Cells, Tissues and Organs of the Immune System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Immunology New Orleans, LA Toll Free 888.355.4191 Toll Free Fax 888.355.4192 Krogerspecialtypharmacy.Com
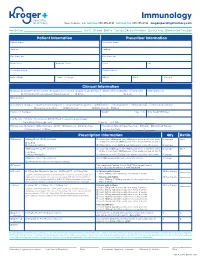
Immunology New Orleans, LA toll free 888.355.4191 toll free fax 888.355.4192 krogerspecialtypharmacy.com Need By Date: _________________________________________________ Ship To: Patient Office Fax Copy: Rx Card Front/Back Clinical Notes Medical Card Front/Back Patient Information Prescriber Information Patient Name Prescriber Name Address Address City State Zip City State Zip Main Phone Alternate Phone Phone Fax Social Security # Contact Person Date of Birth Male Female DEA # NPI # License # Clinical Information Diagnosis: J45.40 Moderate Asthma J45.50 Severe Asthma L20.9 Atopic Dermatitis L50.1 Chronic Idiopathic Urticaria (CIU) Eosinophil Levels J33 Chronic Rhinosinusitis with Nasal Polyposis Other: ________________________________ Dx Code: ___________ Drug Allergies Concomitant Therapies: Short-acting Beta Agonist Long-acting Beta Agonist Antihistamines Decongestants Immunotherapy Inhaled Corticosteroid Leukotriene Modifiers Oral Steroids Nasal Steroids Other: _____________________________________________________________ Please List Therapies Weight kg lbs Date Weight Obtained Lab Results: History of positive skin OR RAST test to a perennial aeroallergen Pretreatment Serum lgE Level: ______________________________________ IU per mL Test Date: _________ / ________ / ________ MD Specialty: Allergist Dermatologist ENT Pediatrician Primary Care Prescription Type: Naïve/New Start Restart Continued Therapy Pulmonologist Other: _________________________________________ Last Injection Date: _________ / ________ -

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -
IFM Innate Immunity Infographic
UNDERSTANDING INNATE IMMUNITY INTRODUCTION The immune system is comprised of two arms that work together to protect the body – the innate and adaptive immune systems. INNATE ADAPTIVE γδ T Cell Dendritic B Cell Cell Macrophage Antibodies Natural Killer Lymphocites Neutrophil T Cell CD4+ CD8+ T Cell T Cell TIME 6 hours 12 hours 1 week INNATE IMMUNITY ADAPTIVE IMMUNITY Innate immunity is the body’s first The adaptive, or acquired, immune line of immunological response system is activated when the innate and reacts quickly to anything that immune system is not able to fully should not be present. address a threat, but responses are slow, taking up to a week to fully respond. Pathogen evades the innate Dendritic immune system T Cell Cell Through antigen Pathogen presentation, the dendritic cell informs T cells of the pathogen, which informs Macrophage B cells B Cell B cells create antibodies against the pathogen Macrophages engulf and destroy Antibodies label invading pathogens pathogens for destruction Scientists estimate innate immunity comprises approximately: The adaptive immune system develops of the immune memory of pathogen exposures, so that 80% system B and T cells can respond quickly to eliminate repeat invaders. IMMUNE SYSTEM AND DISEASE If the immune system consistently under-responds or over-responds, serious diseases can result. CANCER INFLAMMATION Innate system is TOO ACTIVE Innate system NOT ACTIVE ENOUGH Cancers grow and spread when tumor Certain diseases trigger the innate cells evade detection by the immune immune system to unnecessarily system. The innate immune system is respond and cause excessive inflammation. responsible for detecting cancer cells and This type of chronic inflammation is signaling to the adaptive immune system associated with autoimmune and for the destruction of the cancer cells. -

Environments of Haematopoiesis and B-Lymphopoiesis in Foetal Liver K
Environments of haematopoiesis and B-lymphopoiesis in foetal liver K. Kajikhina1, M. Tsuneto1,2, F. Melchers1 1Max Planck Fellow Research Group ABSTRACT potent myeloid/lymphoid progenitors on “Lymphocyte Development”, In human and murine embryonic de- (MPP), and their immediate progeny, Max Planck Institute for Infection velopment, haematopoiesis and B-lym- common myeloid progenitors (CMP) Biology, Berlin, Germany; phopoiesis show stepwise differentia- and common lymphoid progenitors 2Department of Stem Cell and Developmental Biology, Mie University tion from pluripotent haematopoietic (CLP) soon thereafter (10). The first Graduate School of Medicine, Tsu, Japan. stem cells and multipotent progenitors, T- or B-lymphoid lineage-directed pro- Katja Kajikhina over lineage-restricted lymphoid and genitors appear at E12.5-13.5, for T- Motokazu Tsuneto, PhD myeloid progenitors to B-lineage com- lymphocytes in the developing thymus Fritz Melchers, PhD mitted precursors and finally differenti- (11), for B-lymphocytes in foetal liver Please address correspondence to: ated pro/preB cells. This wave of dif- (12). Time in development, therefore, Fritz Melchers, ferentiation is spatially and temporally separates and orders these different Max Planck Fellow Research Group organised by the surrounding, mostly developmental haematopoietic stages. on “Lymphocyte Development”, non-haematopoietic cell niches. We re- Three-dimensional imaging of progen- Max Planck Institute for Infection Biology, view here recent developments and our itors and precursors indicates that stem Chariteplatz 1, current contributions on the research D-10117 Berlin, Germany. cells are mainly found inside the em- E-mail: [email protected] on blood cell development. bryonic blood vessel, and are attracted Received and accepted on August 28, 2015. -

Thalassemia and the Spleen
Thalassemia and the Spleen 4 Living with Thalassemia are developing an infection (fever, chills, sore throats, unexplained coughs, listlessness, muscle pain, etc.) and Issues in Thalassemia report them to your doctor right away. Thalassemia Care • Sometimes a splenectomy can lead to an exceptionally and the Spleen high platelet count, which can in turn lead to blood clotting. by Marie B. Martin, RN, and Craig Butler Your doctor should monitor your platelet count on a regular basis and may ask you to take baby aspirin daily. This sounds kind of frightening. Is a splenectomy really a What is the spleen? wise choice? The spleen is a small organ (normally That’s a decision that must be made in each individual case. about the size of a fist) that lies in the A doctor with significant experience with thalassemia is upper left part of the abdomen, near going to be in the best position to offer advice about this; the stomach and below the ribcage. however, most people who are splenectomized are able to What does it do? manage the challenges it presents with relatively little The spleen has a number of functions, the most important of difficulty. which are filtering blood and creating lymphocytes. It also acts as a “reservoir” of blood, keeping a certain amount on Of course, it’s best to avoid any circumstances that can lead hand for use in emergencies. to the need for a splenectomy in the first place. For a person with thalassemia, this means following a transfusion In its filtering capacity, the spleen is able to remove large regimen that keeps hemoglobin levels above 9 or 10gm/dL. -

Regulate CD4 T Cell Responses Dependent Red Pulp Macrophages − CSF-1
CSF-1−Dependent Red Pulp Macrophages Regulate CD4 T Cell Responses Daisuke Kurotaki, Shigeyuki Kon, Kyeonghwa Bae, Koyu Ito, Yutaka Matsui, Yosuke Nakayama, Masashi Kanayama, This information is current as Chiemi Kimura, Yoshinori Narita, Takashi Nishimura, of September 29, 2021. Kazuya Iwabuchi, Matthias Mack, Nico van Rooijen, Shimon Sakaguchi, Toshimitsu Uede and Junko Morimoto J Immunol published online 14 January 2011 http://www.jimmunol.org/content/early/2011/01/14/jimmun Downloaded from ol.1001345 Supplementary http://www.jimmunol.org/content/suppl/2011/01/14/jimmunol.100134 Material 5.DC1 http://www.jimmunol.org/ Why The JI? Submit online. • Rapid Reviews! 30 days* from submission to initial decision • No Triage! Every submission reviewed by practicing scientists by guest on September 29, 2021 • Fast Publication! 4 weeks from acceptance to publication *average Subscription Information about subscribing to The Journal of Immunology is online at: http://jimmunol.org/subscription Permissions Submit copyright permission requests at: http://www.aai.org/About/Publications/JI/copyright.html Email Alerts Receive free email-alerts when new articles cite this article. Sign up at: http://jimmunol.org/alerts The Journal of Immunology is published twice each month by The American Association of Immunologists, Inc., 1451 Rockville Pike, Suite 650, Rockville, MD 20852 Copyright © 2011 by The American Association of Immunologists, Inc. All rights reserved. Print ISSN: 0022-1767 Online ISSN: 1550-6606. Published January 14, 2011, doi:10.4049/jimmunol.1001345 The Journal of Immunology CSF-1–Dependent Red Pulp Macrophages Regulate CD4 T Cell Responses Daisuke Kurotaki,*,† Shigeyuki Kon,† Kyeonghwa Bae,† Koyu Ito,† Yutaka Matsui,* Yosuke Nakayama,† Masashi Kanayama,† Chiemi Kimura,† Yoshinori Narita,‡ Takashi Nishimura,‡ Kazuya Iwabuchi,x Matthias Mack,{ Nico van Rooijen,‖ Shimon Sakaguchi,# Toshimitsu Uede,*,† and Junko Morimoto† The balance between immune activation and suppression must be regulated to maintain immune homeostasis. -

We Work at the Intersection of Immunology and Developmental Biology
Development and Homeostasis of Mucosal Tissues U934/UMR3215 – Genetics and Developmental Biology Pedro Hernández Chef d'équipe [email protected] We work at the intersection of immunology and developmental biology. Our primary goal is to understand how immune responses impact the development, integrity and function of mucosal tissue layers, such as the intestinal epithelium, during homeostasis and upon different types of stress, including infections. To study these questions we exploit the advantages of the zebrafish model such as ex utero and rapid development, transparency, large progeny, and simple genetic manipulation. We combine live imaging, flow cytometry, single-cell transcriptomics, and models inducing mucosal stress, including pathogenic challenges. Our research can be subdivided into three main topics: 1) Protection of intestinal epithelial integrity since early development: Epithelial cells are at the core of intestinal organ function. They are in charge of absorbing nutrients and water, and at the same time constitute a barrier for potential pathogens and harmful molecules. Epithelial cells perform all these functions before full development of the immune system, which promotes epithelial barrier function upon injury. We study how robust epithelial integrity is achieved prior and after maturation of the intestinal immune system, with a focus on the function of mucosal cytokines. 2) Epithelial-leukocyte crosstalk throughout development: Intestines become vastly populated by leukocytes after exposure to external cues from diet and colonization by the microbiota. We have recently reported the existence and diversity of zebrafish innate lymphoid cells (ILCs), a key component of the mucosal immune system recently discovered in mice and humans. ILCs mediate immune responses by secreting cytokines such as IL-22 which safeguards gut epithelial integrity. -

Immunology in Pediatric Dentistry
PEDIATRIC DENTISTRY/Copynght© 1983 by The American Academy of Pedodontics/Vol. 5, No. 3 Immunology in pediatric dentistry William C. Donlon, DMD, MA Abstract The scope of clinical immunology is ever- usually are directed against a specific allergen and this increasing. A working knowledge of the immune substance will always invoke the same type of response system and its disease states is important in the although the severity may vary. Another variable is evalution and treatment of pediatric dental patients. whether the reaction is localized or generalized. This review focuses both on immune conditions with The antibody type which initiates the histamine- a possible iatrogenic origin, such as allergy, and releasing immediate atopic reaction is IgE. Molecule immune phenomena which the pedodontist may dimers of IgE adhere to most cells and basophils causing diagnose or treat as part of the medical team. degranulation and subsequent increase in extracellular levels of vasodilators such as histamine, slow-reacting substance - A, and the kinins. Clinical symptoms are "ue to advances in the science of immunology, pa- cutaneous wheal and flare, edema, rhinorrhea, tearing, tients with defects of the immune system are being possible respiratory embarrassment, and hypotension diagnosed earlier and living longer. The condition and/or (Figure 1). treatment modality may affect the patient's oral health Antihistamines are the most effective treatment in mild and delivery of dental care. On a more mundane level, cases. Active therapy of allergy may include induction of the pedodontist deals with the immune system daily when IgG antibody synthesis by multiple injections of minute inquiring about allergies and rheumatic fever in the quantities of the allergen. -

An Essential Role of UBXN3B in B Lymphopoiesis Tingting Geng Et Al. This File Contains 9 Supplemental Figures and Legends
An Essential Role of UBXN3B in B Lymphopoiesis Tingting Geng et al. This file contains 9 supplemental figures and legends. a Viral load (relative) load Viral Serum TNF-α b +/+ Serum IL-6 Ubxn3b Ubxn3b-/- Ubxn3b+/+ 100 100 ** Ubxn3b-/- ** 10 10 IL-6 IL-6 (pg/ml) GM-CSF (pg/ml) GM-CSF 1 1 0 3 8 14 35 0 3 8 14 35 Time post infection (Days) Time post infection (Days) Serum IL-10 Serum CXCL10 Ubxn3b+/+ Ubxn3b-/- 10000 1000 +/+ -/- * Ubxn3b Ubxn3b 1000 100 IFN-γ (pg/ml) CXCL10 (pg/ml) CXCL10 100 10 0 3 8 14 35 0 3 8 14 35 Time post infection (Days) Time post infection (Days) IL-1β IL-1β (pg/ml) Supplemental Fig.s1 UBXN3B is essential for controlling SARS-CoV-2 pathogenesis. Sex- and-age matched littermates were administered 2x105 plaque forming units (PFU) of SARS-CoV-2 intranasally. a) Quantitative RT-PCR (qPCR) quantification of SARS-CoV-2 loads in the lung at days 3 and 10 post infection (p.i). Each symbol= one mouse, the small horizontal line: the median of the result. *, p<0.05; **, p<0.01, ***, p<0.001 (non-parametric Mann-Whitney test) between Ubxn3b+/+ and Ubxn3b-/- littermates at each time point. Ubxn3b+/+ Ubxn3b-/- Live Live 78.0 83.6 CD45+ CD45+ UV UV CD45 94.1 CD45 90.9 FSC-A FSC-A FSC-A FSC-A Mac Mac 23.0 38.1 MHC II MHC II CD11b Eso CD11b Eso 5.81 7.44 CD19, MHCII subset F4_80, CD11b subset CD19, MHCII subset F4_80, CD11b subset Myeloid panel Myeloid 70.1 65.6 94.2 51.1 CD19 F4/80 CD19 F4/80 Neu DC Neu DC 4.87 1.02 16.2 2.24 CD11b, Ly-6G subset CD11b, Ly-6G subset 94.9 83.3 Ly-6G Ly-6G MHC II MHC II CD11b CD11c CD11b CD11c Live Live 82.3 76.5 CD45+ CD45+ 91.1 91.3 UV UV CD45 CD45 FSC-A FSC-A FSC-A FSC-A Q1 Q2 Q1 Q2 Q1 Q2 Q1 Q2 Lymphoid panel Lymphoid 20.1 0.29 54.1 1.17 4.27 0.060 39.2 2.55 CD4 CD4 CD19 CD19 Q4 Q3 Q4 Q3 Q4 Q3 Q4 Q3 47.0 32.6 7.21 37.5 67.7 28.0 7.27 51.0 CD3 CD8 CD3 CD8 Supplemental Fig.s2 Dysregulated immune compartmentalization in Ubxn3b-/- lung. -

Our Immune System (Children's Book)
OurOur ImmuneImmune SystemSystem A story for children with primary immunodeficiency diseases Written by IMMUNE DEFICIENCY Sara LeBien FOUNDATION A note from the author The purpose of this book is to help young children who are immune deficient to better understand their immune system. What is a “B-cell,” a “T-cell,” an “immunoglobulin” or “IgG”? They hear doctors use these words, but what do they mean? With cheerful illustrations, Our Immune System explains how a normal immune system works and what treatments may be necessary when the system is deficient. In this second edition, a description of a new treatment has been included. I hope this book will enable these children and their families to explore together the immune system, and that it will help alleviate any confusion or fears they may have. Sara LeBien This book contains general medical information which cannot be applied safely to any individual case. Medical knowledge and practice can change rapidly. Therefore, this book should not be used as a substitute for professional medical advice. SECOND EDITION COPYRIGHT 1990, 2007 IMMUNE DEFICIENCY FOUNDATION Copyright 2007 by Immune Deficiency Foundation, USA. Readers may redistribute this article to other individuals for non-commercial use, provided that the text, html codes, and this notice remain intact and unaltered in any way. Our Immune System may not be resold, reprinted or redistributed for compensation of any kind without prior written permission from Immune Deficiency Foundation. If you have any questions about permission, please contact: Immune Deficiency Foundation, 40 West Chesapeake Avenue, Suite 308, Towson, MD 21204, USA; or by telephone at 1-800-296-4433. -

Osteopathic Approach to the Spleen
Osteopathic approach to the spleen Luc Peeters and Grégoire Lason 1. Introduction the first 3 years to 4 - 6 times the birth size. The position therefore progressively becomes more lateral in place of The spleen is an organ that is all too often neglected in the original epigastric position. The spleen is found pos- the clinic, most likely because conditions of the spleen do tero-latero-superior from the stomach, its arterial supply is not tend to present a defined clinical picture. Furthermore, via the splenic artery and the left gastroepiploic artery it has long been thought that the spleen, like the tonsils, is (Figure 2). The venous drainage is via the splenic vein an organ that is superfluous in the adult. into the portal vein (Figure 2). The spleen is actually the largest lymphoid organ in the body and is implicated within the blood circulation. In the foetus it is an organ involved in haematogenesis while in the adult it produces lymphocytes. The spleen is for the blood what the lymph nodes are for the lymphatic system. The spleen also purifies and filters the blood by removing dead cells and foreign materials out of the circulation The function of red blood cell reserve is also essential for the maintenance of human activity. Osteopaths often identify splenic congestion under the influence of poor diaphragm function. Some of the symptoms that can be associated with dysfunction of the spleen are: Figure 2 – Position and vascularisation of the spleen Anaemia in children Disorders of blood development Gingivitis, painful and bleeding gums Swollen, painful tongue, dysphagia and glossitis Fatigue, hyperirritability and restlessness due to the anaemia Vertigo and tinnitus Frequent colds and infections due to decreased resis- tance Thrombocytosis Tension headaches The spleen is also considered an important organ by the osteopath as it plays a role in the immunity, the reaction of the circulation and oxygen transport during effort as well as in regulation of the blood pressure. -

Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics
Immunology Stories: How Storytelling Can Help Us to Make Sense of Complex Topics Jennifer Giuliani, MSc Camosun College, Lansdowne Campus, 3100 Foul Bay Rd, Victoria BC V8P 5J2 [email protected] Abstract The immune response is a wonderfully complex aspect of our physiology that can sometimes confound students and instructors alike. How do we wade through the layers of detail to help our students develop an understanding of immunology? In this article, I will share some of the stories about immunology research that helped me strengthen my own understanding and improve my approach to helping students learn and understand this topic. In addition, we will explore some of the research on the power of storytelling, and how learning through stories might be a defining characteristic of what it means to be human. https://doi.org/10.21692/haps.2020.105 Key words: storytelling, immunology Introduction I have been trying to understand the immune response for a My personal journey to develop a better understanding of long time. Like many Anatomy and Physiology instructors, I the immune system was a compelling reminder to me of the did not have an immunology background beyond what was power of storytelling. Suddenly I saw examples of storytelling covered in my undergraduate physiology courses. When the everywhere that I saw authentic learning. In this article, I will time came for me to teach students about the immune system, share some of what I have learned about learning through I relied heavily on the information presented in our textbooks. stories, some of the fun and fascinating immunology stories I was able to present students with the key pieces of from Davis’ books, and my current approach to helping information and help them to remember a few facts, and the students understand the immune response.