Management of Type 2 Diabetes Mellitus Dr Naomi Achong Endocrinologist MBBS(Hons) Bsc FRACP Phd Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Semaglutide Versus Liraglutide for Treatment of Obesity
Archives of Diabetes & Obesity DOI: 10.32474/ADO.2021.03.000162 ISSN: 2638-5910 Review Article Semaglutide versus liraglutide for treatment of obesity Nasser Mikhail* *Department of Medicine, Endocrinology Division, David-Geffen UCLA Medical School, USA *Corresponding author: Nasser Mikhail, Endocrinology Division, Department of Medicine, Olive View-UCLA Medical Center, David- Geffen UCLA Medical School, CA, USA Received: April 02, 2021 Published: April 19, 2021 Abstract Background: Once weekly (OW) semaglutide is a glucagon-like peptide-1 receptor agonist (GLP-1 RA) currently under evaluation for treatment of obesity at a dose of 2.4 mg OW. Objective Methods : To compare weight-loss efficacy and safety of once daily (OD) liraglutide 3.0 mg versus OW semaglutide 2.4 mg. : Pubmed research up to March 31, 2021. Randomized trials, pertinent animal studies, and reviews are included. Search Results terms were glucagon-like peptide-1 receptor agonists, weight loss, obesity, liraglutide, semaglutide, efficacy, safety. semaglutide 2.4 mg. However, marked resemblance between trials in terms of study protocols and subjects’ characteristics may allow indirect: No comparison. head to head In clinical trials are trials available of OW tosemaglutide, provide direct this comparison drug was consistently of efficacy ofassociated OD liraglutide with greater 3.0 mg weightversus lossOW than in trials of OD liraglutide. Thus, placebo-corrected percentage weight reduction was -10.3 to -12.4% and -5.4% with OW semaglutide and OD liraglutide, respectively. In patients with type 2 diabetes, corresponding weight reduction was less pronounced with both drugs being -6.2% and -4.3% with OW semaglutide and OD liraglutide, respectively. -

GLP-1 Receptor Agonists
Cognitive Vitality Reports® are reports written by neuroscientists at the Alzheimer’s Drug Discovery Foundation (ADDF). These scientific reports include analysis of drugs, drugs-in- development, drug targets, supplements, nutraceuticals, food/drink, non-pharmacologic interventions, and risk factors. Neuroscientists evaluate the potential benefit (or harm) for brain health, as well as for age-related health concerns that can affect brain health (e.g., cardiovascular diseases, cancers, diabetes/metabolic syndrome). In addition, these reports include evaluation of safety data, from clinical trials if available, and from preclinical models. GLP-1 Receptor Agonists Evidence Summary GLP-1 agonists are beneficial for patients with type 2 diabetes and obesity. Some evidence suggests benefits for Alzheimer’s disease. It is unclear whether it is beneficial for individuals without underlying metabolic disease. Semaglutide seems to be most effective for metabolic dysfunction, though liraglutide has more preclinical data for Alzheimer’s disease. Neuroprotective Benefit: Evidence from many preclinical studies and a pilot biomarker study suggest some neuroprotective benefits with GLP-1 agonists. However, whether they may be beneficial for everyone or only a subset of individuals (e.g. diabetics) is unclear. Aging and related health concerns: GLP-1 agonists are beneficial for treating diabetes and cardiovascular complications relating to diabetes. It is not clear whether they have beneficial effects in otherwise healthy individuals. Safety: GLP-1 agonists are generally safe for most people with minor side effects. However, long-term side effects are not known. 1 Availability: Available Dose: Varies - see Chemical formula: C172H265N43O51 (Liraglutide) as a prescription chart at the end of MW: 3751.262 g/mol medicine. -

Treatment of Diabetes Mellitus
TREATMENT OF DIABETES MELLITUS DIABETES is a condition that affects how the body makes energy from food. Food is broken down into sugar (glucose) in the body and released into the blood. When the blood sugar level rises after a meal, insulin responds to let the sugar into the cells to be used as energy. In diabetes, the body either does not make enough insulin or it stops responding to insulin as well as it should. This results in sugar staying in the blood and leads to serious health problems over time. DIAGNOSIS OF DIABETES1 • A1C Test: Lab test measuring average blood sugar over past two to three months • Fasting Blood Sugar Test: Lab test measuring blood sugar after eight hours of no food or drink • Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and two hours after drinking a specific sugary liquid • Random Blood Sugar Test: Measures blood sugar at a moment in time, without any kind of preparation (like fasting) FASTING BLOOD ORAL GLUCOSE TOLERANCE RANDOM BLOOD RESULT A1C TEST SUGAR TEST TEST SUGAR TEST Diabetes ≥ 6.5% ≥126 mg/dL ≥ 200 mg/dL ≥ 200 mg/dL Prediabetes 5.7 – 6.4% 100 – 125 mg/dL 140 – 199 mg/dL N/A Normal < 5.7% ≤99 mg/dL < 140 mg/dL N/A NON-DRUG TREATMENTS2 THERAPY COST WHAT TO EXPECT Diet (Mediterranean diet) and exercise (30 minutes a day, five days a week of moderate- Weight loss $-$$ intensity exercise); 7% weight loss decreases risk of diabetes3 Psychological intervention $$-$$$ Psychotherapy may reduce diabetic distress and improve glycemic control4,5 nationalcooperativerx.com PRESCRIPTION TREATMENTS -

A 26-Week Randomized Controlled Trial of Semaglutide Once Daily Versus Liraglutide and Placebo in Patients with Type 2 Diabetes
1926 Diabetes Care Volume 41, September 2018 Ildiko Lingvay,1 Cyrus V. Desouza,2 A 26-Week Randomized Katarina S. Lalic,3 Ludger Rose,4 Thomas Hansen,5 Jeppe Zacho,5 and Controlled Trial of Semaglutide Thomas R. Pieber6 EMERGING THERAPIES: DRUGS AND REGIMENS Once Daily Versus Liraglutide and Placebo in Patients With Type 2 Diabetes Suboptimally Controlled on Diet and Exercise With or Without Metformin Diabetes Care 2018;41:1926–1937 | https://doi.org/10.2337/dc17-2381 OBJECTIVE To investigate the efficacy and safety of once-daily semaglutide in comparison with once-daily liraglutide and placebo in patients with type 2 diabetes. RESEARCH DESIGN AND METHODS This 26-week, multicenter, double-blind trial involved patients diagnosed with 1University of Texas Southwestern Medical Cen- type 2 diabetes with HbA1c 7.0–10.0% (53–86 mmol/mol) and treated with diet ter at Dallas, Dallas, TX and exercise with or without metformin. Patients were randomized 2:2:1 to once- 2University of Nebraska Medical Center, Omaha, daily semaglutide, liraglutide, or placebo in one of four volume-matched doses NE 3Faculty of Medicine, University of Belgrade, and (semaglutide 0.05, 0.1, 0.2, or 0.3 mg and liraglutide 0.3, 0.6, 1.2, or 1.8 mg, with Clinic for Endocrinology, Diabetes and Metabolic both compared within each volume-matched dose group). Primary end point was Diseases, Clinical Center of Serbia, Belgrade, Serbia change in HbA1c from baseline to week 26. 4Institute for Diabetes Research in Munster,¨ RESULTS Munster,¨ Germany 5Novo Nordisk A/S, Søborg, Denmark In total, 705 randomized patients were exposed to trial products. -

OZEMPIC (Semaglutide) Injection, for Subcutaneous Use Initial U.S
HIGHLIGHTS OF PRESCRIBING INFORMATION ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙CONTRAINDICATIONS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ These highlights do not include all the information needed to use Personal or family history of medullary thyroid carcinoma or in patients OZEMPIC® safely and effectively. See full prescribing information with Multiple Endocrine Neoplasia syndrome type 2 (4). for OZEMPIC. Known hypersensitivity to OZEMPIC or any of the product components (4). OZEMPIC (semaglutide) injection, for subcutaneous use Initial U.S. Approval: 2017 ∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙WARNINGS AND PRECAUTIONS∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙∙ Pancreatitis: Has been reported in clinical trials. Discontinue promptly if WARNING: RISK OF THYROID C-CELL TUMORS pancreatitis is suspected. Do not restart if pancreatitis is confirmed (5.2). See full prescribing information for complete boxed warning. Diabetic Retinopathy Complications: Has been reported in a clinical trial. Patients with a history of diabetic retinopathy should be monitored (5.3). In rodents, semaglutide causes thyroid C-cell tumors. It is Never share an OZEMPIC pen between patients, even if the needle is unknown whether OZEMPIC causes thyroid C-cell tumors, changed (5.4). including medullary thyroid carcinoma (MTC), in humans as Hypoglycemia: When OZEMPIC is used with an insulin secretagogue or the human relevance of semaglutide-induced rodent thyroid C- insulin, consider lowering the dose of the secretagogue or insulin to reduce cell tumors has not been determined (5.1, 13.1). the risk of hypoglycemia (5.5). OZEMPIC is contraindicated in patients with a personal or Acute Kidney Injury: Monitor renal function in patients with renal family history of MTC or in patients with Multiple Endocrine impairment reporting severe adverse gastrointestinal reactions (5.6). Neoplasia syndrome type 2 (MEN 2). -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

Subcutaneous Semaglutide, Dulaglutide and Liraglutide 1.2Mg for the Treatment of Type
North Central London Joint Formulary Committee Factsheet Subcutaneous SEMAGLUTIDE▼ (Ozempic®), DULAGLUTIDE▼ (Trulicity®) and LIRAGLUTIDE 1.2mg (Victoza®) Treatment of Type 2 Diabetes Mellitus Start date: December 2019 Review date: August 2022 Document Control Date Version Action July 2016 1.0 New guideline August 2019 1.1 Subcutaneous semaglutide added as the preferred GLP-1 receptor agonist November 2019 1.2 Supply quantities added Agreed by NCL Shared Care Group: December 2019 FACTSHEET TO FACILITATE PRESCRIBING PLEASE NOTE THIS IS NOT A SHARED CARE GUIDELINE, NOR IS IT A FULL SUMMARY OF DRUG INFORMATION. ALWAYS REFER TO THE MOST RECENT BNF AND/OR SUMMARY OF PRODUCT CHARACTERISTICS. Disclaimer This Fact Sheet is registered at North Central London (NCL) Joint Formulary Committee (JFC) and is intended solely for use by healthcare professionals to aid the treatment of patients within NCL. However, this fact sheet is for guidance only, its interpretation and application remains the responsibility of the individual clinician. If in doubt, contact a senior colleague or expert. Clinicians are advised to refer to the manufacturer’s current prescribing information before treating individual patients. The authors and NCL JFC accept no liability for use of this information from this beyond its intended use. While we have tried to compile accurate information in this document, and to keep it updated in a timely manner, we cannot guarantee that it is fully complete and correct at all times. If you identify information within this document that is inaccurate, please report this to the [email protected]. If a patient is harmed as a consequence of following this document, please complete a local incident report and inform [email protected]. -

The Sodium Glucose Cotransporter Type 2 Inhibitor Empagliflozin Preserves B-Cell Mass and Restores Glucose Homeostasis in the Male Zucker Diabetic Fatty Rat
1521-0103/350/3/657–664$25.00 http://dx.doi.org/10.1124/jpet.114.213454 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 350:657–664, September 2014 Copyright ª 2014 by The American Society for Pharmacology and Experimental Therapeutics The Sodium Glucose Cotransporter Type 2 Inhibitor Empagliflozin Preserves b-Cell Mass and Restores Glucose Homeostasis in the Male Zucker Diabetic Fatty Rat Henrik H. Hansen, Jacob Jelsing, Carl Frederik Hansen, Gitte Hansen, Niels Vrang, Michael Mark, Thomas Klein, and Eric Mayoux Gubra, Hørsholm, Denmark (H.H.H., J.J., C.F.H., G.H., N.V.); and Boehringer Ingelheim Pharma, Biberach, Germany (M.M., T.K., E.M.) Received January 22, 2014; accepted July 2, 2014 Downloaded from ABSTRACT Type 2 diabetes is characterized by impaired b-cell function at week 8 of treatment compared with week 4, those of empagliflozin associated with progressive reduction of insulin secretion and remained stable throughout the study period. Similarly, empagliflozin b -cell mass. Evidently, there is an unmet need for treatments improved glucose tolerance and preserved insulin secretion jpet.aspetjournals.org with greater sustainability in b-cell protection and antidiabetic after both 4 and 8 weeks of treatment. These effects were efficacy. Through an insulin and b cell–independent mechanism, reflected by less reduction in b-cell mass with empagliflozin or empagliflozin, a specific sodium glucose cotransporter type 2 liraglutide at week 4, whereas only empagliflozin showed b-cell (SGLT-2) inhibitor, may potentially provide longer efficacy. This sparing effects also at week 8. Although this study cannot be study compared the antidiabetic durability of empagliflozin treat- used to dissociate the absolute antidiabetic efficacy among ment (10 mg/kg p.o.) against glibenclamide (3 mg/kg p.o.) and the different mechanisms of drug action, the study demon- liraglutide (0.2 mg/kg s.c.) on deficient glucose homeostasis and strates that empagliflozin exerts a more sustained improve- b-cell function in Zucker diabetic fatty (ZDF) rats. -

PRESCRIBING INFORMATION ------WARNINGS and PRECAUTIONS------These Highlights Do Not Include All the Information Needed to Use JARDIANCE Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use JARDIANCE safely and effectively. See full prescribing information for Ketoacidosis: Assess patients who present with signs and symptoms of JARDIANCE. metabolic acidosis for ketoacidosis, regardless of blood glucose level. If suspected, discontinue JARDIANCE, evaluate and treat promptly. JARDIANCE® (empagliflozin tablets), for oral use Before initiating JARDIANCE, consider risk factors for ketoacidosis. Initial U.S. Approval: 2014 Patients on JARDIANCE may require monitoring and temporary discontinuation of therapy in clinical situations known to predispose to ---------------------------RECENT MAJOR CHANGES--------------------------- ketoacidosis. (5.1) Volume Depletion: Before initiating JARDIANCE, assess volume status Indications and Usage (1) 8/2021 and renal function in patients with impaired renal function, elderly Dosage and Administration (2.1) 6/2021 patients, or patients on loop diuretics. Monitor for signs and symptoms Dosage and Administration (2.2) 8/2021 during therapy. (5.2, 6.1) Dosage and Administration (2.3) – Removed 8/2021 Urosepsis and Pyelonephritis: Evaluate patients for signs and symptoms Contraindications (4) 6/2021 of urinary tract infections and treat promptly, if indicated (5.3) Warnings and Precautions (5.1, 5.2) 6/2021 Hypoglycemia: Consider lowering the dose of insulin secretagogue or Warnings and Precautions (5.3, 5.5) 8/2021 insulin to reduce the risk of hypoglycemia when initiating JARDIANCE Warnings and Precautions (5.9) – Removed 6/2021 (5.4) ----------------------------INDICATIONS AND USAGE--------------------------- Necrotizing Fasciitis of the Perineum (Fournier’s Gangrene): Serious, JARDIANCE is a sodium-glucose co-transporter 2 (SGLT2) inhibitor life-threatening cases have occurred in both females and males. -

Clinical Pharmacology Biopharmaceutics Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 206111Orig1s000 CLINICAL PHARMACOLOGY AND BIOPHARMACEUTICS REVIEW(S) (b) Q=(4) % at 20 minutes for empagliflozin and metformin HCl Review: The Biopharmaceutics review is focused on the evaluation and acceptability of the bioequivalence and dissolution data to support approvability of the proposed FDC tablets. RECOMMENDATION: The bioequivalence results and dissolution method are acceptable. From the Biopharmaceutics perspective, NDA 206111 for Empagliflozin/Metformin Hydrochloride Fixed Dose Combination Tablets is recommended for approval. Signature Signature Digitally signed by Kelly M. Kitchens -S Digitally signed by Tapash K. Ghosh -S DN: c=US, o=U.S. Government, DN: c=US, o=U.S. Government, ou=HHS, Kelly M. Tapash K. ou=FDA, ou=People, ou=HHS, ou=FDA, ou=People, 0.9.2342.19200300.100.1.1=200033657 0.9.2342.19200300.100.1.1=1300148262 , cn=Tapash K. Ghosh -S 4, cn=Kelly M. Kitchens -S Date: 2015.04.15 16:19:26 -04'00' Kitchens -S Date: 2015.04.15 15:55:42 -04'00' Ghosh -S Kelly M. Kitchens, Ph.D. Tapash Ghosh, Ph.D. Acting Biopharmaceutics Lead Acting Biopharmaceutics Branch Chief Office of New Drug Products Office of New Drug Products cc. PSeo. 4 Bioequivalence Study No. 1276.6 8 9 Bioanalytical Results: Analyte Name: Empagliflozin Parameter Standard Curve Samples Concentration (nmol/mL) 1.11 2.22 111 55.4 222 665 998 1110 Inter day Precision 7.5 5.2 2.8 2.3 2.2 2.2 2.6 1.7 (%CV) Inter day Accuracy -0.8 0.6 1.0 0.3 -1.7 0.4 -0.2 0.1 (%bias) Linearity 0.994576 – 0.999437 (range -
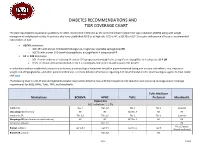
Diabetes Recommendations and Tier Coverage Chart
DIABETES RECOMMENDATIONS AND TIER COVERAGE CHART The American Diabetes Association guidelines for 2020, recommend metformin as the preferred initial treatment for type 2 diabetes (T2DM) along with weight management and physical activity. In patients who have established ASVD or at high risk, CKD, or HF, a SGLT2i or GLP-1 receptor with proven efficacy is recommended independent of A1C. • ASCVD dominates: o GLP-1RA with proven CVD benefit (dulaglutide, liraglutide, injectable semaglutide) OR o SGLT2i with proven CVD benefit (canagliflozin, empagliflozin) if adequate eGFR • HF or CKD dominates: o SGLT2i with evidence of reducing HF and/or CKD progression (empagliflozin, canagliflozin, dapagliflozin) if adequate eGFR OR o If SGLT2i intolerant/contraindicated or eGFR is inadequate, then GLP-1RA with proven CVD benefit In individuals without established cardiovascular disease, pharmacological treatment should be patient-centered taking into account side-effects, cost, impact on weight, risk of hypoglycemia, and other patient preferences. For more detailed information regarding ADA recommendations for pharmacological agents to treat T2DM click here. The following chart is a list of oral and injectable diabetes medications listed by class with their respective A1C reduction and insurance coverage and/or coverage requirements for BCBS, HPHC, Tufts, TMP, and MassHealth. Tufts Medicare Medications BCBSMA HPHC Tufts Preferred MassHealth Biguanides A1C reduction: 1-1.5% metformin Tier 1 Tier 1;2 Tier 1 Tier 1 Covered Glucoghage (metformin) NC NC NC;Tier -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option.