E. Coli Sequence Types (Sts) Were Identified Including Unknown As Well As Sts Frequently Linked to Infectious Diseases
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Final Report on the Project
BP Conservation Programme (CLP) 2005 PROJECT NO. 101405 - BRONZE AWARD WINNER ECOLOGY, DISTRIBUTION, STATUS AND PROTECTION OF THREE CONGOLESE FRUIT BATS FINAL REPORT Patrick KIPALU Team Leader Observatoire Congolais pour la Protection de l’Environnement OCPE – ong Kinshasa – Democratic Republic of the Congo E-mail: [email protected] APRIL 2009 1 Table of Content Acknowledgements…………………………………………………………………. p3 I. Project Summary……………………………………………………………….. p4 II. Introduction…………………………………………………………………… p4-p7 III. Materials and Methods ……………………………………………………….. p7-p10 IV. Results per Study Site…………………………………………………………. p10-p15 1. Pointe-Noire ………………………………………………………….. p10-p12 2. Mayumbe Forest /Luki Reserve……………………………………….. p12-p13 3. Zongo Forest…………………………………………………………... p14 4. Mbanza-Ngungu ………………………………………………………. P15 V. General Results ………………………………………………………………p15-p16 VI. Discussions……………………………………………………………………p17-18 VII. Conclusion and Recommendations……………………………………….p 18-p19 VIII. Bibliography………………………………………………………………p20-p21 Acknowledgements 2 The OCPE (Observatoire Congolais pour la Protection de l’Environnement) project team would like to start by expressing our gratefulness and saying thank you to the BP Conservation Program, which has funded the execution of this project. The OCPE also thanks the Van Tienhoven Foundation which provided a further financial support. Without these organisations, execution of the project would not have been possible. We would like to thank specially the BPCP “dream team”: Marianne D. Carter, Robyn Dalzen and our regretted Kate Stoke for their time, advices, expertise and care, which helped us to complete this work, Our special gratitude goes to Dr. Wim Bergmans, who was the hero behind the scene from the conception to the execution of the research work. Without his expertise, advices and network it would had been difficult for the project team to produce any result from this project. -
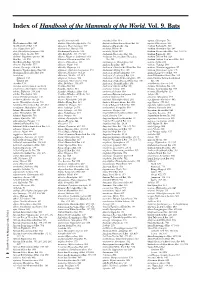
Index of Handbook of the Mammals of the World. Vol. 9. Bats
Index of Handbook of the Mammals of the World. Vol. 9. Bats A agnella, Kerivoula 901 Anchieta’s Bat 814 aquilus, Glischropus 763 Aba Leaf-nosed Bat 247 aladdin, Pipistrellus pipistrellus 771 Anchieta’s Broad-faced Fruit Bat 94 aquilus, Platyrrhinus 567 Aba Roundleaf Bat 247 alascensis, Myotis lucifugus 927 Anchieta’s Pipistrelle 814 Arabian Barbastelle 861 abae, Hipposideros 247 alaschanicus, Hypsugo 810 anchietae, Plerotes 94 Arabian Horseshoe Bat 296 abae, Rhinolophus fumigatus 290 Alashanian Pipistrelle 810 ancricola, Myotis 957 Arabian Mouse-tailed Bat 164, 170, 176 abbotti, Myotis hasseltii 970 alba, Ectophylla 466, 480, 569 Andaman Horseshoe Bat 314 Arabian Pipistrelle 810 abditum, Megaderma spasma 191 albatus, Myopterus daubentonii 663 Andaman Intermediate Horseshoe Arabian Trident Bat 229 Abo Bat 725, 832 Alberico’s Broad-nosed Bat 565 Bat 321 Arabian Trident Leaf-nosed Bat 229 Abo Butterfly Bat 725, 832 albericoi, Platyrrhinus 565 andamanensis, Rhinolophus 321 arabica, Asellia 229 abramus, Pipistrellus 777 albescens, Myotis 940 Andean Fruit Bat 547 arabicus, Hypsugo 810 abrasus, Cynomops 604, 640 albicollis, Megaerops 64 Andersen’s Bare-backed Fruit Bat 109 arabicus, Rousettus aegyptiacus 87 Abruzzi’s Wrinkle-lipped Bat 645 albipinnis, Taphozous longimanus 353 Andersen’s Flying Fox 158 arabium, Rhinopoma cystops 176 Abyssinian Horseshoe Bat 290 albiventer, Nyctimene 36, 118 Andersen’s Fruit-eating Bat 578 Arafura Large-footed Bat 969 Acerodon albiventris, Noctilio 405, 411 Andersen’s Leaf-nosed Bat 254 Arata Yellow-shouldered Bat 543 Sulawesi 134 albofuscus, Scotoecus 762 Andersen’s Little Fruit-eating Bat 578 Arata-Thomas Yellow-shouldered Talaud 134 alboguttata, Glauconycteris 833 Andersen’s Naked-backed Fruit Bat 109 Bat 543 Acerodon 134 albus, Diclidurus 339, 367 Andersen’s Roundleaf Bat 254 aratathomasi, Sturnira 543 Acerodon mackloti (see A. -

Updates to the Zoonotic Niche Map of Ebola Virus Disease in Africa
RESEARCH ADVANCE Updates to the zoonotic niche map of Ebola virus disease in Africa David M Pigott1,2*, Anoushka I Millear1, Lucas Earl1, Chloe Morozoff1*, Barbara A Han3, Freya M Shearer2, Daniel J Weiss4,5, Oliver J Brady2, Moritz UG Kraemer4,5, Catherine L Moyes2, Samir Bhatt4,5, Peter W Gething4,5, Nick Golding2,6, Simon I Hay1,2 1Institute for Health Metrics and Evaluation, University of Washington, Seattle, United States; 2Oxford Big Data Institute, Li Ka Shing Centre for Health Information and Discovery, Oxford, United Kingdom; 3Cary Institute of Ecosystem Studies, New York, United States; 4Spatial Ecology and Epidemiology Group, University of Oxford, Oxford, United Kingdom; 5Department of Zoology, University of Oxford, Oxford, United Kingdom; 6Department of BioSciences, University of Melbourne, Parkville, Australia Abstract As the outbreak of Ebola virus disease (EVD) in West Africa is now contained, attention is turning from control to future outbreak prediction and prevention. Building on a previously published zoonotic niche map (Pigott et al., 2014), this study incorporates new human and animal occurrence data and expands upon the way in which potential bat EVD reservoir species are incorporated. This update demonstrates the potential for incorporating and updating data used to generate the predicted suitability map. A new data portal for sharing such maps is discussed. This output represents the most up-to-date estimate of the extent of EVD zoonotic risk in Africa. These maps can assist in strengthening surveillance and response capacity to contain viral haemorrhagic fevers. DOI: 10.7554/eLife.16412.001 *For correspondence: pigottdm@ uw.edu (DMP); [email protected] (CM) Competing interest: See page 10 Introduction Since the index case in 2013, the West African Ebola epidemic has killed more than 11,000 people Funding: See page 10 (World Heath Organization, 2016) and exposed national and international inadequacies in pan- Received: 30 March 2016 demic preparedness and response (Moon et al., 2015). -

Monthly Report
Monthly Report April 2017 Nyika National Park. Photo credit Mike Langton The “refusing to write any more1 of Matt’s dumb reports” bat The ABC Staff Dr Emma Stone Matt Town Godwin Zimba Founder/Director Senior Research Assistant Community Engagement Officer Kathy Halsall Peter Phiri Jess Dangerfield Urban Research Assistant Research Assistant Research Assistant, LNP Rachel Midgley Kelly Rosier Urban Bat Research and Conservation Urban Field Assistant, Lilongwe Assistant, Lilongwe 1 Contents News from Nyika NP ................................................................................................................. 3 News from Nyika ........................................................................................................................... 3 New Species: Rousettus lanosus ................................................................................................. 3 First Vesper (A) Roost Discovered .............................................................................................. 3 Community Work in the Staff Village ......................................................................................... 4 Mzuzu Bat Hunter and Bat Meat Trade in the North ............................................................... 4 Urban Bat Project News ........................................................................................................... 5 Staff News ...................................................................................................................................... 5 Update -

Monthly Report
Monthly Report May 2019 Little epauletted fruit bat (Epomophorus labiatus ) Photo by: Emily Stanford The “refusing to write any more1 of Matt’s dumb reports” bat ABC Staff Dr Emma Stone Matt Town Madalitso “Mada” Mwaungulu Founder/Coordinator Research Manager Community and Outreach Officer Susan Eshelman Karen Shevlin Fay Taylor Research Assistant Entomologist, Projects Manager Research Assistant Sam Hay-Roe Dilly Hoyt Savanna Shafer Research Assistant Research Assistant Research Assistant 1 Contents ABC News……………………………………………………………………………………………..... 3 Student’s Experience on University of Sussex Field Course………………....………..…..……….. 3 Bat Team Return to Vwaza..………………………………………………………………..…………. 4 A View from a Volunteer………………………………………………………………………………. 5 Interesting finds during Urban BMPs ………………………………………………………..……… 6 ABC Project Species List ........................................................................................................ 7 Sponsors of ABC ...................................................................................................................... 9 2 ABC News ABC Host assessments. My project focused on dung University of Sussex Field Course and track transects along the floodplain. I really appreciated having the opportunity By: Rebecca O’Sullivan, CRA MSc Student to learn a new skill. I definitely hope to learn more about dung and track identification in the future. Despite doing separate projects, we also got involved in each other’s projects in order to gain a variety of experiences. One group was doing bat -

Diversity and Diversification Across the Global Radiation of Extant Bats
Diversity and Diversification Across the Global Radiation of Extant Bats by Jeff J. Shi A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy (Ecology and Evolutionary Biology) in the University of Michigan 2018 Doctoral Committee: Professor Catherine Badgley, co-chair Assistant Professor and Assistant Curator Daniel Rabosky, co-chair Associate Professor Geoffrey Gerstner Associate Research Scientist Miriam Zelditch Kalong (Malay, traditional) Pteropus vampyrus (Linnaeus, 1758) Illustration by Gustav Mützel (Brehms Tierleben), 19271 1 Reproduced as a work in the public domain of the United States of America; accessible via the Wikimedia Commons repository. EPIGRAPHS “...one had to know the initial and final states to meet that goal; one needed knowledge of the effects before the causes could be initiated.” Ted Chiang; Story of Your Life (1998) “Dr. Eleven: What was it like for you, at the end? Captain Lonagan: It was exactly like waking up from a dream.” Emily St. John Mandel; Station Eleven (2014) Bill Watterson; Calvin & Hobbes (October 27, 1989)2 2 Reproduced according to the educational usage policies of, and direct correspondence with Andrews McMeel Syndication. © Jeff J. Shi 2018 [email protected] ORCID: 0000-0002-8529-7100 DEDICATION To the memory and life of Samantha Jade Wang. ii ACKNOWLEDGMENTS All of the research presented here was supported by a National Science Foundation (NSF) Graduate Research Fellowship, an Edwin H. Edwards Scholarship in Biology, and awards from the University of Michigan’s Rackham Graduate School and the Department of Ecology & Evolutionary Biology (EEB). A significant amount of computational work was funded by a Michigan Institute for Computational Discovery and Engineering fellowship; specimen scanning, loans, and research assistants were funded by the Museum of Zoology’s Hinsdale & Walker fund and an NSF Doctoral Dissertation Improvement Grant. -

Han EEID Filo-Chiro.Pptx
Photo:%Hipposideros%commersoni?% Barbara%Han,%JP%Schmidt,%Laura%Alexander,%% David%Hayman,%Sarah%Bowden,%John%Drake% Viruses 2014, 6 1763 Figure 1. (A) The multiple transmission pathways are shown for Ebolavirus genera viruses. The role of vectors is unlikely, but not known (dashed line). Those pathways with epidemiological uncertainty are shown with question marks. Potential reservoir dynamics are shown in blue, spillover epidemics in small mammals (Africa), pigs (Reston ebolavirus only), duikers (Africa), primates and humans shown in red and ongoing human transmission in orange; (B) The multiple transmission pathways are shown for Marburgvirus genera viruses. The role of vectors is unlikely, but not known (dashed line). Those with epidemiological uncertainty are shown with question marks. Potential reservoir dynamics are shown in blue, spillover epidemics in primates and humans shown in red and ongoing human transmission in orange. A) Ebolavirus transmission dynamics Spillover dynamics ? ? ? ? ? ? ? Intra- and inter- species ? ? ? transmission ??% ? ? ? Reservoir dynamics Olival&and&Hayman&2014& B) Marburgvirus transmission dynamics Spillover dynamics Intra- and inter- ? species ? ? transmission ? ? ? Reservoir dynamics ! Can%we%help%target%surveillance?%% ! What%are%additional%candidate%reservoir%species% for%filoviruses?% ! How%are%filovirus%reservoirs%distinct%from%nonG reservoirs?% % “Reservoir”&=&any&evidence&of&a&positive&filovirus&infection&using&any&diagnostic&test& Distribution*of*all*bat*species*found*‘positive’*for*filovirus*infection*(N=23/1116*bats)* -

Available Only Within the Gorilla Journal PDF File
Gorilla Journal Journal of Berggorilla & Regenwald Direkthilfe No. 32, June 2006 The Stories of Bwindi-Impenetra- The Cross-Sanaga Humans and Go- Mugaruka and ble: 15 Years as a Gorillas: North- rillas – what Kind Chimanuka National Park ernmost Gorilla of Relationship? Populations BERGGORILLA & REGENWALD DIREKTHILFE Authors of this Issue a scientifi c assistant at the Inst. of Bio- CONTENTS science at the University of Rostock. D. R. Congo 3 Stephen Asuma is a Field Offi cer Jean Claude Kyungu Kasolene Trip to Kahuzi-Biega 3 for IGCP in Uganda. led an ecology NGO, the Tayna Gorilla Attack on the Mugaba Patrol Post 3 James Byamukama has worked Reserve and the Walikale Community Le Gorille Magazine 2006 4 for IGCP as a Field Offi cer since April Gorilla Reserve and is now Project Ma- The Stories of Mugaruka and Chi- 2004. Since 1991 he has worked with nager for Tshiabirimu Gorilla Project. manuka ... so far 4 the Uganda Forest Department and Dr. Eric Leroy is a virologist and the The Silverback Mugaruka 5 with UNDP/GEF. chief of the “Emerging Viruses Unit” in New Patrol Post at Mt. Tshiabirimu 6 Prof. Dr. Raymond Corbey is a the Centre International de Recherch- Uganda 8 philosopher and anthropologist who is es Médicales de Franceville, Gabon. Bwindi-Impenetrable: 15 Years 8 connected to the Dept. of Philosophy of Dr. Alastair McNeilage is currently HuGo – the Uganda Experience 10 Tilburg University and the Dept. of Ar- the director of the Institute of Tropical Cross River 13 chaeology of Leiden University. Forest Conservation in Bwindi. He has Trip to Nigeria 13 Prof. -

A Historical Perspective and Review of the Evidence to Support Fruit Bats As the Natural Reservoir for Ebola Viruses
Georgia State University ScholarWorks @ Georgia State University Public Health Theses School of Public Health Fall 12-20-2012 A Historical Perspective and Review of the Evidence to Support Fruit Bats as the Natural Reservoir for Ebola Viruses Zachary Reed Follow this and additional works at: https://scholarworks.gsu.edu/iph_theses Recommended Citation Reed, Zachary, "A Historical Perspective and Review of the Evidence to Support Fruit Bats as the Natural Reservoir for Ebola Viruses." Thesis, Georgia State University, 2012. https://scholarworks.gsu.edu/iph_theses/241 This Thesis is brought to you for free and open access by the School of Public Health at ScholarWorks @ Georgia State University. It has been accepted for inclusion in Public Health Theses by an authorized administrator of ScholarWorks @ Georgia State University. For more information, please contact [email protected]. A Historical Perspective and Review of the Evidence to Support Fruit Bats as the Natural Reservoir for Ebola Viruses By Zachary D. Reed B.S. University of Georgia A Capstone Project Submitted to the Graduate Faculty of Georgia State University in Partial Fulfillment of the Requirement for the Degree MASTER OF PUBLIC HEALTH ATLANTA, GEORGIA 2012 1 Abstract The Ebola viruses cause sporadic outbreaks of Ebola hemorrhagic fever (EHF) where origins have been traced to the continent of Africa and the Philippines. Since the initial discovery of Zaire and Sudan ebolavirus in 1976, the Ebola viruses have been responsible for severe hemorrhagic fever outbreaks in Africa with case fatality rates between 40-90%. The natural reservoir(s) of the Ebola viruses is currently unknown, but there is mounting evidence that fruit bats may play a key role. -

List of Taxa for Which MIL Has Images
LIST OF 27 ORDERS, 163 FAMILIES, 887 GENERA, AND 2064 SPECIES IN MAMMAL IMAGES LIBRARY 31 JULY 2021 AFROSORICIDA (9 genera, 12 species) CHRYSOCHLORIDAE - golden moles 1. Amblysomus hottentotus - Hottentot Golden Mole 2. Chrysospalax villosus - Rough-haired Golden Mole 3. Eremitalpa granti - Grant’s Golden Mole TENRECIDAE - tenrecs 1. Echinops telfairi - Lesser Hedgehog Tenrec 2. Hemicentetes semispinosus - Lowland Streaked Tenrec 3. Microgale cf. longicaudata - Lesser Long-tailed Shrew Tenrec 4. Microgale cowani - Cowan’s Shrew Tenrec 5. Microgale mergulus - Web-footed Tenrec 6. Nesogale cf. talazaci - Talazac’s Shrew Tenrec 7. Nesogale dobsoni - Dobson’s Shrew Tenrec 8. Setifer setosus - Greater Hedgehog Tenrec 9. Tenrec ecaudatus - Tailless Tenrec ARTIODACTYLA (127 genera, 308 species) ANTILOCAPRIDAE - pronghorns Antilocapra americana - Pronghorn BALAENIDAE - bowheads and right whales 1. Balaena mysticetus – Bowhead Whale 2. Eubalaena australis - Southern Right Whale 3. Eubalaena glacialis – North Atlantic Right Whale 4. Eubalaena japonica - North Pacific Right Whale BALAENOPTERIDAE -rorqual whales 1. Balaenoptera acutorostrata – Common Minke Whale 2. Balaenoptera borealis - Sei Whale 3. Balaenoptera brydei – Bryde’s Whale 4. Balaenoptera musculus - Blue Whale 5. Balaenoptera physalus - Fin Whale 6. Balaenoptera ricei - Rice’s Whale 7. Eschrichtius robustus - Gray Whale 8. Megaptera novaeangliae - Humpback Whale BOVIDAE (54 genera) - cattle, sheep, goats, and antelopes 1. Addax nasomaculatus - Addax 2. Aepyceros melampus - Common Impala 3. Aepyceros petersi - Black-faced Impala 4. Alcelaphus caama - Red Hartebeest 5. Alcelaphus cokii - Kongoni (Coke’s Hartebeest) 6. Alcelaphus lelwel - Lelwel Hartebeest 7. Alcelaphus swaynei - Swayne’s Hartebeest 8. Ammelaphus australis - Southern Lesser Kudu 9. Ammelaphus imberbis - Northern Lesser Kudu 10. Ammodorcas clarkei - Dibatag 11. Ammotragus lervia - Aoudad (Barbary Sheep) 12. -

Overview of Bat and Wildlife Coronavirus Surveillance in Africa: a Framework for Global Investigations
viruses Review Overview of Bat and Wildlife Coronavirus Surveillance in Africa: A Framework for Global Investigations Marike Geldenhuys 1 , Marinda Mortlock 1 , Jonathan H. Epstein 1,2 , Janusz T. Paw˛eska 1,3 , Jacqueline Weyer 1,3,4 and Wanda Markotter 1,* 1 Centre for Viral Zoonoses, Department of Medical Virology, Faculty of Health Sciences, University of Pretoria, Pretoria 0001, South Africa; [email protected] (M.G.); [email protected] (M.M.); [email protected] (J.H.E.); [email protected] (J.T.P.); [email protected] (J.W.) 2 EcoHealth Alliance, New York, NY 10001, USA 3 Centre for Emerging Zoonotic and Parasitic Diseases, National Institute for Communicable Diseases, Johannesburg 2131, South Africa 4 Department of Microbiology and Infectious Diseases, School of Pathology, University of Witwatersrand, Johannesburg 2131, South Africa * Correspondence: [email protected] Abstract: The ongoing coronavirus disease 2019 (COVID-19) pandemic has had devastating health and socio-economic impacts. Human activities, especially at the wildlife interphase, are at the core of forces driving the emergence of new viral agents. Global surveillance activities have identified bats as the natural hosts of diverse coronaviruses, with other domestic and wildlife animal species possibly acting as intermediate or spillover hosts. The African continent is confronted by several factors that challenge prevention and response to novel disease emergences, such as high species diversity, inadequate health systems, and drastic social and ecosystem changes. We reviewed published animal coronavirus surveillance studies conducted in Africa, specifically summarizing surveillance approaches, species numbers tested, and findings. Far more surveillance has been Citation: Geldenhuys, M.; Mortlock, initiated among bat populations than other wildlife and domestic animals, with nearly 26,000 bat M.; Epstein, J.H.; Paw˛eska,J.T.; Weyer, J.; Markotter, W. -

Master's Thesis
MASTER’S THESIS ‘Megabats’ Stephen Turnbull Department of Biological Sciences Faculty of Science Aarhus University, Denmark [email protected] Supervisor: Associate Professor Jens M. Olesen Cover photograph: Dorte Nyhagen Introduction Why megabats? A brief explanation of my experiences with megabats. I first came across megabats when studying for my honours project at Aberdeen University under the supervision of Professor Paul Racey – an intimidating yet extremely likeable giant of the bat world. I was to study Pteropus rodricensis, the famed golden fruit bat, endemic to the island of Rodrigues; a tiny far-flung speck in the Indian Ocean, politically aligned with Mauritius. I had some idea of what to expect, but no firm plans of how to carry out my studies, relying instead on my confident ability to improvise. Upon arrival, the island presented itself as a catalogue of environmental short-sightedness and ecological collapse, yet the fruit bats clung on to their perilous existence, saved from extinction by the irregular topography of some parts of the island. In a near- vertical and densely vegetated gorge, the bats could roost in peace during the day, flying to their feeding sites each evening at dusk, their destinations presumably carefully planned the previous night. I quickly came to realise a number of problems inherently linked with the study of fruit-bats. Firstly, they’re nocturnal. This presents a whole host of difficulties, not least of which being the absence of daylight. Secondly, there was no way in which to access their roost site, and even if I could, my clumsy approach would disturb them.