Section 8: Hematology CHAPTER 47: ANEMIA
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

PATHOLOGY RESIDENT HEMATOLOGY ROTATION (North Florida/South Georgia Veterans Health Care System): Rotation Director: William L
PATHOLOGY RESIDENT HEMATOLOGY ROTATION (North Florida/South Georgia Veterans Health Care System): Rotation Director: William L. Clapp, M.D., Chief, Hematology Section, Gainesville VAMC; Consultants: Neil S. Harris, M.D., Director, Laboratory Hematology/Coagulation, University of Florida and Shands Hospital and Raul C. Braylan, M.D., Director, Hematopathology, University of Florida and Shands Hospital 1. Description of the Rotation: In this rotation, the resident will gain experience in laboratory hematology, which will include (1) peripheral blood studies to evaluate a variety of hematologic disorders, including anemias, lymphoproliferative and myeloproliferative disorders and leukemias. The emphasis on a multidisciplinary approach to diagnose hematologic disorders (including correlation of the peripheral blood studies with bone marrow and lymph node studies) provides an opportunity for the resident to also gain additional experience in (2) traditional histopathology, (3) immunohistochemistry, (4) electron microscopy, (5) protein electrophoresis, (6) flow cytometry, (7) cytogenetics and (8) molecular genetics which may be performed on the peripheral blood, bone marrow or lymph nodes of patients. The residents will acquire valuable experience by independently performing some bone marrow procedures. In addition, the resident will gain experience in coagulation testing. The residents will become familiar with the instrumentation in the hematology laboratory, including the operating principles and trouble-shooting (medical knowledge). The availability of assembled case study sets and reading materials (medical knowledge) will enhance the resident’s experience. Participation in CAP surveys, continuing education and hematology conferences is a component of the rotation (practice-based learning). Management issues and computer applications will be discussed (practice-based learning). As appropriate to the individual case or consultation under review, the ethical, socioeconomic, medicolegal and cost-containment issues will be reviewed and discussed. -

Pancytopenia; Study for Clinical Features and Etiological Pattern at Tertiary Care Settings in Abbottabad
The Professional Medical Journal www.theprofesional.com ORIGINAL PROF-2253 PANCYTOPENIA; STUDY FOR CLINICAL FEATURES AND ETIOLOGICAL PATTERN AT TERTIARY CARE SETTINGS IN ABBOTTABAD Dr. Atif Sitwat Hayat1, Dr. Abdul Haque Khan2, Dr. Ghulam Hussian Baloch3, Dr.Naila Shaikh4 1. MBBS, M.D (Medicine) Assistant Professor of Medicine, ABSTRACT... Background: Pancytopenia is an important hematological problem encountered Isra University Hospital, Hala Road in our day-to-day clinical practice. The aim of our study was to evaluate clinical features and Hyderabad, Sind, Pakistan. 2. MBBS, FCPS (Medicine) etiological pattern of pancytopenia at tertiary care settings in Abbottabad. Methods: This Associate Professor of Medicine prospective study was conducted at Northern Institue of Medical Sciences (NIMS) and Ayub Liaquat University of Medical and Health Sciences Jamshoro, Sind, Pakistan. Teaching Hospital Abbottabad from 25th August 2009 to 31st July 2010. A total of 85 patients 3. MBBS, Dip Card, M.D (Medicine) fulfilling the criteria of pancytopenia were randomly selected by time-based sampling. Associate Professor of Medicine Pancytopenia was diagnosed by anemia (hemoglobin ≤ 10.0g/dl), leucopenia (WBC ≤ 4.0×109/L) Liaquat University of Medical and 9 Health Sciences Jamshoro, Sind, Pakistan. and thrombocytopenia (platelets ≤ 150×10 /L). All data has been entered and analyzed by SPSS 4. MBBS, DCP version 10.0. Results: Out of 85 patients, 62(72.94%) were males and 23(27.05%) females with Senior Lecturer, Liaquat University of Medical and M to F ratio of 2.69:1. The mean age (±SD) of males was 30.20±15.42 years, while that of females Health Sciences Jamshoro, Sind, Pakistan. -
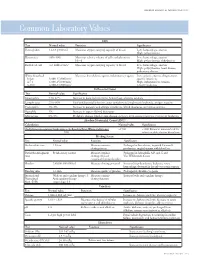
Common Laboratory Values
AmericAn AcAdemy of PediAtric dentistry Reference Manual 2006-2007 Resource Section 251 Common LaboratoryCommon Values Laboratory Values CBC Test Normal value Function Significance Hemoglobin 12-18 g/100 mL Measures oxygen carrying capacity of blood Low: hemorrhage, anemia High: polycythemia Hematocrit 35%-50% Measures relative volume of cells and plasma in Low: hemorrhage, anemia blood High: polycythemia, dehydration Red blood cell 4-6 million/mm3 Measures oxygen-carrying capacity of blood Low: hemorrhage, anemia High: polycythemia, heart disease, pulmonary disease White blood cell Measures host defense against inflammatory agents Low: aplastic anemia, drug toxicity, Infant 8,000-15,000/mm3 specific infections 4-7 y 6,000-15,000/mm3 High: inflammation, trauma, 8-18 y 4,500-13,500/mm3 toxicity, leukemia Differential Count Test Normal value Significance Neutrophils 54%-62% Increase in bacterial infections, hemorrhage, diabetic acidosis Lymphocytes 25%-30% Viral and bacterial infection, acute and chronic lymphocytic leukemia, antigen reaction Eosinophils 1%-3% Increase in parasitic and allergic conditions, blood dyscrasias, pernicious anemia Basophils 1% Increase in types of blood dyscrasias Monocytes 0%-9% Hodgkin’s disease, lipid storage disease, recovery from severe infections, monocytic leukemia Absolute Neutrophil Count (ANC) Calculation Normal value Significance (% Polymorphonuclear Leukocytes + % Bands)×Total White Cell Count >1500 <1000 Patient at increased risk for 100 infection; defer elective dental care Bleeding Screen Test -

Method Development and Validation of Vitamin D2 and Vitamin D3 Using Mass Spectrometry
Method Development and Validation of Vitamin D2 and Vitamin D3 Using Mass Spectrometry Devon Victoria Riley A thesis submitted in partial fulfillment of the requirements for the degree of Master of Science University of Washington 2016 Committee: Andrew Hoofnagle Geoffrey Baird Dina Greene Program Authorized to Offer Degree: Laboratory Medicine ©Copyright 2016 Devon V. Riley ii University of Washington Abstract Method Development and Validation of Vitamin D2 and Vitamin D3 Using Mass Spectrometry Devon V. Riley Chair of the Supervisory Committee: Associate Professor Andrew Hoofnagle, MD, PhD Vitamin D has long been known to maintain bone health by regulating calcium and phosphorous homeostasis. In recent years, scientists have discovered additional physiological roles for vitamin D. The complex interaction between the active vitamin D hormone and its metabolic precursors continues to be a rich area of research. Fundamental to this research is the availability of accurate and precise assays. Few published assays for vitamins D2 and D3 have contained sufficient details on method validation or performance characteristics. The liquid chromatography-tandem mass spectrometry (LC-MS/MS) assay developed for this thesis has undergone a rigorous validation and proven to yield a sensitive and specific method that exceeds the capabilities of all previously published methods. Developing and validating a novel assay is often complicated by the lack of established acceptability standards. This thesis explores this challenge, specifically for establishing meaningful interpretations and qualification standards of the lower limit of the measuring interval. Altogether, future research focused on vitamins D2, D3 and the Vitamin D pathway can benefit from this robust LC-MS/MS assay and the associated quality parameters outlined in this thesis. -

Acquired Hemophilia A: Pathogenesis and Treatment
Bleeding disorders Acquired hemophilia A: pathogenesis and treatment P.W. Collins ABSTRACT Arthur Bloom Haemophilia Centre, Acquired hemophilia A is an autoimmune disease caused by an inhibitory antibody to factor VIII. The School of Medicine, severity of bleeding varies but patients remain at risk of life-threatening bleeding until the inhibitor Cardiff University, Heath Park, has been eradicated. The cornerstones of management are rapid and accurate diagnosis, control of Cardiff, UK bleeding, investigation for an underlying cause, and eradication of the inhibitor by immunosuppres - sion. Patients should be managed jointly with a specialist center even if they present without signifi - cant bleeding. Despite an extensive literature, few controlled data are available and management Hematology Education: guidelines are based on expert opinion. Recombinant factor VIIa and activated prothrombin complex the education program for the concentrate are equally efficacious for treating bleeds and both are superior to factor VIII or desmo - annual congress of the European pressin. Immunosuppression should be started as soon as the diagnosis is made. Commonly used reg - Hematology Association imens are steroids alone or combined with cytotoxic agents. Rituximab is being used more commonly but current evidence does not suggest that it improves outcomes or reduces side effects. 2012;6:65-72 Introduction Pathogenesis Acquired hemophilia A (AHA) is a bleed - AHA is associated with autoimmune dis - ing disorder caused by polyclonal IgG1 and eases, such as rheumatoid arthritis, polymyal - IgG4 autoantibodies to the factor VIII ( FVIII ) gia rheumatic, and systemic lupus erythe - A2 and C2 domain. Morbidity and mortality matosis; malignancy; pregnancy and dermato - are high secondary to age, underlying dis - logical disorders, such as pemphigoid. -

A Distant Gene Deletion Affects Beta-Globin Gene Function in an Atypical Gamma Delta Beta-Thalassemia
A distant gene deletion affects beta-globin gene function in an atypical gamma delta beta-thalassemia. P Curtin, … , A D Stephens, H Lehmann J Clin Invest. 1985;76(4):1554-1558. https://doi.org/10.1172/JCI112136. Research Article We describe an English family with an atypical gamma delta beta-thalassemia syndrome. Heterozygosity results in a beta-thalassemia phenotype with normal hemoglobin A2. However, unlike previously described cases, no history of neonatal hemolytic anemia requiring blood transfusion was obtained. Gene mapping showed a deletion that extended from the third exon of the G gamma-globin gene upstream for approximately 100 kilobases (kb). The A gamma-globin, psi beta-, delta-, and beta-globin genes in cis remained intact. The malfunction of the beta-globin gene on a chromosome in which the deletion is located 25 kb away suggests that chromatin structure and conformation are important for globin gene expression. Find the latest version: https://jci.me/112136/pdf A Distant Gene Deletion Affects ,8-Globin Gene Function in an Atypical '6y5-Thalassemia Peter Curtin, Mario Pirastu, and Yuet Wai Kan Howard Hughes Medical Institute and Department ofMedicine, University of California, San Francisco, California 94143 John Anderson Gobert-Jones Department ofPathology, West Suffolk County Hospital, Bury St. Edmunds IP33-2QZ, Suffolk, England Adrian David Stephens Department ofHaematology, St. Bartholomew's Hospital, London ECIA-7BE, England Herman Lehmann Department ofBiochemistry, University ofCambridge, Cambridge CB2-lQW, England Abstract tologic picture of f3-thalassemia minor in adult life. Globin syn- thetic studies reveal a ,3 to a ratio of -0.5, but unlike the usual We describe an English family with an atypical 'yS6-thalassemia fl-thalassemia heterozygote, the levels of HbA2 (and HbF) are syndrome. -

Anemia in Heart Failure - from Guidelines to Controversies and Challenges
52 Education Anemia in heart failure - from guidelines to controversies and challenges Oana Sîrbu1,*, Mariana Floria1,*, Petru Dascalita*, Alexandra Stoica1,*, Paula Adascalitei, Victorita Sorodoc1,*, Laurentiu Sorodoc1,* *Grigore T. Popa University of Medicine and Pharmacy; Iasi-Romania 1Sf. Spiridon Emergency Hospital; Iasi-Romania ABSTRACT Anemia associated with heart failure is a frequent condition, which may lead to heart function deterioration by the activation of neuro-hormonal mechanisms. Therefore, a vicious circle is present in the relationship of heart failure and anemia. The consequence is reflected upon the pa- tients’ survival, quality of life, and hospital readmissions. Anemia and iron deficiency should be correctly diagnosed and treated in patients with heart failure. The etiology is multifactorial but certainly not fully understood. There is data suggesting that the following factors can cause ane- mia alone or in combination: iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunc- tion. There is data suggesting the association among iron deficiency, inflammation, erythropoietin levels, prescribed medication, hemodilution, and medullar dysfunction. The main pathophysiologic mechanisms, with the strongest evidence-based medicine data, are iron deficiency and inflammation. In clinical practice, the etiology of anemia needs thorough evaluation for determining the best possible therapeutic course. In this context, we must correctly treat the patients’ diseases; according with the current guidelines we have now only one intravenous iron drug. This paper is focused on data about anemia in heart failure, from prevalence to optimal treatment, controversies, and challenges. (Anatol J Cardiol 2018; 20: 52-9) Keywords: anemia, heart failure, intravenous iron, ferric carboxymaltose, quality of life Introduction g/dL in men) (2). -

Prolonged Partial Thromboplastin Time Without Bleeding History; Fletcher Factor Deficiency
Prolonged Partial Thromboplastin Time Without Bleeding History; Fletcher Factor Deficiency Celalettin ÜSTÜN*, Anand JILLELLA*, Linda HENDRIKS*, Mary JONAH**, Ferdane KUTLAR*, Russell BURGESS*, Abdullah KUTLAR* * Section of Hematology Oncology, Department of Medicine, Medical College of Georgia, ** Department of Pathology, Medical College of Georgia, Augusta, USA ABSTRACT A 67-year-old patient was admitted to the hospital to perform an esophagogastrectomy because a lesion at the lower esophagus was strongly suspicious for cancer. Her medical history and her family his- tory were negative for bleeding tendency or thrombosis. Her activated partial thromboplastin time (aPTT) was prolonged (44 s) whereas her prothrombin time (PT) was normal (11 s) presurgery. Mixing of her plasma with normal plasma corrected her prolonged aPTT (27.9 s). Prolonged incubation shortened the patient’s aPTT (36.3 s). Fletcher factor activity was found to be 50%. The patient underwent an esopha- gogastrectomy without bleeding complications under spinal anesthesia. Fletcher factor deficiency, a ra- re disorder, should be considered in patients who have no history of bleeding tendency with a prolonged aPTT. Surgical interventions are safe in these patients. Key Words: aPTT, Surgery, Fletcher factor, Prekallikrein. Turk J Haematol 2002;19(3): 417-419 Received: 20.06.2001 Accepted: 28.07.2001 INTRODUCTION unt[2]. Hematologists are frequently consulted for preoperative coagulation abnormalities. Preoperative evaluation of hemostasis is cru- cial to assess the risk of per-and peri-operative Prolonged aPTT is not an uncommon abnor- bleeding. The most effective screening method is mality encountered during preoperative evaluati- to obtain a thorough history of bleeding[1]. on. It may indicate the presence of antiphospholi- Preoperative screening tests mostly include acti- pid antibodies or a factor deficiency in the intrinsic vated partial thromboplastin time (aPTT), proth- and/or common pathways of blood coagulation. -

A Rapid and Quantitative D-Dimer Assay in Whole Blood and Plasma on the Point-Of-Care PATHFAST Analyzer ARTICLE in PRESS
MODEL 6 TR-03106; No of Pages 7 ARTICLE IN PRESS Thrombosis Research (2007) xx, xxx–xxx intl.elsevierhealth.com/journals/thre REGULAR ARTICLE A rapid and quantitative D-Dimer assay in whole blood and plasma on the point-of-care PATHFAST analyzer Teruko Fukuda a,⁎, Hidetoshi Kasai b, Takeo Kusano b, Chisato Shimazu b, Kazuo Kawasugi c, Yukihisa Miyazawa b a Department of Clinical Laboratory Medicine, Teikyo University School of Medical Technology, 2-11-1 Kaga, Itabashi, Tokyo 173-8605, Japan b Department of Central Clinical Laboratory, Teikyo University Hospital, Japan c Department of Internal Medicine, Teikyo University School of Medicine, Japan Received 11 July 2006; received in revised form 7 December 2006; accepted 28 December 2006 KEYWORDS Abstract The objective of this study was to evaluate the accuracy indices of the new D-Dimer; rapid and quantitative PATHFAST D-Dimer assay in patients with clinically suspected Deep-vein thrombosis; deep-vein thrombosis (DVT). Eighty two consecutive patients (34% DVT, 66% non-DVT) Point-of-care testing; with suspected DVT of a lower limb were tested with the D-Dimer assay with a Chemiluminescent PATHFAST analyzer. The diagnostic value of the PATHFAST D-Dimer assay (which is immunoassay based on the principle of a chemiluminescent enzyme immunoassay) for DVT was evaluated with pre-test clinical probability, compression ultrasonography (CUS). Furthermore, each patient underwent contrast venography and computed tomogra- phy, if necessary. The sensitivity and specificity of the D-Dimer assay using 0.570 μg/ mL FEU as a clinical cut-off value was found to be 100% and 63.2%, respectively, for the diagnosis of DVT, with a positive predictive value (PPV) and negative predictive value (NPV) of 66.7% and 100%, respectively. -

Evaluation of Prolonged Surface Activated Coagulation Time
Biomedical Science Faculty of Health and Society Malm¨oUniversity SE-205 06 Malm¨o Sweden Master programme in Biomedical Surface Science http://edu.mah.se/en/Program/VABSE Evaluation of prolonged surface activated coagulation time Master degree thesis, 30 ECTS Author: Amalie Jesting Supervisors: Sebastian Bj¨orklund,PhD, Lecturer, Malm¨oUniversity Jens Peter Gøtze, MD, DMSc Professor, Chief-Physician, Rigshospitalet Søren Frank Jørgensen, MSc, Senior Lecturer, Metropolitan University College August 2018 MALMO¨ UNIVERSITY Abstract Faculty of Health and Society Master programme in Biomedical Surface Science Evaluation of prolonged surface activated coagulation time by Amalie Jesting Background: Blood coagulation is an essential defense mechanism to prevent bleeding. Disorders in the coagulation system can be severe and blood tests measuring the blood's ability to coagulate are important. Activated partial thromboplastin time (APTT) is a blood test that measures blood coagulation time. An abnormal prolonged APTT can both be associated with a bleeding tendency or a risk of thrombosis. Additional blood tests are needed to discover the cause of a prolonged APTT. One potential test is the APTT mixing study, which can separate samples with and without inhibitors. The aim of this project is to investigate how the cause of a prolonged APTT is evaluated today and to examine if it is possible to indicate the cause of a prolonged APTT using the APTT mixing study performed on routine samples. The goal is to be able to indicate the cause of a prolonged APTT immediately when is it first discovered. This will save time and help guide the physicians in their work with the patient. -
Introduction to Hematological Assessment (PDF)
UPDATED 01/2021 Introduction to Hematological Assessment Objectives After completing this lesson, you will be able to: • State the main purposes of a hematological assessment. • Explain the procedures for collecting and processing a blood sample. • Understand the importance of hand washing. • Understand the importance of preventing blood borne pathogen transmission. • Describe and follow the hemoglobin test procedure using the Hemocue Hemoglobin Analyzer. Overview The most common form of nutritional deficiency is “iron deficiency”. It is observed more frequently among children and women of childbearing age (particularly pregnant women). Iron deficiency can result in developmental delays and behavioral disturbance in children, as well as increased risk for a preterm delivery in pregnant women. Iron status can be determined using several different types of laboratory tests. The two tests most commonly used to screen for iron deficiency are hemoglobin (Hgb) concentration and hematocrit (Hct). Proper screening for iron deficiency requires sound laboratory methods and procedures. Often, CPAs will hear the following questions: “Do you have to stick my finger? What does this have to do with my WIC foods anyway? Will it hurt?” For most of us, the thought of having blood taken, even from a finger, is not pleasant. However, evaluating the results of a blood test is a part of screening for nutritional risk. Why Does WIC Require Hematological Assessment? WIC requires that each applicant be screened for risk of a medical condition known as iron deficiency anemia. Anemia is a condition of the blood in which the amount of hemoglobin falls below a level considered desirable for good health. -

The Hematological Complications of Alcoholism
The Hematological Complications of Alcoholism HAROLD S. BALLARD, M.D. Alcohol has numerous adverse effects on the various types of blood cells and their functions. For example, heavy alcohol consumption can cause generalized suppression of blood cell production and the production of structurally abnormal blood cell precursors that cannot mature into functional cells. Alcoholics frequently have defective red blood cells that are destroyed prematurely, possibly resulting in anemia. Alcohol also interferes with the production and function of white blood cells, especially those that defend the body against invading bacteria. Consequently, alcoholics frequently suffer from bacterial infections. Finally, alcohol adversely affects the platelets and other components of the blood-clotting system. Heavy alcohol consumption thus may increase the drinker’s risk of suffering a stroke. KEY WORDS: adverse drug effect; AODE (alcohol and other drug effects); blood function; cell growth and differentiation; erythrocytes; leukocytes; platelets; plasma proteins; bone marrow; anemia; blood coagulation; thrombocytopenia; fibrinolysis; macrophage; monocyte; stroke; bacterial disease; literature review eople who abuse alcohol1 are at both direct and indirect. The direct in the number and function of WBC’s risk for numerous alcohol-related consequences of excessive alcohol increases the drinker’s risk of serious Pmedical complications, includ- consumption include toxic effects on infection, and impaired platelet produc- ing those affecting the blood (i.e., the the bone marrow; the blood cell pre- tion and function interfere with blood cursors; and the mature red blood blood cells as well as proteins present clotting, leading to symptoms ranging in the blood plasma) and the bone cells (RBC’s), white blood cells from a simple nosebleed to bleeding in marrow, where the blood cells are (WBC’s), and platelets.