Tradjenta (Linagliptin)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Supplementary Material
Supplementary material Table S1. Search strategy performed on the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL). 1. Randomi*ed study OR random allocation OR Randomi*ed controlled trial OR Random* Control* trial OR RCT Epidemiological study 2. sodium glucose cotransporter 2 OR sodium glucose cotransporter 2 inhibitor* OR sglt2 inhibitor* OR empagliflozin OR dapagliflozin OR canagliflozin OR ipragliflozin OR tofogliflozin OR ertugliflozin OR sotagliflozin OR sergliflozin OR remogliflozin 3. 1 AND 2 1 Table S2. Safety outcomes of empagliflozin and linagliptin combination therapy compared with empagliflozin or linagliptin monotherapy in treatment naïve type 2 diabetes patients Safety outcome Comparator 1 Comparator 2 I2 RR [95% CI] Number of events Number of events / / total subjects total subjects i. Empagliflozin + linagliptin vs empagliflozin monotherapy Empagliflozin + Empagliflozin linagliptin monotherapy ≥ 1 AE(s) 202/272 203/270 77% 0.99 [0.81, 1.21] ≥ 1 drug-related 37/272 38/270 0% 0.97 [0.64, 1.47] AE(s) ≥ 1 serious AE(s) 13/272 19/270 0% 0.68 [0.34, 1.35] Hypoglycaemia* 0/272 5/270 0% 0.18 [0.02, 1.56] UTI 32/272 25/270 29% 1.28 [0.70, 2.35] Events suggestive 12/272 13/270 9% 0.92 [0.40, 2.09] of genital infection i. Empagliflozin + linagliptin vs linagliptin monotherapy Empagliflozin + Linagliptin linagliptin monotherapy ≥ 1 AE(s) 202/272 97/135 0% 1.03 [0.91, 1.17] ≥ 1 drug-related 37/272 17/135 0% 1.08 [0.63, 1.84] AE(s) ≥ 1 serious AE(s) 13/272 2/135 0% 3.22 [0.74, 14.07] Hypoglycaemia* 0/272 1/135 NA 0.17 [0.01, 4.07] UTI 32/272 12/135 0% 1.32 [0.70, 2.49] Events suggestive 12/272 4/135 0% 1.45 [0.47, 4.47] of genital infection RR, relative risk; AE, adverse event; UTI, urinary tract infection. -

Assessment of the Pharmacokinetic Interaction Between the Novel DPP-4 Inhibitor Linagliptin Andasulfonylurea,Glyburide,Inhealthysubjects
Drug Metab. Pharmacokinet. 26 (2): 123129 (2011). Copyright © 2011 by the Japanese Society for the Study of Xenobiotics (JSSX) Regular Article Assessment of the Pharmacokinetic Interaction between the Novel DPP-4 Inhibitor Linagliptin andaSulfonylurea,Glyburide,inHealthySubjects Ulrike GRAEFE-MODY1,*, Peter ROSE2,ArneRING2,KerstinZANDER2, Mario IOVINO2 and Hans-Juergen WOERLE1 1Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany 2Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach, Germany Full text of this paper is available at http://www.jstage.jst.go.jp/browse/dmpk Summary: The aim of this study was to investigate the effect of the dipeptidyl peptidase-4 inhibitor linagliptin on the pharmacokinetics of glyburide (a CYP2C9 and CYP3A4 substrate) and vice versa.This randomized, open-label, three-period, two-way crossover study examined the effects of co-administration of multiple oral doses of linagliptin (5 mg/day © 6 days) and single doses of glyburide (1.75 mg/day © 1day)on the relative bioavailability of either compound in healthy subjects (n = 20, age 1855 years). Coadmin- istration of glyburide did not alter the steady-state pharmacokinetics of linagliptin. Geometric mean ratios (GMRs) [90% CI] for (linagliptin + glyburide)/linagliptin AUC¸,ss and Cmax,ss were 101.7% [97.7105.8%] and 100.8% [89.0114.3%], respectively. For glyburide, there was a slight reduction in exposure of ³14% when coadministered with linagliptin (GMRs [90% CI] for (glyburide + linagliptin)/glyburide AUC0¨ and Cmax were 85.7% [79.892.1%] and 86.2% [79.693.3%], respectively). However, this was not seen as clinically relevant due to the absence of a reliable doseresponse relationship and the known large pharmacokinetic interindividual variability of glyburide. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -
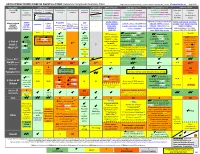
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances The
International Journal of Molecular Sciences Article The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances the Contractile Recovery of Mouse Hearts at a Concentration Equivalent to that Achieved with Standard Dosing in Humans 1, 1, 1 1 Sri Nagarjun Batchu y, Veera Ganesh Yerra y , Youan Liu , Suzanne L. Advani , Thomas Klein 2 and Andrew Advani 1,* 1 Keenan Research Center for Biomedical Science and Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON M5B 1T8, Canada; [email protected] (S.N.B.); [email protected] (V.G.Y.); [email protected] (Y.L.); [email protected] (S.L.A.) 2 Department of Cardiometabolic Diseases Research, Boehringer Ingelheim Pharma GmbH & Co. KG, 88397 Biberach, Germany; [email protected] * Correspondence: [email protected]; Tel.: +1-416-864-6060 (ext. 8413) These authors contributed equally to this work. y Received: 14 June 2020; Accepted: 9 August 2020; Published: 11 August 2020 Abstract: Despite a similar mechanism of action underlying their glucose-lowering effects in type 2 diabetes, dipeptidyl peptidase-4 (DPP-4) inhibitors have diverse molecular structures, raising the prospect of agent-specific, glucose-independent actions. To explore the issue of possible DPP-4 inhibitor cardiac heterogeneity, we perfused different DPP-4 inhibitors to beating mouse hearts ex vivo, at concentrations equivalent to peak plasma levels achieved in humans with standard dosing. We studied male and female mice, young non-diabetic mice, and aged diabetic high fat diet-fed mice and observed that linagliptin enhanced recovery after ischemia-reperfusion, whereas sitagliptin, alogliptin, and saxagliptin did not. -

Linagliptin (Tradjenta) for the Treatment of Diabetes Mellitus KAREN WHALEN, Pharmd, BCPS, CDE, and KAREN R
STEPS New Drug Reviews Linagliptin (Tradjenta) for the Treatment of Diabetes Mellitus KAREN WHALEN, PharmD, BCPS, CDE, and KAREN R. SANDO, PharmD, CDE University of Florida College of Pharmacy, Gainesville, Florida STEPS new drug reviews Linagliptin (Tradjenta) is a dipeptidyl-peptidase-4 (DPP-4) inhibitor labeled for the treat- cover Safety, Tolerability, ment of type 2 diabetes mellitus. Similar to sitagliptin (Januvia) and saxagliptin (Onglyza), Effectiveness, Price, and Simplicity. Each indepen- linagliptin delays the breakdown of endogenous incretin hormones such as glucagon-like dent review is provided peptide 1 and glucose-dependent insulinotropic polypeptide. These hormones, when secreted by authors who have no in response to food intake, stimulate postmeal insulin secretion, inhibit glucagon release, financial association with improve satiety, and slow gastric emptying.1,2 Linagliptin can be used alone or in combination the drug manufacturer. with metformin (Glucophage), sulfonylureas, pioglitazone (Actos), or insulin. The series coordinator for AFP is Allen F. Shaugh- nessy, PharmD, Tufts Drug Dosage Dose form Cost* University Family Medicine Residency Program at Linagliptin (Tradjenta) 5 mg daily 5-mg tablet $254 for 30 tablets Cambridge Health Alli- ance, Malden, Mass. *—Estimated retail price of one month’s treatment based on information obtained at http://www.goodrx.com A collection of STEPS pub- (accessed October 1, 2012). lished in AFP is available at http://www.aafp.org/ afp/steps. SAFETY control should be used in patients receiving Few severe adverse effects have been associ- strong inducers of cytochrome P450 3A4 ated with linagliptin. When used alone or or P-glycoprotein, such as rifampin. Lina- with metformin or pioglitazone, linagliptin gliptin is a U.S. -

Diabetes: Putting It All Together to Design a High Value Diabetes Regimen for Your Patient
Diabetes: Putting it all together to design a high value diabetes regimen for your patient Cecilia C. Low Wang, MD Professor of Medicine Division of Endocrinology, Metabolism and Diabetes University of Colorado School of Medicine [email protected] Disclosures • None Objectives • Describe the benefits, side effects/risks, and costs of the newer diabetes medications • Discuss the value of the newer diabetes medications • Make high-value patient-centered decisions when intensifying diabetes therapy Worsening HbA1c • Ms L is a 48 year old woman here for routine f/u • She has Type 2 diabetes (x 5 years; no complications), obesity (BMI 41), chronic knee pain from osteoarthritis, and is postmenopausal s/p TAH 6 yr ago for uterine leiomyomas • You last saw her 6 months ago. At that time, her A1c was 6.4% on metformin 1000 mg BID • You see that her A1c is now 8.5%. • What other information do you need? • How would you intensify her diabetes treatment? “New-onset” diabetes • Mr. B is a 53 year old M hospitalized for NSTEMI and underwent 3v CABG • He had HTN but no other medical history and was on no medications prior to admission • Admission point-of-care (POC) glucose: 263 mg/dL • HbA1c: 11.5% • He agrees that he needs to be on insulin upon discharge • Are there any non-insulin medications that should be considered for him? • How would you design his regimen? ADVANCE: Diabetes complications and A1c relationship CVA CV death • Linear relationship (no threshold) for eye complications • J-curve: Increasing DKD Retinopathy risk with A1c <6.5% for CV and renal complications 6 Zoungas, et al. -

Information for the User Trajenta® 5 Mg Film-Coated Tablets Linagliptin
Package leaflet: Information for the user Trajenta® 5 mg film-coated tablets Linagliptin Read all of this leaflet carefully before you start taking this medicine because it contains important information for you. - Keep this leaflet. You may need to read it again. - If you have any further questions, ask your doctor, pharmacist or nurse. - This medicine has been prescribed for you only. Do not pass it on to others. It may harm them, even if their signs of illness are the same as yours. - If you get any side effects talk to your doctor, pharmacist or nurse. This includes any possible side effects not listed in this leaflet. See section 4. What is in this leaflet: 1. What Trajenta is and what it is used for 2. What you need to know before you take Trajenta 3. How to take Trajenta 4. Possible side effects 5. How to store Trajenta 6. Contents of the pack and other information 1. What Trajenta is and what it is used for Trajenta contains the active substance linagliptin which belongs to a group of medicines called “oral anti-diabetics”. Oral anti-diabetics are used to treat high blood sugar levels. They work by helping the body reduce the level of sugar in your blood. Trajenta is used for ‘type 2 diabetes’ in adults, if the disease cannot be adequately controlled with one oral anti-diabetic medicine (metformin or sulphonylureas) or diet and exercise alone. Trajenta may be used together with other anti-diabetic medicines e.g. metformin, sulphonylureas (e.g. glimepiride, glipizide), empagliflozin, or insulin. -

Trajenta, INN-Linagliptin
ANNEX I SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Trajenta 5 mg film-coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Each tablet contains 5 mg of linagliptin. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet (tablet). 8 mm diameter round, light red film-coated tablet debossed with "D5" on one side and the Boehringer Ingelheim logo on the other. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Trajenta is indicated in adults with type 2 diabetes mellitus as an adjunct to diet and exercise to improve glycaemic control as: monotherapy • when metformin is inappropriate due to intolerance, or contraindicated due to renal impairment. combination therapy • in combination with other medicinal products for the treatment of diabetes, including insulin, when these do not provide adequate glycaemic control (see sections 4.4, 4.5 and 5.1 for available data on different combinations). 4.2 Posology and method of administration Posology The dose of linagliptin is 5 mg once daily. When linagliptin is added to metformin, the dose of metformin should be maintained, and linagliptin administered concomitantly. When linagliptin is used in combination with a sulphonylurea or with insulin, a lower dose of the sulphonylurea or insulin, may be considered to reduce the risk of hypoglycaemia (see section 4.4) Special populations Renal impairment For patients with renal impairment, no dose adjustment for linagliptin is required. Hepatic impairment Pharmacokinetic studies suggest that no dose adjustment is required for patients with hepatic impairment but clinical experience in such patients is lacking. Elderly No dose adjustment is necessary based on age. -

Janumet XR (Sitagliptin/Metformin), Jentadueto
Januvia® (sitagliptin), Janumet®, Janumet XR (sitagliptin/metformin), Jentadueto®, Jentadueto XR (linagliptin/metformin), Tradjenta® (linagliptin), Glyxambi® (linagliptin/empagliflozin) – New warning • On August 10, 2017, the FDA approved updates to the Warnings and Precautions sections of the Januvia (sitagliptin), Janumet (sitagliptin/metformin), Janumet XR (sitagliptin/metformin XR), Jentadueto (linagliptin/metformin), Jentadueto XR (linagliptin/metformin XR), Tradjenta (linagliptin), and Glyxambi (linagliptin/empagliflozin) drug labels regarding heart failure. • Januvia, Janumet, Janumet XR, Jentadueto, Jentadueto XR, Tradjenta, and Glyxambi are approved as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). — Combination products are indicated when treatment with both agents is appropriate. — These products should not be used in patients with type 1 diabetes or for the treatment of diabetic ketoacidosis. — These products have not been studied in patients with a history of pancreatitis. — Jardiance® (empagliflozin) is indicated to reduce the risk of cardiovascular (CV) death in adults with T2DM and established CV disease. However, the effectiveness of Glyxambi on reducing the risk of CV death in adults with T2DM and CV disease has not been established. • An association between dipeptidyl peptidase-4 (DPP-4) inhibitor treatment and heart failure has been observed in CV outcomes trials for two other members (Nesina® [alogliptin] and Onglyza® [saxagliptin]) of the DPP-4 inhibitor class. These trials evaluated patients with T2DM and atherosclerotic CV disease. • The risks and benefits of Januvia, Janumet, Janumet XR, Jentadueto, Jentadueto XR, Tradjenta, and Glyxambi should be considered prior to initiating treatment in patients at risk for heart failure, such as those with a prior history of heart failure and a history of renal impairment, and observe these patients for signs and symptoms of heart failure during therapy. -

Growing Our Future in Diabetes Care: Where Are We Now and Where Are We Going?
GROWING OUR FUTURE IN DIABETES CARE: WHERE ARE WE NOW AND WHERE ARE WE GOING? Ashley Firm, Pharm.D. Lindsey Meston, Pharm.D. Disclosure Neither Dr. Firm nor Dr. Meston have anything to disclosure concerning possible financial or personal relationships with commercial entities (or their competitors) mentioned in this presentation. Objectives ■ Summarize key differences and updates to guidelines related to the care of diabetic patients, especially updates in the 2018 American Diabetes Association Standard of Medical Care in Diabetes ■ Select most appropriate treatment regimens for sample patients based on diabetic presentation and co-morbid conditions ■ Evaluate new products to the market for the treatment of diabetes, including place in therapy, pros and cons of use, major adverse effects, and other pertinent pharmacokinetic and pharmacodynamic properties. SOC-36238233 Socrative Join Code Which of the following correctly pairs a basal insulin and GLP1-RA coformulation? A. Insulin glargine- semaglutide B. Insulin determir- dulaglutide C. Insulin degludec- liraglutide Which new agent was accepted by the FDA for regulatory filing as a dual inhibitor of SGLT-2 in the treatment of type 1 diabetes? A. Sotagliflozin B. Empagliflozin C. Dapagliflozin D. Canagliflozin Under the ADA Standards of Care 2018, a patient with a history of a myocardial infarction would be recommended for which class of medication in addition to metformin? A. Thiazolidinediones B. Sulfonylureas C. Sodium Glucose Co-Transporter 2 Inhibitor D. Alpha Glucosidase Inhibitor Under the updated guidelines of the American Association of Clinical Endocrinologists, a patient failing to achieve A1C goal with metformin would be most appropriately treated with a medication from which class? A. -

Type I Diabetes Treatments Clinical Notes Recommendations
Ramsell's Recommendation: NV ADAP should cover Diabetic Supplies such as Lancets, test strips, needles ONLY. Diabetic Meters in most cases are obtained free of charge to patients or thru patient assistance programs. Recommendations (Use DM TXT guidelines and for efficient treatment recommendations. X Consider effiacacy, safety, and cost combined with a patient-centered approach when choosing Type I Diabetes Treatments Clinical notes formulary/TXT agents. NV Medicaid Questions? For Type 1 and some cases of Type 2 DM, ADD ALL Insulins INSULINS Vials & Pens Short Acting Insulins regular insulin (Humulin and Novolin) √ Rapid Acting Insulins insulin aspart(NovoLog, FlexPen) √ insulin glulisine (Apidra) √ insulin lispro (Humalog) √ Intermediate Acting Insulins insulin isophane (Humulin N, Novolin N) √ Long Acting Insulins insulin degludec (Tresiba) √ insulin detemir (Levemir) √ insulin glargine (Lantus) √ insulin glargine (Toujeo) Combination Insulins NovoLog Mix 70/30 (insulin aspart protamine-insulin aspart) Humalog Mix 75/25 (insulin lispro protamine-insulin lispro) Humalog Mix 50/50 (insulin lispro protamine-insulin lispro) Humulin 70/30 (human insulin NPH-human insulin regular) Novolin 70/30 (human insulin NPH-human insulin regular) Ryzodeg (insulin degludec-insulin aspart) Amylinomimetic Drug Pramlintide (SymlinPen 120, SymlinPen 60) √ Consider efficacy, safety, and cost combined with a patient- centered approach when Type 2 Diabetes Treatments choosing agents. These drugs slow the digestion of starches and sugars and are used for mild Alpha-glucosidase inhibitor cases of diabetes acarbose (Precose) √ miglitol (Glyset) √ Metformin is the preferred first-line agent providing a 1-2% decrease in A1c. • Metformin is not associated with weight gain, has a low risk for hypoglycemia, and is the most cost effective agent.