blood Count and Differential in Diagnosis of Early Onset Neonatal
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
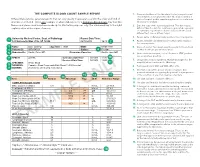
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -
Evaluation of Complete Blood Count Parameters for Diagnosis In
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.68886 • J Pediatr Inf 2020;14(2):e55-e62 Evaluation of Complete Blood Count Parameters for Diagnosis in Children with Sepsis in the Pediatric Intensive Care Unit Pediatrik Yoğun Bakım Ünitesinde Sepsisli Çocuklarda Tanı İçin Tam Kan Sayımı Parametrelerinin Değerlendirilmesi Fatih Aygün1(İD), Cansu Durak1(İD), Fatih Varol1(İD), Haluk Çokuğraş2(İD), Yıldız Camcıoğlu2(İD), Halit Çam1(İD) 1 Department of Pediatric Intensive Care, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey 2 Department of Pediatric Infectious Diseases, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey Cite this article as: Aygün F, Durak C, Varol F, Çokuğraş H, Camcıoğlu Y, Çam H. Evaluation of complete blood count parameters for diagnosis in children with sepsis in the pediatric intensive care unit. J Pediatr Inf 2020;14(2):e55-e62. Abstract Öz Objective: Early diagnosis of sepsis is important for effective treatment Giriş: Erken tanı sepsiste etkili tedavi ve iyi prognoz için önemlidir. C-re- and improved prognosis. C-reactive protein (CRP) and procalcitonin aktif protein (CRP) ve prokalsitonin (PKT) sepsiste en sık kullanılan bi- (PCT) are the most commonly used biomarkers for sepsis. However, their yobelirteçlerdir. Fakat rutinde kullanımı maliyet etkin değildir. Tam kan routine usage is not cost-effective. Complete Blood Count (CBC) param- sayımı (TKS) parametrelerinden eritrosit dağılım genişliği (EDG), nötrofil eters including red cell distribution width (RDW), neutrophil to lympho- lenfosit oranı (NLO), trombosit lenfosit oranı (TLO), ortalama trombosit cyte ratios (NLR), platelet to lymphocyte ratios (PLR), mean platelet vol- hacmi (OTH) basit ve kolay olarak hesaplanmaktadır. Bu çalışmanın ama- ume (MPV), and hemoglobin are simple and easily calculated. -

Complete Blood Count in Primary Care
Complete Blood Count in Primary Care bpac nz better medicine Editorial Team bpacnz Tony Fraser 10 George Street Professor Murray Tilyard PO Box 6032, Dunedin Clinical Advisory Group phone 03 477 5418 Dr Dave Colquhoun Michele Cray free fax 0800 bpac nz Dr Rosemary Ikram www.bpac.org.nz Dr Peter Jensen Dr Cam Kyle Dr Chris Leathart Dr Lynn McBain Associate Professor Jim Reid Dr David Reith Professor Murray Tilyard Programme Development Team Noni Allison Rachael Clarke Rebecca Didham Terry Ehau Peter Ellison Dr Malcolm Kendall-Smith Dr Anne Marie Tangney Dr Trevor Walker Dr Sharyn Willis Dave Woods Report Development Team Justine Broadley Todd Gillies Lana Johnson Web Gordon Smith Design Michael Crawford Management and Administration Kaye Baldwin Tony Fraser Kyla Letman Professor Murray Tilyard Distribution Zane Lindon Lyn Thomlinson Colleen Witchall All information is intended for use by competent health care professionals and should be utilised in conjunction with © May 2008 pertinent clinical data. Contents Key points/purpose 2 Introduction 2 Background ▪ Haematopoiesis - Cell development 3 ▪ Limitations of reference ranges for the CBC 4 ▪ Borderline abnormal results must be interpreted in clinical context 4 ▪ History and clinical examination 4 White Cells ▪ Neutrophils 5 ▪ Lymphocytes 9 ▪ Monocytes 11 ▪ Basophils 12 ▪ Eosinophils 12 ▪ Platelets 13 Haemoglobin and red cell indices ▪ Low haemoglobin 15 ▪ Microcytic anaemia 15 ▪ Normocytic anaemia 16 ▪ Macrocytic anaemia 17 ▪ High haemoglobin 17 ▪ Other red cell indices 18 Summary Table 19 Glossary 20 This resource is a consensus document, developed with haematology and general practice input. We would like to thank: Dr Liam Fernyhough, Haematologist, Canterbury Health Laboratories Dr Chris Leathart, GP, Christchurch Dr Edward Theakston, Haematologist, Diagnostic Medlab Ltd We would like to acknowledge their advice, expertise and valuable feedback on this document. -
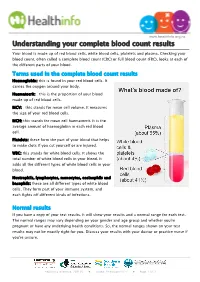
Understanding Your Complete Blood Count Results
www.healthinfo.org.nz Understanding your complete blood count results Your blood is made up of red blood cells, white blood cells, platelets and plasma. Checking your blood count, often called a complete blood count (CBC) or full blood count (FBC), looks at each of the different parts of your blood. Terms used in the complete blood count results Haemoglobin: this is found in your red blood cells. It carries the oxygen around your body. Haematocrit: this is the proportion of your blood made up of red blood cells. MCV: this stands for mean cell volume. It measures the size of your red blood cells. MCH: this stands for mean cell haematocrit. It is the average amount of haemoglobin in each red blood cell. Platelets: these form the part of your blood that helps to make clots if you cut yourself or are injured. WBC: this stands for white blood cells. It shows the total number of white blood cells in your blood. It adds all the different types of white blood cells in your blood. Neutrophils, lymphocytes, monocytes, eosinophils and basophils: these are all different types of white blood cells. They form part of your immune system, and each fights off different kinds of infections. Normal results If you have a copy of your test results, it will show your results and a normal range for each test. The normal ranges may vary depending on your gender and age group and whether you're pregnant or have any underlying health conditions. So, the normal ranges shown on your test results may not be exactly right for you. -
Laboratory Procedure Manual
Laboratory Procedure Manual Analyte: Complete Blood Count Matrix: Whole Blood Method: Complete Blood Count with 5-Part Differential Method No.: Revised: as performed by: Contact: November 2007 Important Information for Users CDC periodically refines these laboratory methods. It is the responsibility of the user to contact the person listed on the title page of each write-up before using the analytical method to find out whether any changes have been made and what revisions, if any, have been incorporated. Complete Blood Count (CBC) with Five-Part Differential NHANES 2005–2006 Public Release Data Set Information This document details the Lab Protocol for testing the items listed in the following table: Lab Number Analyte SAS Label LBXWBCSI White blood cell count (SI) LBXLYPCT Lymphocyte (%) LBXMOPCT Monocyte (%) LBXNEPCT Segmented neutrophils (%) LBXEOPCT Eosinophils (%) LBXBAPCT Basophils (%) LBDLYMNO Lymphocyte number LBDMONO Monocyte number LBDNENO Segmented neutrophils number LBDEONO Eosinophils number CBC_d LBDBANO Basophils number LBXRBCSI Red cell count SI LBXHGB Hemoglobin (g/dL) LBXHCT Hematocrit (%) LBXMCVSI Mean cell volume (fL) LBXMCHSI Mean cell hemoglobin (pg) LBXMC MCHC (g/dL) LBXRDW Red cell distribution width (%) LBXPLTSI Platelet count (%) SI LBXMPSI Mean platelet volume (fL) Page 2 of 32 Complete Blood Count (CBC) with Five-Part Differential NHANES 2005–2006 1. Clinical Relevance and Summary of Test Principle Perform a complete blood count (CBC) in duplicate on all Sample Persons (SPs) age 1 and older. Perform the CBC on the Beckman Coulter MAXM. Run a CBC on home exam SP’s EDTA blood tubes after returning to the MEC. A. Purpose and Principle of Test The Beckman Coulter method of sizing and counting particles uses measurable changes in electrical resistance produced by nonconductive particles suspended in an electrolyte. -

In Asymptomatic Term Newborns at Risk for Sepsis, Is a Six-Hour CBC a Better Predictor of Sepsis Than a One-Hour CBC?
In asymptomatic term newborns at risk for sepsis, is a six-hour CBC a better predictor of sepsis than a one-hour CBC? Tori Treloar, R.N., B.S.N; Betsy Finley, R.N., B.S.N., M.P.H.; Audrey Nugent, R.N., B.S.N.; Lucy Schoemer, R.N., M.S.N.; Minshan Coudert, R.N., B.S.N. Background Neonatal sepsis is an invasive infection and remains one of the leading causes of Implications for Practice morbidity and mortality among both term and preterm infants (Shah, Padbury, 2014). The evidence is consistent in that well appearing The current practice at Inova Fairfax Medical Campus is to obtain a complete blood neonates at risk for sepsis should not receive a count (CBC) at one hour and again at 12 hours of life on all newborns at risk for sepsis. complete blood count (CBC) until at least six hours At one hour of life, there is normal decreased perfusion to limbs making it difficult to of life. Values obtained at or after six hours are obtain viable blood sample from a newborn. Multiple venous punctures are often more clinically useful as compared to those utilized to obtain the sample which can be distressing to parents and their newborns. obtained immediately after birth. New practice guidelines from CDC and the American Academy of Pediatrics (AAP) The evidence reviewed is consistent across all of support a CBC to be performed at 6-12 hours of life for low-risk, well-appearing the research and provides a compelling indication infants (Merck Manual, 2019). -
Complete Blood Count
ASSESSMENT OF HAEMATOLOGICAL PARAMETERS SOP: Measure - Complete Blood Count DEFINITION A Complete Blood Count (CBC) is a standardized test to assess components of the blood (e.g., red blood cells, white blood cells, hematocrit, hemoglobin, platelets). PURPOSE Complete Blood Count (CBC) tests are performed to determine the overall health of an individual and may help identify underlying conditions. CBC test results may identify a broad range of common and rare diseases. SCOPE This procedure applies to any research studies conducted by collaborators in the Sickle Pan African Research Consortium and the Sickle Africa Data Coordinating Centre (SADaCC) project. DESCRIPTION OF PROTOCOL The Complete Blood Count (CBC) protocol is a standard blood panel from the National Health and Nutrition Examination Survey (NHANES) and performed on participants aged 1 and older. Blood is collected from participants via standard venipuncture in a 3 or 4 ml K3 EDTA tube. The ambient blood sample is placed into a hematological analyzer for CBC and differential analyses. The blood should be tested as soon as possible after venipuncture and no later than 24 hours. SPECIFIC INSTRUCTION Blood should be drawn directly into an EDTA anticoagulated tube. Venipuncture is preferred rather than capillary blood draw although arterial blood may be used. The tube should be filled to the maximum volume stated. Although this assay specifies the Coulter® HMX Hematology Analyzer, there are a number of different assays and instruments that are appropriate to perform the CBC analyses. Commercial laboratories perform CBC tests routinely, and they are inexpensive. Blood should be analyzed according to the instrument manufacturer’s instructions and according to the laboratory’s standard operating procedure and interpreted in the context of age specific normal values. -

Blood and Immunity
Chapter Ten BLOOD AND IMMUNITY Chapter Contents 10 Pretest Clinical Aspects of Immunity Blood Chapter Review Immunity Case Studies Word Parts Pertaining to Blood and Immunity Crossword Puzzle Clinical Aspects of Blood Objectives After study of this chapter you should be able to: 1. Describe the composition of the blood plasma. 7. Identify and use roots pertaining to blood 2. Describe and give the functions of the three types of chemistry. blood cells. 8. List and describe the major disorders of the blood. 3. Label pictures of the blood cells. 9. List and describe the major disorders of the 4. Explain the basis of blood types. immune system. 5. Define immunity and list the possible sources of 10. Describe the major tests used to study blood. immunity. 11. Interpret abbreviations used in blood studies. 6. Identify and use roots and suffixes pertaining to the 12. Analyse several case studies involving the blood. blood and immunity. Pretest 1. The scientific name for red blood cells 5. Substances produced by immune cells that is . counteract microorganisms and other foreign 2. The scientific name for white blood cells materials are called . is . 6. A deficiency of hemoglobin results in the disorder 3. Platelets, or thrombocytes, are involved in called . 7. A neoplasm involving overgrowth of white blood 4. The white blood cells active in adaptive immunity cells is called . are the . 225 226 ♦ PART THREE / Body Systems Other 1% Proteins 8% Plasma 55% Water 91% Whole blood Leukocytes and platelets Formed 0.9% elements 45% Erythrocytes 10 99.1% Figure 10-1 Composition of whole blood. -

Provider Compliance Tips for Laboratory Tests-Blood Counts
Print-Friendly Version Fact Sheet Provider Compliance Tips for Laboratory Tests – Blood Counts What’s Changed? Updated information to include 2020 data. You’ll find substantive content updates in dark red font. Introduction This publication educates providers on proper documentation and billing for blood count laboratory tests. Provider Types Affected Physicians and non-physician practitioners (NPPs) who write requisitions or orders for blood count laboratory tests. Page 1 of 3 MLN909481 January 2021 Provider Compliance Tips for Laboratory Tests – Blood Counts MLN Fact Sheet Background The complete blood count (CBC) is a common laboratory test that includes a hemogram and differential white blood count (WBC). The hemogram includes a count of red blood cells, WBC, and platelets, as well as the finding of hemoglobin, hematocrit, and indicators. The Medicare Fee-for-Service (FFS) improper payment rate for blood count lab tests for the 2020 reporting period is 11.1% with a projected improper payment amount of $28.1 million. Reasons for Denial For the 2020 reporting period, insufficient documentation accounted for 86.4% of improper payments for lab tests. Blood counts and incorrect coding accounted for 13.6% of improper payments. How to Prevent Denials • You (the physician or NPP) who consult or treat a patient for a specific medical problem and use the test results to manage the patient’s medical problem must order the laboratory tests. Tests you don’t order for treating the patient aren’t reasonable and necessary. • Keep documents of medical necessity for services you order in the patient’s medical record. • The entity sending the claim must keep documents from you that show the correct processing of the order, submission of the claim, and diagnostic or other medical information you supplied to the laboratory, including any ICD-10-CM code or narrative description. -

Guideline for Complete Blood Count in Medical Laboratories: Effects of Preanalytical Parameters
Guideline for Complete Blood Count in Medical Laboratories: Effects of Preanalytical Parameters Prepared by the Turkish Biochemical Society Preanalytical Phase Working Group. 2020-ANKARA ISBN: 978-605-70111-0-7 Guideline for Complete Blood Count in Medical Laboratories: Effects of Preanalytical Parameters Prepared by the Turkish Biochemical Society Preanalytical Phase Working Group. 2020-Ankara ISBN: 978- 605-70111- 0 -7 Published by Turkish Biochemical Society Hirfanlı Sokak 9/3 G.O.P. Çankaya/Ankara Tel: 0 312 447 09 97 Fax: 0 312 447 09 63 Publication Year 2020 All rights are reserved. Any part of this book cannot be reproduced, kept electronically, copied neither electronically nor photographically and cannot be published in any way without written permission. PREPARED BY Fehime Benli Aksungar Fatma Demet Arslan Esin Avcı Güzin Aykal Cihan Coşkun İpek Çınaroğlu Ayfer Çolak Pınar Eker Funda Güçel Alper Gümüş Aylin Haklıgör Berrin Berçik İnal Bağnu Orhan Çiğdem Sönmez Mehmet Şeneş Fatma Taneli Canan Yılmaz CONTENT Abbreviations ........................................................................................................ 8 1. INTRODUCTION ............................................................................................... 9 2. GENERAL INFORMATION ................................................................................ 9 2.1. Structure and Cellular Components of Blood ...........................................9 2.2. Development of Complete Blood Count Method ...................................14 3. PRINCIPLES -

Cbc (Complete Blood Count) with Diff
CBC (COMPLETE BLOOD COUNT) WITH DIFF The CBC, also known as a Complete Blood Count, is a test that provides information about certain cells in the blood. It is a very common and important test that is frequently ordered by a physician to check a patient’s general health status. The CBC is a panel of tests which includes: WBC (White Blood (Leukocyte) Cell Count) ‐ a count of the actual number of white blood cells per volume of blood. White blood cells protect the body against infection and their numbers can quickly increase when a person has a bacterial infection. Both increases and decreases can be significant. WBC types include: Neutrophils, Bands (young neutrophils), Lymphocytes, Monocytes, Eosinophils, and Basophils. RBC (Red Blood Cell Count) ‐ a count of the actual number of red blood cells per volume of blood. If the RBC count is low, the body may not be getting the oxygen it needs. If the RBC count is too high (polycythemia) it may cause thickening of the blood, which could increase the risk for blood clots. Hemoglobin ‐ measures the amount of oxygen‐carrying protein in the blood. Hemoglobin is what gives blood its red color. Hematocrit ‐ is the percentage of red blood cells in the blood. For example, a hematocrit of 36 means that 36% of the blood's volume is made of red blood cells. Hematocrit and hemoglobin values can show if anemia or polycythemia is present. MCV (Mean Corpuscular Volume) ‐ indicates size of red blood cell, MCH (Mean Corpuscular Hemoglobin) ‐ indicates amount of hemoglobin in an average red blood cell, MCHC (Mean corpuscular hemoglobin concentration) ‐ measures the concentration of hemoglobin in a red blood cell. -
Your Guide to Anemia
YOUR GUIDE TO Anemia Healthy AnemiaLifestyle Changes Prevent n Treat n Control Iron-Deficiency Anemia Pernicious Anemia Aplastic Anemia Hemolytic Anema YOUR GUIDE TO Anemia Healthy AnemiaLifestyle Changes Prevent n Treat n Control Iron-Deficiency Anemia Pernicious Anemia Aplastic Anemia Hemolytic Anema NIH Publication No. 11-7629 September 2011 Contents Introduction . 1 . Anemia . .2 What Is Anemia? . 2 What Causes Anemia? . 4 Making Too Few Red Blood Cells . .5 Destroying Too Many Red Blood Cells . 6 Losing Too Many Red Blood Cells . 7 Signs and Symptoms of Anemia . 8 Diagnosing Anemia . 10 Medical and Family Histories . 10 Physical Exam . 11 Tests and Procedures . 11 Treating Anemia . 14 Types of Anemia . 16 . Iron-Deficiency Anemia . 16 What Is Iron-Deficiency Anemia and What Causes It? . 17 Who Is At Risk for Iron-Deficiency Anemia? . 19 What Are the Signs and Symptoms of Iron-Deficiency Anemia? . 24 How Is Iron-Deficiency Anemia Diagnosed? . 25 . How Is Iron-Deficiency Anemia Treated? . 26 Pernicious Anemia . 28 What Is Pernicious Anemia and What Causes It? . .28 . Who Is At Risk for Pernicious Anemia? . 29 What Are the Signs and Symptoms of Pernicious Anemia? .30 How Is Pernicious Anemia Diagnosed? . .32 How Is Pernicious Anemia Treated? . 33 Aplastic Anemia . 34 What Is Aplastic Anemia and What Causes It? . .34 Who Is At Risk for Aplastic Anemia? . 36 What Are the Signs and Symptoms of Aplastic Anemia? . 36 How Is Aplastic Anemia Diagnosed? . .37 Contents How Is Aplastic Anemia Treated? . 38 Hemolytic Anemia . 41 What Is Hemolytic Anemia and What Causes It? . 41 Who Is At Risk for Hemolytic Anemia? .