The Complete Blood Count and Associated Tests Purpose Course
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

WHITE BLOOD CELLS Formation Function ~ TEST YOURSELF
Chapter 9 Blood, Lymph, and Immunity 231 WHITE BLOOD CELLS All white blood cells develop in the bone marrow except Any nucleated cell normally found in blood is a white blood for some lymphocytes (they start out in bone marrow but cell. White blood cells are also known as WBCs or leukocytes. develop elsewhere). At the beginning of leukopoiesis all the When white blood cells accumulate in one place, they grossly immature white blood cells look alike even though they're appear white or cream-colored. For example, pus is an accu- already committed to a specific cell line. It's not until the mulation of white blood cells. Mature white blood cells are cells start developing some of their unique characteristics larger than mature red blood cells. that we can tell them apart. There are five types of white blood cells. They are neu- Function trophils, eosinophils, basophils, monocytes and lymphocytes (Table 9-2). The function of all white blood cells is to provide a defense White blood cells can be classified in three different ways: for the body against foreign invaders. Each type of white 1. Type of defense function blood cell has its own unique role in this defense. If all the • Phagocytosis: neutrophils, eosinophils, basophils, mono- white blood cells are functioning properly, an animal has a cytes good chance of remaining healthy. Individual white blood • Antibody production and cellular immunity: lympho- cell functions will be discussed with each cell type (see cytes Table 9-2). 2. Shape of nucleus In providing defense against foreign invaders, the white • Polymorphonuclear (multilobed, segmented nucleus): blood cells do their jobs primarily out in the tissues. -
Automatic System for Differential Blood Counting
ISSN (Print) : 2320 – 3765 ISSN (Online): 2278 – 8875 International Journal of Advanced Research in Electrical, Electronics and Instrumentation Engineering (An ISO 3297: 2007 Certified Organization) Vol. 5, Issue 4, April 2016 Automatic System for Differential Blood Counting 1 2 Manisha Shirvoikar , Dr.H.G.Virani PG Student [ECI], Dept. of ETC, Goa College of Engineering, Ponda, Goa, India1 Professor & Head of Department, Dept. of ETC, Goa College of Engineering, Ponda, Goa, India2 ABSTRACT: For detecting various diseases, Doctor first suggests the patient to undergo blood test which is used as a health indicator. Differential Blood Count (DBC) provides haematologist with valuable information about health of the patient. DBC determines the percentage of types of WBC this is important because it give exact count of five types of WBC such as neutrophil, lymphocyte, monocyte, eosinophil and basophile. Increase or decrease of DBC than the ideal count indicated that our body is not healthy. Precise counting of type of WBC is very important. Manual counting of White blood cells is time consuming and can lead to human error with increase in number of samples. Automatic cell counter sometimes misclassifies the cells having different morphology. Even they are very expensive and unaffordable by remote area health centres and hospitals. These problems are overcome by developing a system which is image based, cost effective, fast and accurate which has the capability to identify, classify the different type of white blood cell and perform DBC. Implementation is done using MATLABR2014b. KEYWORDS: MATLAB, peripheral blood smear, RBC, Thresholding, WBC, DBC. I.INTRODUCTION Total volume of blood in human is 5-6 litres i.e 8% of body weight or 80 mL/kg body weight. -

Understanding the CBC
Understanding the CBC What is Hematology? Hematology is the science of blood and blood-forming tissues. Blood is made up of plasma and blood cells. Blood formation (hematopoesis) is a continuous process that occurs in the bone marrow. Within the bone marrow there is a pluripotent stem cell, the Mother Cell, the originator of all types of blood cells. The stem cell produces blood cells that exit the bone marrow and circulate in the blood system. Red cells circulate about four months, platelets last an average of ten days, and white cells range from only hours to a week or so. Stem cells that are found outside the bone marrow are called “peripheral stem cells” and are collected and frozen for stem cell transplants. What is a CBC? The CBC- the complete blood count, or the counts- is a lab test that will be ordered frequently on your child. This test determines the number, type, percentage, concentration and quality of the various types of blood cells that make up the blood. This test can be completed on blood that is collected by a finger stick, a lab draw from a central vein access and/or a straight draw from a peripheral vein, (usually from an arm, hand or foot). The CBC is commonly performed on an automated analyzer. However when abnormalities are noted in the blood, parts of the test can be completed manually. That is when the blood sample is viewed under the microscope. Some institutions commonly perform an extensively complete CBC and others may perform just specific aspects of the CBC. -
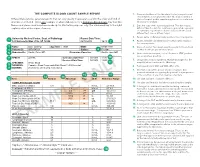
The Complete Blood Count Sample Report 1
THE COMPLETE BLOOD COUNT SAMPLE REPORT 1. Name and address of the lab where the test was performed. Tests may be run in a physician office lab, a lab located in a Different laboratories generate reports that can vary greatly in appearance and in the order and kind of The Complete Blood Count Sample Report clinic or hospital, and/or samples may be sent to a reference information included. This is one example of what a lab report for a Complete Blood Count may look like. laboratory for analysis. NamesDifferent and laboratories places used generate have been reports made that up can for vary illustrative greatly inpurposes appearance only. andThe innumbered the order keyand tokind the of right 2. Date this copy of the report was printed. This date may be explainsinformation a few included. of the reportThis is elements.one exampl e of what a lab report for a Complete Blood Count may look like. different than the date the results were generated, especially Names and places used have been made up for illustrative purposes only. Point your cursor at a number on cumulative reports (those that include results of several to learn about the different report elements. different tests run on different days). 3. Patient name or identifier. Links results to the correct person. 1 University Medical Center, Dept. of Pathology Report Date/Time: 123 University Way, City, ST 12345 02/10/2014 16:40 2 4. Patient identifier and identification number. Links results to the correct person. 3 Name: Doe, John Q. Age/Sex: 73/M DOB: 01/01/1941 5. -

Azathioprine and Mercaptopurine Therapy
Patient & Family Guide 2021 Azathioprine and Mercaptopurine Therapy www.nshealth.ca Azathioprine and Mercaptopurine Therapy Your health care provider feels that treatment with azathioprine (a-za-THY-o-preen) (Imuran®) or mercaptopurine (mur-CAP-toe-pure-een) (6-MP) may help you manage an over-active immune response. This pamphlet will help you decide if this medication is right for you. It describes what azathioprine is, how it works, and possible side effects. What are azathioprine (AZA) and mercaptopurine (6-MP)? • The cells in your immune system fight infection and inflammation (swelling). • If your immune system is over-active, it can can cause inflammation and damage to body tissues and organs. • Diseases that cause an over-active immune response are: › Rheumatoid arthritis › Inflammatory bowel disease (IBD), such as Crohn’s disease and ulcerative colitis › Certain forms of liver disease • AZA is an immunosuppressive medication. It suppresses (weakens) the immune response, which lowers inflammation. 1 • 6-MP is very similar to AZA. It works much the same way, but your body breaks it down in a different way. This makes it less likely to cause nausea (feeling sick to your stomach) and vomiting (throwing up). 6-MP costs more than azathioprine. If you have nausea or vomiting when taking AZA, talk to your health care provider. How well does AZA work? Will it work for me? • AZA, when used alone, helps to control diseases that cause an over-active immune response in many people, including IBD. • Take this medication as told by your doctor. This increases the chance that it will work well. -
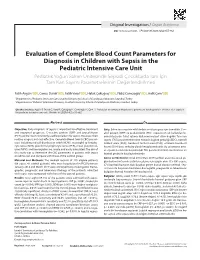
Evaluation of Complete Blood Count Parameters for Diagnosis In
Original Investigation / Özgün Araştırma DOI: 10.5578/ced.68886 • J Pediatr Inf 2020;14(2):e55-e62 Evaluation of Complete Blood Count Parameters for Diagnosis in Children with Sepsis in the Pediatric Intensive Care Unit Pediatrik Yoğun Bakım Ünitesinde Sepsisli Çocuklarda Tanı İçin Tam Kan Sayımı Parametrelerinin Değerlendirilmesi Fatih Aygün1(İD), Cansu Durak1(İD), Fatih Varol1(İD), Haluk Çokuğraş2(İD), Yıldız Camcıoğlu2(İD), Halit Çam1(İD) 1 Department of Pediatric Intensive Care, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey 2 Department of Pediatric Infectious Diseases, Istanbul University School of Cerrahpasa Medicine, Istanbul, Turkey Cite this article as: Aygün F, Durak C, Varol F, Çokuğraş H, Camcıoğlu Y, Çam H. Evaluation of complete blood count parameters for diagnosis in children with sepsis in the pediatric intensive care unit. J Pediatr Inf 2020;14(2):e55-e62. Abstract Öz Objective: Early diagnosis of sepsis is important for effective treatment Giriş: Erken tanı sepsiste etkili tedavi ve iyi prognoz için önemlidir. C-re- and improved prognosis. C-reactive protein (CRP) and procalcitonin aktif protein (CRP) ve prokalsitonin (PKT) sepsiste en sık kullanılan bi- (PCT) are the most commonly used biomarkers for sepsis. However, their yobelirteçlerdir. Fakat rutinde kullanımı maliyet etkin değildir. Tam kan routine usage is not cost-effective. Complete Blood Count (CBC) param- sayımı (TKS) parametrelerinden eritrosit dağılım genişliği (EDG), nötrofil eters including red cell distribution width (RDW), neutrophil to lympho- lenfosit oranı (NLO), trombosit lenfosit oranı (TLO), ortalama trombosit cyte ratios (NLR), platelet to lymphocyte ratios (PLR), mean platelet vol- hacmi (OTH) basit ve kolay olarak hesaplanmaktadır. Bu çalışmanın ama- ume (MPV), and hemoglobin are simple and easily calculated. -

Digitalcommons@UNMC Granulocytopenia
University of Nebraska Medical Center DigitalCommons@UNMC MD Theses Special Collections 5-1-1936 Granulocytopenia Howard E. Mitchell University of Nebraska Medical Center This manuscript is historical in nature and may not reflect current medical research and practice. Search PubMed for current research. Follow this and additional works at: https://digitalcommons.unmc.edu/mdtheses Part of the Medical Education Commons Recommended Citation Mitchell, Howard E., "Granulocytopenia" (1936). MD Theses. 457. https://digitalcommons.unmc.edu/mdtheses/457 This Thesis is brought to you for free and open access by the Special Collections at DigitalCommons@UNMC. It has been accepted for inclusion in MD Theses by an authorized administrator of DigitalCommons@UNMC. For more information, please contact [email protected]. G PA~lULOCYTOPENI A SENIOR THESIS By Howard E. Mitchell April 17, 1936 TABLE OF CONT'ENTS Introduction Definition • · 1 History . • • • 1 Nomenclature • • • • • 4 ClassificBtion • • • • 6 Physiology • • • • .10 Etiology • • 22 Geographic Distribution • 23 Age, Sex, and R9ce • • ·• 23 Occupation • .. • • • • .. • 23 Ba.cteria • • • • .. 24 Glandu18.r Dysfunction • • • 27 Radiation • • • • 28 Allergy • • • 28 Chemotactic and Maturation Factors • • 28 Chemicals • • • • • 30 Pathology • • • • • 36 Symptoms • • • • • • • 43 DiEtgnosis • • • • • .. • • • • • .. • 4'7 Prognosis 48 '" • • • • • • • • • • • • Treatment • • • • • • • • 49 Non"'specific Therapy • • • • .. 50 Transfusion • • • • .. 51 X-Ray • • • • • • • • • 52 Liver ·Extract • • • • • • • 53 Nucleotides • • • • • • • • • • • 53 General Ca.re • • • • • • • • 57 Conclusion • • • • • • • • • 58 480805 INTHODUCTION Although t~ere is reference in literature of the Nineteenth Century to syndromes similating the disease (granulocytopenia) 9.8 W(~ know it todes, it "vas not un til the year 1922 that Schultz 8ctually described his C8se as a disease entity and by so doing, stimulated the interest of tne medical profession to further in vestigation. -

Bone Marrow Suppression (Myelosuppression) and Leukopenia/Neutropenia
Effects on the Hematopoietic System: Bone Marrow Suppression (Myelosuppression) and Leukopenia/Neutropenia Effects on the Hematopoietic System: Bone Marrow Suppression (Myelosuppression) and Leukopenia/Neutropenia Author: Ayda G. Nambayan, DSN, RN, St. Jude Children’s Research Hospital Erin Gafford, Pediatric Oncology Education Student, St. Jude Children’s Research Hospital; Nursing Student, School of Nursing, Union University Content Reviewed by: Monika Metzger, MD, St. Jude Children’s Research Hospital Cure4Kids Release Date: 6 June 2006 Leukopenia is a decrease in the absolute number of white blood cells, whereas neutropenia is the condition in which the absolute neutrophil count (ANC) is either < 500/mm3 or <1000/mm3 with a predictable decline to <500/mm3 in 24 to 48 hours. Leukopenia and neutropenia can be caused by cancer or by myelosuppression secondary to therapy (chemotherapy and radiation therapy). Infection is the most common complication associated with neutropenia and the major cause of morbidity and mortality in neutropenic patients with cancer. Important determinants of the risk of infection include the number of circulating neutrophils and the duration of the neutropenia. The lower the number of circulating neutrophils is and the longer the neutropenia lasts, the higher the incidence and the more severe the infections are. Children and adolescents with severe neutropenia (ANC< 500/mm3) are at risk of life- threatening bacterial, fungal and viral infections. If the patient has febrile neutropenia (A – 1), surveillance cultures and more blood tests should be conducted to determine whether infection is present and, if it is, where it is located. Assessment Patient assessment must include a careful history and physical examination. -

Severe Myelotoxicity Associated with Thiopurine S-Methyltransferase*3A
Case Report DOI: 10.4274/tjh.2013.0082 Severe Myelotoxicity Associated with Thiopurine S-Methyltransferase*3A/*3C Polymorphisms in a Patient with Pediatric Leukemia and the Effect of Steroid Therapy Pediatrik Bir Lösemi Olgusunda Tiyopurin S-Metiltransferaz *3A/*3C Polimorfizmi ile İlişkili Ağır Miyelotoksisite-Steroid Tedavisinin Etkisi Burcu Fatma Belen1, Türkiz Gürsel1, Nalan Akyürek2, Meryem Albayrak3, Zühre Kaya1, Ülker Koçak1 1Gazi University Faculty of Medicine, Department of Pediatric Hematology, Ankara, Turkey 2Gazi University Faculty of Medicine, Department of Pathology, Ankara, Turkey 3Kırıkkale University Faculty of Medicine, Department of Pediatric Hematology, Ankara, Turkey Abstract: Myelosuppression is a serious complication during treatment of acute lymphoblastic leukemia and the duration of myelosuppression is affected by underlying bone marrow failure syndromes and drug pharmacogenetics caused by genetic polymorphisms. Mutations in the thiopurine S-methyltransferase (TPMT) gene causing excessive myelosuppression during 6-mercaptopurine (MP) therapy may cause excessive bone marrow toxicity. We report the case of a 15-year-old girl with T-ALL who developed severe pancytopenia during consolidation and maintenance therapy despite reduction of the dose of MP to 5% of the standard dose. Prednisolone therapy produced a remarkable but transient bone marrow recovery. Analysis of common TPMT polymorphisms revealed TPMT *3A/*3C. Key Words: Myelosuppression, Thiopurine S-methyl transferase, Acute leukemia Özet: Miyelosupresyon, -

SEED Haematology Sysmex Educational Enhancement and Development October 2012
SEED Haematology Sysmex Educational Enhancement and Development October 2012 The red blood cell indices The full blood count has been used in conjunction with the traditional red The complete blood count (CBC) is central to clinical deci- cell indices in order to narrow down the possible causes sion making. This makes it one of the commonest laboratory of anaemia in an individual patient. investigations performed worldwide. Whilst the definition of what constitutes an CBC is influenced by the number Impedance technology and type of parameters measured by different haematology The RBC, HCT and MCV are all closely interrelated as they analysers, the traditional red cell indices that are widely are derived from information obtained from the passage used to classify anaemias are common to all. of cells through the aperture of the impedance channel of an automated haematology analyser. The impedance The laboratory approach to anaemia technology is based on the principle that an electrical field, Anaemia is an extremely common global healthcare prob- created between two electrodes of opposite charge, can lem. However, anaemia is merely a symptom which can be used to count and determine the size of cells. Blood result from a multitude of causes. Effective treatment is cells are poor conductors of electricity. The diluent in which only possible if the underlying cause is correctly identified. they are suspended as they pass through the aperture To this end, several classification systems have been devis- during counting is an isotonic solution which is a good ed. The most useful and widely used classification system conductor of electricity. -

Ingenuity Pathway Analysis of Human Facet Joint Tissues: Insight Into Facet Joint Osteoarthritis
EXPERIMENTAL AND THERAPEUTIC MEDICINE 19: 2997-3008, 2020 Ingenuity pathway analysis of human facet joint tissues: Insight into facet joint osteoarthritis CHU CHEN*, SHENGYU CUI*, WEIDONG LI, HURICHA JIN, JIANBO FAN, YUYU SUN and ZHIMING CUI Department of Spine Surgery, The Second Affiliated Hospital of Nantong University, Nantong, Jiangsu 226001, P.R. China Received August 17, 2019; Accepted January 30, 2020 DOI: 10.3892/etm.2020.8555 Abstract. Facet joint osteoarthritis (FJOA) is a common the top 5 IPA networks (with a score >30). The present study degenerative joint disorder with high prevalence in the elderly. provides insight into the pathological processes of FJOA from FJOA causes lower back pain and lower extremity pain, and a genetic perspective and may thus benefit the clinical treat- thus severely impacts the quality of life of affected patients. ment of FJOA. Emerging studies have focused on the histomorphological and histomorphometric changes in FJOA. However, the dynamic Introduction genetic changes in FJOA have remained to be clearly deter- mined. In the present study, previously obtained RNA deep Facet joint osteoarthritis (FJOA) is a common degenerative sequencing data were subjected to an ingenuity pathway joint disorder that causes the degeneration and breakdown analysis (IPA) and canonical signaling pathways of differ- of cartilage and restricts the movement of joints (1). It has entially expressed genes (DEGs) in FJOA were studied. The been reported that lumbar FJOA occurs at high prevalence top 25 enriched canonical signaling pathways were identified and the presence of FJOA is highly associated with age (2,3). and canonical signaling pathways with high absolute values A community-based cross-sectional study indicated that of z-scores, specifically leukocyte extravasation signaling, in populations aged <50 years, the prevalence of FJOA was Tec kinase signaling and osteoarthritis pathway, were inves- <45%, while it was ~75% in populations aged >50 years (4). -

Laboratory Approach to Anemia Laboratory Approach to Anemia
DOI: 10.5772/intechopen.70359 Provisional chapter Chapter 12 Laboratory Approach to Anemia Laboratory Approach to Anemia Ebru Dündar Yenilmez and Abdullah Tuli Ebru Dündar Yenilmez and Abdullah Tuli Additional information is available at the end of the chapter Additional information is available at the end of the chapter http://dx.doi.org/10.5772/intechopen.70359 Abstract Anemia is a major cause of morbidity and mortality worldwide and can be defined as a decreased quantity of circulating red blood cells (RBCs). The epidemiological studies suggested that one-third of the world’s population is affected with anemia. Anemia is not a disease, but it is instead the sign of an underlying basic pathological process. However, the sign may function as a compass in the search for the cause. Therefore, the prediag- nosis revealed by thorough investigation of this sign should be supported by laboratory parameters according to the underlying pathological process. We expect that this review will provide guidance to clinicians with findings and laboratory tests that can be followed from the initial stage in the anemia search. Keywords: anemia, complete blood count, red blood cell indices, reticulocyte 1. Introduction Anemia, the meaning of which in Greek is “without blood,” is a relatively common sign and symptom of various medical conditions. Anemia is defined as a significant decrease in the count of total erythrocyte [red blood cell (RBC)] mass, although this definition is rarely used in clinical settings. According to the World Health Organization, anemia is a condition in which the number of red blood cells (RBCs, and consequently their oxygen-carrying capacity) is insufficient to meet the body’s physiologic needs [1, 2].