Understanding Your Complete Blood Count
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Blood, Lymph, and Immunity Joann Colville
Blood, Lymph, and Immunity Joann Colville CHAPTER OUTLINE .»: BLOOD Function Introduction Lymphatic Structures Plasma THE IMMUNE SYSTEM Cellular Components of Blood Function Red Blood Cells Immune Reactions Platelets Immunization: Protection Against Disease White Blood Cells THE LYMPHATICSYSTEM Lymph Formation Characteristics LEARNING OBJECTIVES • List and describe the functions of blood • List the functions of the lymphatic system • Describe the composition of blood plasma • Describe the structure and functions of the lymph nodes, • Describe the characteristics of mature erythrocytes spleen, thymus, tonsils, and GALT Describe the structure of the hemoglobin molecule and • List the functions of the immune system explain the fate of hemoglobin following intravascular and • Differentiate between specific and nonspecific immune extravascular hemolysis reactions • Give the origin of thrombocytes and describe their • Differentiate between cell-mediated and humoral immunity characteristics and functions • List the components involved in cell-mediated immunity • Listthe types of leukocytes and describe the functions of each and explain the role of each • Describe the formation of lymph fluid and its circulation List and describe the classes of immunoglobulins through the lymphatic system • Differentiate between active and passive immunity BLOOD vessels of the cardiovascular system. It has three main func- tions: transportation, regulation, and defense. INTRODUCTION Blood. Say the word, and some people cringe, others faint, Function and if you believe authors Bram Stoker, Stephen King, and 1. Blood is a transport system. Christopher Moore (all authors of vampire books), others • It carries oxygen, nutrients, and other essential com- drool. But no matter what you think about blood, animals pounds to every living cell in the body. -

White Blood Cells and Severe COVID-19: a Mendelian Randomization Study
Journal of Personalized Medicine Article White Blood Cells and Severe COVID-19: A Mendelian Randomization Study Yitang Sun 1 , Jingqi Zhou 1,2 and Kaixiong Ye 1,3,* 1 Department of Genetics, Franklin College of Arts and Sciences, University of Georgia, Athens, GA 30602, USA; [email protected] (Y.S.); [email protected] (J.Z.) 2 School of Public Health, Shanghai Jiao Tong University School of Medicine, Shanghai 200025, China 3 Institute of Bioinformatics, University of Georgia, Athens, GA 30602, USA * Correspondence: [email protected]; Tel.: +1-706-542-5898; Fax: +1-706-542-3910 Abstract: Increasing evidence shows that white blood cells are associated with the risk of coronavirus disease 2019 (COVID-19), but the direction and causality of this association are not clear. To evaluate the causal associations between various white blood cell traits and the COVID-19 susceptibility and severity, we conducted two-sample bidirectional Mendelian Randomization (MR) analyses with summary statistics from the largest and most recent genome-wide association studies. Our MR results indicated causal protective effects of higher basophil count, basophil percentage of white blood cells, and myeloid white blood cell count on severe COVID-19, with odds ratios (OR) per standard deviation increment of 0.75 (95% CI: 0.60–0.95), 0.70 (95% CI: 0.54–0.92), and 0.85 (95% CI: 0.73–0.98), respectively. Neither COVID-19 severity nor susceptibility was associated with white blood cell traits in our reverse MR results. Genetically predicted high basophil count, basophil percentage of white blood cells, and myeloid white blood cell count are associated with a lower risk of developing severe COVID-19. -

WHITE BLOOD CELLS Formation Function ~ TEST YOURSELF
Chapter 9 Blood, Lymph, and Immunity 231 WHITE BLOOD CELLS All white blood cells develop in the bone marrow except Any nucleated cell normally found in blood is a white blood for some lymphocytes (they start out in bone marrow but cell. White blood cells are also known as WBCs or leukocytes. develop elsewhere). At the beginning of leukopoiesis all the When white blood cells accumulate in one place, they grossly immature white blood cells look alike even though they're appear white or cream-colored. For example, pus is an accu- already committed to a specific cell line. It's not until the mulation of white blood cells. Mature white blood cells are cells start developing some of their unique characteristics larger than mature red blood cells. that we can tell them apart. There are five types of white blood cells. They are neu- Function trophils, eosinophils, basophils, monocytes and lymphocytes (Table 9-2). The function of all white blood cells is to provide a defense White blood cells can be classified in three different ways: for the body against foreign invaders. Each type of white 1. Type of defense function blood cell has its own unique role in this defense. If all the • Phagocytosis: neutrophils, eosinophils, basophils, mono- white blood cells are functioning properly, an animal has a cytes good chance of remaining healthy. Individual white blood • Antibody production and cellular immunity: lympho- cell functions will be discussed with each cell type (see cytes Table 9-2). 2. Shape of nucleus In providing defense against foreign invaders, the white • Polymorphonuclear (multilobed, segmented nucleus): blood cells do their jobs primarily out in the tissues. -

The Diagnosis of Paroxysmal Nocturnal Hemoglobinuria: Role of Flow Cytometry
THE DIAGNOSIS OF PAROXYSMAL NOCTURNAL HEMOGLOBINURIA: ROLE OF FLOW CYTOMETRY Alberto Orfao Department of Medicine, Cancer Research Centre (IBMCC-CSIC/USAL), University of Salamanca, Salamanca, Spain Paroxysmal nocturnal hemoglobinuria (PNH) on one or multiple populations of peripheral blood is an acquired clonal disorder typically affecting red cells and/or leucocytes of PNH patients, this young adults, which involves the phosphatidylino- translating into a new diagnostic test. Because sitol glycan anchor biosynthesis class A gene of this flow cytometry became an essential tool (PIGA) coded in chromosome X, in virtually every in the diagnosis of PNH. In turn, it could be also case. The altered gene encodes for a defective pro- demonstrated that investigation of the presence of tein product, the pig-a enzyme which is involved GPI-deficient cells among circulating mature neu- in the early steps of the synthesis of glycosylphos- trophils and monocytes, increases the sensitivity phatidylinositol (GPI). This later molecule (GPI) of red blood cell screening because of the shorter acts as an anchor of a wide range of proteins to lifetime of both populations of leucocytes. Despite the cell surface. At present a large number of GPI- all the above, routine assessment of CD55 and anchor associated proteins have been described CD59 is also associated with several limitations which are expressed by one or multiple distinct due to distinct patterns of expression among dif- compartments of hematopoietic cells. The altered ferent cell populations, dim and heterogeneous PIGA gene leads to an altered GPI anchor which expression among normal individuals and the lack leads to defective expression of GPI-AP on the of experience in many labs as regards the normal cytoplasmic membrane, on the cell surface. -

Human Physiology an Integrated Approach
Gas Exchange and Transport Gas Exchange in the Lungs and Tissues 18 Lower Alveolar P Decreases Oxygen Uptake O2 Diff usion Problems Cause Hypoxia Gas Solubility Aff ects Diff usion Gas Transport in the Blood Hemoglobin Binds to Oxygen Oxygen Binding Obeys the Law of Mass Action Hemoglobin Transports Most Oxygen to the Tissues P Determines Oxygen-Hb Binding O2 Oxygen Binding Is Expressed As a Percentage Several Factors Aff ect Oxygen-Hb Binding Carbon Dioxide Is Transported in Three Ways Regulation of Ventilation Neurons in the Medulla Control Breathing Carbon Dioxide, Oxygen, and pH Infl uence Ventilation Protective Refl exes Guard the Lungs Higher Brain Centers Aff ect Patterns of Ventilation The successful ascent of Everest without supplementary oxygen is one of the great sagas of the 20th century. — John B. West, Climbing with O’s , NOVA Online (www.pbs.org) Background Basics Exchange epithelia pH and buff ers Law of mass action Cerebrospinal fl uid Simple diff usion Autonomic and somatic motor neurons Structure of the brain stem Red blood cells and Giant liposomes hemoglobin of pulmonary Blood-brain barrier surfactant (40X) From Chapter 18 of Human Physiology: An Integrated Approach, Sixth Edition. Dee Unglaub Silverthorn. Copyright © 2013 by Pearson Education, Inc. All rights reserved. 633 Gas Exchange and Transport he book Into Thin Air by Jon Krakauer chronicles an ill- RUNNING PROBLEM fated trek to the top of Mt. Everest. To reach the summit of Mt. Everest, climbers must pass through the “death zone” T High Altitude located at about 8000 meters (over 26,000 ft ). Of the thousands of people who have attempted the summit, only about 2000 have been In 1981 a group of 20 physiologists, physicians, and successful, and more than 185 have died. -

Section 8: Hematology CHAPTER 47: ANEMIA
Section 8: Hematology CHAPTER 47: ANEMIA Q.1. A 56-year-old man presents with symptoms of severe dyspnea on exertion and fatigue. His laboratory values are as follows: Hemoglobin 6.0 g/dL (normal: 12–15 g/dL) Hematocrit 18% (normal: 36%–46%) RBC count 2 million/L (normal: 4–5.2 million/L) Reticulocyte count 3% (normal: 0.5%–1.5%) Which of the following caused this man’s anemia? A. Decreased red cell production B. Increased red cell destruction C. Acute blood loss (hemorrhage) D. There is insufficient information to make a determination Answer: A. This man presents with anemia and an elevated reticulocyte count which seems to suggest a hemolytic process. His reticulocyte count, however, has not been corrected for the degree of anemia he displays. This can be done by calculating his corrected reticulocyte count ([3% × (18%/45%)] = 1.2%), which is less than 2 and thus suggestive of a hypoproliferative process (decreased red cell production). Q.2. A 25-year-old man with pancytopenia undergoes bone marrow aspiration and biopsy, which reveals profound hypocellularity and virtual absence of hematopoietic cells. Cytogenetic analysis of the bone marrow does not reveal any abnormalities. Despite red blood cell and platelet transfusions, his pancytopenia worsens. Histocompatibility testing of his only sister fails to reveal a match. What would be the most appropriate course of therapy? A. Antithymocyte globulin, cyclosporine, and prednisone B. Prednisone alone C. Supportive therapy with chronic blood and platelet transfusions only D. Methotrexate and prednisone E. Bone marrow transplant Answer: A. Although supportive care with transfusions is necessary for treating this patient with aplastic anemia, most cases are not self-limited. -

Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant
Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease Bone Marrow (Stem Cell) Transplant for Sickle Cell Disease 1 Produced by St. Jude Children’s Research Hospital Departments of Hematology, Patient Education, and Biomedical Communications. Funds were provided by St. Jude Children’s Research Hospital, ALSAC, and a grant from the Plough Foundation. This document is not intended to take the place of the care and attention of your personal physician. Our goal is to promote active participation in your care and treatment by providing information and education. Questions about individual health concerns or specifi c treatment options should be discussed with your physician. For more general information on sickle cell disease, please visit our Web site at www.stjude.org/sicklecell. Copyright © 2009 St. Jude Children’s Research Hospital How did bone marrow (stem cell) transplants begin for children with sickle cell disease? Bone marrow (stem cell) transplants have been used for the treatment and cure of a variety of cancers, immune system diseases, and blood diseases for many years. Doctors in the United States and other countries have developed studies to treat children who have severe sickle cell disease with bone marrow (stem cell) transplants. How does a bone marrow (stem cell) transplant work? 2 In a person with sickle cell disease, the bone marrow produces red blood cells that contain hemoglobin S. This leads to the complications of sickle cell disease. • To prepare for a bone marrow (stem cell) transplant, strong medicines, called chemotherapy, are used to weaken or destroy the patient’s own bone marrow, stem cells, and infection fi ghting system. -

Apheresis Donation This Quick Reference Guide Will Help You Identify the Best Donation for Your Unique Blood Type
Apheresis Donation This quick reference guide will help you identify the best donation for your unique blood type. Donors now have the opportunity to make an apheresis (ay-fur-ee-sis) donation and donate just platelets, red cells, or plasma at blood drives. These individual components are vital for local patients in need. Platelets Control Bleeding Red Cells Deliver Oxygen Plasma transports blood cells & controls bleeding Donation Type Blood Types Requirements Donation Time A+, B+, O+ Over 75% of population has one of these blood types. Platelet Donation: Be healthy, weigh at least 114 lbs 2 hours cancer & surgery patients no aspirin for 48 hours Platelets only last five days after donation so the need is constant. O-, O+, A-, B- Special height, weight, Double Red: O-Negative is the 1 hour and hematocrit requirements. surgery, trauma patients, universal red cell donor. +25 min Please call us or see a staff member accident, & burn victims Only 17% of population has one of these negative blood types Plasma: AB+, AB- Trauma patients, burn Universal Plasma Donors 1 hour Be healthy, weigh at least 114 lbs victims, & patients with +30 min serious illness or injuries Only 4% of population How Apheresis works: Blood is drawn from the donor’s arm and the components are separated. Only the components being donated are collected while the remaining components are safely returned to the donor How to Schedule an Appointment: Please call 800-398-7888 or visit schedule.bloodworksnw.org. Walk-ins are also welcome at some blood drives, so be sure to ask our staff when you stop in. -

A Rapid and Quantitative D-Dimer Assay in Whole Blood and Plasma on the Point-Of-Care PATHFAST Analyzer ARTICLE in PRESS
MODEL 6 TR-03106; No of Pages 7 ARTICLE IN PRESS Thrombosis Research (2007) xx, xxx–xxx intl.elsevierhealth.com/journals/thre REGULAR ARTICLE A rapid and quantitative D-Dimer assay in whole blood and plasma on the point-of-care PATHFAST analyzer Teruko Fukuda a,⁎, Hidetoshi Kasai b, Takeo Kusano b, Chisato Shimazu b, Kazuo Kawasugi c, Yukihisa Miyazawa b a Department of Clinical Laboratory Medicine, Teikyo University School of Medical Technology, 2-11-1 Kaga, Itabashi, Tokyo 173-8605, Japan b Department of Central Clinical Laboratory, Teikyo University Hospital, Japan c Department of Internal Medicine, Teikyo University School of Medicine, Japan Received 11 July 2006; received in revised form 7 December 2006; accepted 28 December 2006 KEYWORDS Abstract The objective of this study was to evaluate the accuracy indices of the new D-Dimer; rapid and quantitative PATHFAST D-Dimer assay in patients with clinically suspected Deep-vein thrombosis; deep-vein thrombosis (DVT). Eighty two consecutive patients (34% DVT, 66% non-DVT) Point-of-care testing; with suspected DVT of a lower limb were tested with the D-Dimer assay with a Chemiluminescent PATHFAST analyzer. The diagnostic value of the PATHFAST D-Dimer assay (which is immunoassay based on the principle of a chemiluminescent enzyme immunoassay) for DVT was evaluated with pre-test clinical probability, compression ultrasonography (CUS). Furthermore, each patient underwent contrast venography and computed tomogra- phy, if necessary. The sensitivity and specificity of the D-Dimer assay using 0.570 μg/ mL FEU as a clinical cut-off value was found to be 100% and 63.2%, respectively, for the diagnosis of DVT, with a positive predictive value (PPV) and negative predictive value (NPV) of 66.7% and 100%, respectively. -
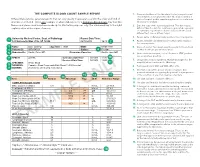
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -
Myelodysplastic Syndromes Overview and Types
cancer.org | 1.800.227.2345 About Myelodysplastic Syndromes Overview and Types If you have been diagnosed with a myelodysplastic syndrome or are worried about it, you likely have a lot of questions. Learning some basics is a good place to start. ● What Are Myelodysplastic Syndromes? ● Types of Myelodysplastic Syndromes Research and Statistics See the latest estimates for new cases of myelodysplastic syndromes in the US and what research is currently being done. ● Key Statistics for Myelodysplastic Syndromes ● What's New in Myelodysplastic Syndrome Research? What Are Myelodysplastic Syndromes? Myelodysplastic syndromes (MDS) are conditions that can occur when the blood- forming cells in the bone marrow become abnormal. This leads to low numbers of one or more types of blood cells. MDS is considered a type of cancer1. Normal bone marrow 1 ____________________________________________________________________________________American Cancer Society cancer.org | 1.800.227.2345 Bone marrow is found in the middle of certain bones. It is made up of blood-forming cells, fat cells, and supporting tissues. A small fraction of the blood-forming cells are blood stem cells. Stem cells are needed to make new blood cells. There are 3 main types of blood cells: red blood cells, white blood cells, and platelets. Red blood cells pick up oxygen in the lungs and carry it to the rest of the body. These cells also bring carbon dioxide back to the lungs. Having too few red blood cells is called anemia. It can make a person feel tired and weak and look pale. Severe anemia can cause shortness of breath. White blood cells (also known as leukocytes) are important in defending the body against infection. -

Patient Information Leaflet – Plasma Exchange Procedure
Therapeutic Apheresis Services Patient Information Leaflet – Plasma Exchange Procedure Introduction Antibodies, which normally help to protect you from infection, can begin to attack your own This leaflet has been written to give patients healthy cells, or an over production of proteins can information about plasma exchange (sometimes cause your blood to become thicker and slow down called plasmapheresis). If you would like any more the blood flow throughout your body. A plasma information or have any questions, please ask the exchange can help improve your symptoms, doctors and nurses involved in your treatment at although this may not happen immediately. the NHS Blood and Transplant (NHSBT) Therapeutic Apheresis Services Unit. Although plasma exchange may help with symptoms, it will not normally cure your condition When you have considered the information given as it does not switch off the production of the in this leaflet, and after we have discussed the harmful antibodies or proteins. It is likely that procedure and its possible risks with you, we will this procedure will form only one part of your ask you to sign a consent form to indicate that you treatment. are happy for the procedure to go ahead. Before any further procedures we will again check that you are happy to proceed. How do we perform Plasma Exchange? What is a plasma exchange? Plasma exchange is performed using a machine Blood is made up of red cells, white cells and called a Blood Cell Separator which can separate platelets which are carried around in fluid called blood into its various parts. The machine separates plasma.