Empagliflozin, Linagliptin, and Metformin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Diabetes Mellitus
TREATMENT OF DIABETES MELLITUS DIABETES is a condition that affects how the body makes energy from food. Food is broken down into sugar (glucose) in the body and released into the blood. When the blood sugar level rises after a meal, insulin responds to let the sugar into the cells to be used as energy. In diabetes, the body either does not make enough insulin or it stops responding to insulin as well as it should. This results in sugar staying in the blood and leads to serious health problems over time. DIAGNOSIS OF DIABETES1 • A1C Test: Lab test measuring average blood sugar over past two to three months • Fasting Blood Sugar Test: Lab test measuring blood sugar after eight hours of no food or drink • Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and two hours after drinking a specific sugary liquid • Random Blood Sugar Test: Measures blood sugar at a moment in time, without any kind of preparation (like fasting) FASTING BLOOD ORAL GLUCOSE TOLERANCE RANDOM BLOOD RESULT A1C TEST SUGAR TEST TEST SUGAR TEST Diabetes ≥ 6.5% ≥126 mg/dL ≥ 200 mg/dL ≥ 200 mg/dL Prediabetes 5.7 – 6.4% 100 – 125 mg/dL 140 – 199 mg/dL N/A Normal < 5.7% ≤99 mg/dL < 140 mg/dL N/A NON-DRUG TREATMENTS2 THERAPY COST WHAT TO EXPECT Diet (Mediterranean diet) and exercise (30 minutes a day, five days a week of moderate- Weight loss $-$$ intensity exercise); 7% weight loss decreases risk of diabetes3 Psychological intervention $$-$$$ Psychotherapy may reduce diabetic distress and improve glycemic control4,5 nationalcooperativerx.com PRESCRIPTION TREATMENTS -

Supplementary Material
Supplementary material Table S1. Search strategy performed on the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL). 1. Randomi*ed study OR random allocation OR Randomi*ed controlled trial OR Random* Control* trial OR RCT Epidemiological study 2. sodium glucose cotransporter 2 OR sodium glucose cotransporter 2 inhibitor* OR sglt2 inhibitor* OR empagliflozin OR dapagliflozin OR canagliflozin OR ipragliflozin OR tofogliflozin OR ertugliflozin OR sotagliflozin OR sergliflozin OR remogliflozin 3. 1 AND 2 1 Table S2. Safety outcomes of empagliflozin and linagliptin combination therapy compared with empagliflozin or linagliptin monotherapy in treatment naïve type 2 diabetes patients Safety outcome Comparator 1 Comparator 2 I2 RR [95% CI] Number of events Number of events / / total subjects total subjects i. Empagliflozin + linagliptin vs empagliflozin monotherapy Empagliflozin + Empagliflozin linagliptin monotherapy ≥ 1 AE(s) 202/272 203/270 77% 0.99 [0.81, 1.21] ≥ 1 drug-related 37/272 38/270 0% 0.97 [0.64, 1.47] AE(s) ≥ 1 serious AE(s) 13/272 19/270 0% 0.68 [0.34, 1.35] Hypoglycaemia* 0/272 5/270 0% 0.18 [0.02, 1.56] UTI 32/272 25/270 29% 1.28 [0.70, 2.35] Events suggestive 12/272 13/270 9% 0.92 [0.40, 2.09] of genital infection i. Empagliflozin + linagliptin vs linagliptin monotherapy Empagliflozin + Linagliptin linagliptin monotherapy ≥ 1 AE(s) 202/272 97/135 0% 1.03 [0.91, 1.17] ≥ 1 drug-related 37/272 17/135 0% 1.08 [0.63, 1.84] AE(s) ≥ 1 serious AE(s) 13/272 2/135 0% 3.22 [0.74, 14.07] Hypoglycaemia* 0/272 1/135 NA 0.17 [0.01, 4.07] UTI 32/272 12/135 0% 1.32 [0.70, 2.49] Events suggestive 12/272 4/135 0% 1.45 [0.47, 4.47] of genital infection RR, relative risk; AE, adverse event; UTI, urinary tract infection. -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

The Sodium Glucose Cotransporter Type 2 Inhibitor Empagliflozin Preserves B-Cell Mass and Restores Glucose Homeostasis in the Male Zucker Diabetic Fatty Rat
1521-0103/350/3/657–664$25.00 http://dx.doi.org/10.1124/jpet.114.213454 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 350:657–664, September 2014 Copyright ª 2014 by The American Society for Pharmacology and Experimental Therapeutics The Sodium Glucose Cotransporter Type 2 Inhibitor Empagliflozin Preserves b-Cell Mass and Restores Glucose Homeostasis in the Male Zucker Diabetic Fatty Rat Henrik H. Hansen, Jacob Jelsing, Carl Frederik Hansen, Gitte Hansen, Niels Vrang, Michael Mark, Thomas Klein, and Eric Mayoux Gubra, Hørsholm, Denmark (H.H.H., J.J., C.F.H., G.H., N.V.); and Boehringer Ingelheim Pharma, Biberach, Germany (M.M., T.K., E.M.) Received January 22, 2014; accepted July 2, 2014 Downloaded from ABSTRACT Type 2 diabetes is characterized by impaired b-cell function at week 8 of treatment compared with week 4, those of empagliflozin associated with progressive reduction of insulin secretion and remained stable throughout the study period. Similarly, empagliflozin b -cell mass. Evidently, there is an unmet need for treatments improved glucose tolerance and preserved insulin secretion jpet.aspetjournals.org with greater sustainability in b-cell protection and antidiabetic after both 4 and 8 weeks of treatment. These effects were efficacy. Through an insulin and b cell–independent mechanism, reflected by less reduction in b-cell mass with empagliflozin or empagliflozin, a specific sodium glucose cotransporter type 2 liraglutide at week 4, whereas only empagliflozin showed b-cell (SGLT-2) inhibitor, may potentially provide longer efficacy. This sparing effects also at week 8. Although this study cannot be study compared the antidiabetic durability of empagliflozin treat- used to dissociate the absolute antidiabetic efficacy among ment (10 mg/kg p.o.) against glibenclamide (3 mg/kg p.o.) and the different mechanisms of drug action, the study demon- liraglutide (0.2 mg/kg s.c.) on deficient glucose homeostasis and strates that empagliflozin exerts a more sustained improve- b-cell function in Zucker diabetic fatty (ZDF) rats. -

PRESCRIBING INFORMATION ------WARNINGS and PRECAUTIONS------These Highlights Do Not Include All the Information Needed to Use JARDIANCE Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use JARDIANCE safely and effectively. See full prescribing information for Ketoacidosis: Assess patients who present with signs and symptoms of JARDIANCE. metabolic acidosis for ketoacidosis, regardless of blood glucose level. If suspected, discontinue JARDIANCE, evaluate and treat promptly. JARDIANCE® (empagliflozin tablets), for oral use Before initiating JARDIANCE, consider risk factors for ketoacidosis. Initial U.S. Approval: 2014 Patients on JARDIANCE may require monitoring and temporary discontinuation of therapy in clinical situations known to predispose to ---------------------------RECENT MAJOR CHANGES--------------------------- ketoacidosis. (5.1) Volume Depletion: Before initiating JARDIANCE, assess volume status Indications and Usage (1) 8/2021 and renal function in patients with impaired renal function, elderly Dosage and Administration (2.1) 6/2021 patients, or patients on loop diuretics. Monitor for signs and symptoms Dosage and Administration (2.2) 8/2021 during therapy. (5.2, 6.1) Dosage and Administration (2.3) – Removed 8/2021 Urosepsis and Pyelonephritis: Evaluate patients for signs and symptoms Contraindications (4) 6/2021 of urinary tract infections and treat promptly, if indicated (5.3) Warnings and Precautions (5.1, 5.2) 6/2021 Hypoglycemia: Consider lowering the dose of insulin secretagogue or Warnings and Precautions (5.3, 5.5) 8/2021 insulin to reduce the risk of hypoglycemia when initiating JARDIANCE Warnings and Precautions (5.9) – Removed 6/2021 (5.4) ----------------------------INDICATIONS AND USAGE--------------------------- Necrotizing Fasciitis of the Perineum (Fournier’s Gangrene): Serious, JARDIANCE is a sodium-glucose co-transporter 2 (SGLT2) inhibitor life-threatening cases have occurred in both females and males. -

Clinical Pharmacology Biopharmaceutics Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 206111Orig1s000 CLINICAL PHARMACOLOGY AND BIOPHARMACEUTICS REVIEW(S) (b) Q=(4) % at 20 minutes for empagliflozin and metformin HCl Review: The Biopharmaceutics review is focused on the evaluation and acceptability of the bioequivalence and dissolution data to support approvability of the proposed FDC tablets. RECOMMENDATION: The bioequivalence results and dissolution method are acceptable. From the Biopharmaceutics perspective, NDA 206111 for Empagliflozin/Metformin Hydrochloride Fixed Dose Combination Tablets is recommended for approval. Signature Signature Digitally signed by Kelly M. Kitchens -S Digitally signed by Tapash K. Ghosh -S DN: c=US, o=U.S. Government, DN: c=US, o=U.S. Government, ou=HHS, Kelly M. Tapash K. ou=FDA, ou=People, ou=HHS, ou=FDA, ou=People, 0.9.2342.19200300.100.1.1=200033657 0.9.2342.19200300.100.1.1=1300148262 , cn=Tapash K. Ghosh -S 4, cn=Kelly M. Kitchens -S Date: 2015.04.15 16:19:26 -04'00' Kitchens -S Date: 2015.04.15 15:55:42 -04'00' Ghosh -S Kelly M. Kitchens, Ph.D. Tapash Ghosh, Ph.D. Acting Biopharmaceutics Lead Acting Biopharmaceutics Branch Chief Office of New Drug Products Office of New Drug Products cc. PSeo. 4 Bioequivalence Study No. 1276.6 8 9 Bioanalytical Results: Analyte Name: Empagliflozin Parameter Standard Curve Samples Concentration (nmol/mL) 1.11 2.22 111 55.4 222 665 998 1110 Inter day Precision 7.5 5.2 2.8 2.3 2.2 2.2 2.6 1.7 (%CV) Inter day Accuracy -0.8 0.6 1.0 0.3 -1.7 0.4 -0.2 0.1 (%bias) Linearity 0.994576 – 0.999437 (range -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option. -

Assessment of the Pharmacokinetic Interaction Between the Novel DPP-4 Inhibitor Linagliptin Andasulfonylurea,Glyburide,Inhealthysubjects
Drug Metab. Pharmacokinet. 26 (2): 123129 (2011). Copyright © 2011 by the Japanese Society for the Study of Xenobiotics (JSSX) Regular Article Assessment of the Pharmacokinetic Interaction between the Novel DPP-4 Inhibitor Linagliptin andaSulfonylurea,Glyburide,inHealthySubjects Ulrike GRAEFE-MODY1,*, Peter ROSE2,ArneRING2,KerstinZANDER2, Mario IOVINO2 and Hans-Juergen WOERLE1 1Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany 2Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach, Germany Full text of this paper is available at http://www.jstage.jst.go.jp/browse/dmpk Summary: The aim of this study was to investigate the effect of the dipeptidyl peptidase-4 inhibitor linagliptin on the pharmacokinetics of glyburide (a CYP2C9 and CYP3A4 substrate) and vice versa.This randomized, open-label, three-period, two-way crossover study examined the effects of co-administration of multiple oral doses of linagliptin (5 mg/day © 6 days) and single doses of glyburide (1.75 mg/day © 1day)on the relative bioavailability of either compound in healthy subjects (n = 20, age 1855 years). Coadmin- istration of glyburide did not alter the steady-state pharmacokinetics of linagliptin. Geometric mean ratios (GMRs) [90% CI] for (linagliptin + glyburide)/linagliptin AUC¸,ss and Cmax,ss were 101.7% [97.7105.8%] and 100.8% [89.0114.3%], respectively. For glyburide, there was a slight reduction in exposure of ³14% when coadministered with linagliptin (GMRs [90% CI] for (glyburide + linagliptin)/glyburide AUC0¨ and Cmax were 85.7% [79.892.1%] and 86.2% [79.693.3%], respectively). However, this was not seen as clinically relevant due to the absence of a reliable doseresponse relationship and the known large pharmacokinetic interindividual variability of glyburide. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -

204629Orig1s000
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 204629Orig1s000 RISK ASSESSMENT and RISK MITIGATION REVIEW(S) Department of Health and Human Services Public Health Service Food and Drug Administration Center for Drug Evaluation and Research Office of Surveillance and Epidemiology Office of Medication Error Prevention and Risk Management Risk Evaluation and Mitigation Strategy (REMS) Review Date: July 28, 2014 Reviewer(s): Amarilys Vega, M.D., M.P.H, Medical Officer Division of Risk Management (DRISK) Team Leader: Doris Auth, Pharm.D, Team Leader DRISK Division Director Cynthia LaCivita, Pharm.D, Acting Director DRISK Subject: Evaluation of need for a REMS Drug Name(s): Empagliflozin (Jardiance®) Therapeutic Class: Sodium-dependent glucose co-transporter-2 (SGLT2) inhibitor Dosage and Route: 10 mg, 25 mg tablet once daily/oral Application Type/Number: NDA 204629 Submission Number: Resubmission, June 3, 2014 (0032) Applicant/sponsor: Boehringer Ingelheim Pharmaceuticals, Inc. OSE RCM #: 2013-619 and 2013-656 *** This document contains proprietary and confidential information *** that should not be released to the public Reference ID: 3600276 1 INTRODUCTION This review documents the Division of Risk Management’s (DRISK) evaluation of whether a Risk Evaluation and Mitigation Strategy (REMS) is necessary for empagliflozin (NDA 204629). Boehringer Ingelheim Pharmaceuticals, Inc. is seeking approval for empagliflozin as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus (T2DM). DRISK reviewed the original application for empagliflozin submitted to FDA on March 5, 2013 and determined that a REMS was not required to manage the serious risks associated to empagliflozin (e.g., hypoglycemia, volume depletion, and genital infections). -
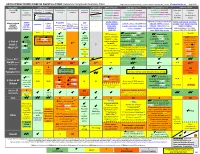
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances The
International Journal of Molecular Sciences Article The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances the Contractile Recovery of Mouse Hearts at a Concentration Equivalent to that Achieved with Standard Dosing in Humans 1, 1, 1 1 Sri Nagarjun Batchu y, Veera Ganesh Yerra y , Youan Liu , Suzanne L. Advani , Thomas Klein 2 and Andrew Advani 1,* 1 Keenan Research Center for Biomedical Science and Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON M5B 1T8, Canada; [email protected] (S.N.B.); [email protected] (V.G.Y.); [email protected] (Y.L.); [email protected] (S.L.A.) 2 Department of Cardiometabolic Diseases Research, Boehringer Ingelheim Pharma GmbH & Co. KG, 88397 Biberach, Germany; [email protected] * Correspondence: [email protected]; Tel.: +1-416-864-6060 (ext. 8413) These authors contributed equally to this work. y Received: 14 June 2020; Accepted: 9 August 2020; Published: 11 August 2020 Abstract: Despite a similar mechanism of action underlying their glucose-lowering effects in type 2 diabetes, dipeptidyl peptidase-4 (DPP-4) inhibitors have diverse molecular structures, raising the prospect of agent-specific, glucose-independent actions. To explore the issue of possible DPP-4 inhibitor cardiac heterogeneity, we perfused different DPP-4 inhibitors to beating mouse hearts ex vivo, at concentrations equivalent to peak plasma levels achieved in humans with standard dosing. We studied male and female mice, young non-diabetic mice, and aged diabetic high fat diet-fed mice and observed that linagliptin enhanced recovery after ischemia-reperfusion, whereas sitagliptin, alogliptin, and saxagliptin did not.