204629Orig1s000
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Diabetes Mellitus
TREATMENT OF DIABETES MELLITUS DIABETES is a condition that affects how the body makes energy from food. Food is broken down into sugar (glucose) in the body and released into the blood. When the blood sugar level rises after a meal, insulin responds to let the sugar into the cells to be used as energy. In diabetes, the body either does not make enough insulin or it stops responding to insulin as well as it should. This results in sugar staying in the blood and leads to serious health problems over time. DIAGNOSIS OF DIABETES1 • A1C Test: Lab test measuring average blood sugar over past two to three months • Fasting Blood Sugar Test: Lab test measuring blood sugar after eight hours of no food or drink • Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and two hours after drinking a specific sugary liquid • Random Blood Sugar Test: Measures blood sugar at a moment in time, without any kind of preparation (like fasting) FASTING BLOOD ORAL GLUCOSE TOLERANCE RANDOM BLOOD RESULT A1C TEST SUGAR TEST TEST SUGAR TEST Diabetes ≥ 6.5% ≥126 mg/dL ≥ 200 mg/dL ≥ 200 mg/dL Prediabetes 5.7 – 6.4% 100 – 125 mg/dL 140 – 199 mg/dL N/A Normal < 5.7% ≤99 mg/dL < 140 mg/dL N/A NON-DRUG TREATMENTS2 THERAPY COST WHAT TO EXPECT Diet (Mediterranean diet) and exercise (30 minutes a day, five days a week of moderate- Weight loss $-$$ intensity exercise); 7% weight loss decreases risk of diabetes3 Psychological intervention $$-$$$ Psychotherapy may reduce diabetic distress and improve glycemic control4,5 nationalcooperativerx.com PRESCRIPTION TREATMENTS -

Step Therapy
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2020 P 3086-9 Program Step Therapy – Diabetes Medications - SGLT2 Inhibitors Medication Farxiga (dapagliflozin)*, Glyxambi (empagliflozin/linagliptan), Invokana (canagliflozin)*, Invokamet (canagliflozin/metformin)*, Invokamet XR (canaglifloxin/metformin extended-release)*, Jardiance (empagliflozin), Qtern (dapagliflozin/saxagliptin)*, Segluromet (ertugliflozin/metformin)*, Steglatro (ertugliflozin)*, Steglujan (ertugliflozin/sitagliptin)*, Xigduo XR (dapagliflozin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 4/2018, 8/2018, 12/2018, 2/2019, 2/2020, 5/2020; 7/2020 Effective Date 10/1/2020; Oxford only: 10/1/2020 1. Background: Farxiga (dapagliflozin)*, Invokana (canagliflozin)*, Jardiance (empagliflozin) and Steglatro (ertugliflozin)* are sodium-glucose co-transporter 2 (SGLT2) inhibitors indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Farxiga*, Invokana* and Jardiance have additional indications. Farxiga* is indicated to reduce the risk of cardiovascular death and hospitalization for heart failure in adults with heart failure (NYHA class II-IV) with reduced ejection fraction. Invokana* is indicated to reduce the risk of major adverse cardiovascular events (cardiovascular death, nonfatal myocardial infarction and nonfatal stroke) in adults with type 2 diabetes mellitus and established cardiovascular disease (CVD), and to reduce the risk of end-stage kidney disease (ESKD), doubling of -

The Sodium Glucose Cotransporter Type 2 Inhibitor Empagliflozin Preserves B-Cell Mass and Restores Glucose Homeostasis in the Male Zucker Diabetic Fatty Rat
1521-0103/350/3/657–664$25.00 http://dx.doi.org/10.1124/jpet.114.213454 THE JOURNAL OF PHARMACOLOGY AND EXPERIMENTAL THERAPEUTICS J Pharmacol Exp Ther 350:657–664, September 2014 Copyright ª 2014 by The American Society for Pharmacology and Experimental Therapeutics The Sodium Glucose Cotransporter Type 2 Inhibitor Empagliflozin Preserves b-Cell Mass and Restores Glucose Homeostasis in the Male Zucker Diabetic Fatty Rat Henrik H. Hansen, Jacob Jelsing, Carl Frederik Hansen, Gitte Hansen, Niels Vrang, Michael Mark, Thomas Klein, and Eric Mayoux Gubra, Hørsholm, Denmark (H.H.H., J.J., C.F.H., G.H., N.V.); and Boehringer Ingelheim Pharma, Biberach, Germany (M.M., T.K., E.M.) Received January 22, 2014; accepted July 2, 2014 Downloaded from ABSTRACT Type 2 diabetes is characterized by impaired b-cell function at week 8 of treatment compared with week 4, those of empagliflozin associated with progressive reduction of insulin secretion and remained stable throughout the study period. Similarly, empagliflozin b -cell mass. Evidently, there is an unmet need for treatments improved glucose tolerance and preserved insulin secretion jpet.aspetjournals.org with greater sustainability in b-cell protection and antidiabetic after both 4 and 8 weeks of treatment. These effects were efficacy. Through an insulin and b cell–independent mechanism, reflected by less reduction in b-cell mass with empagliflozin or empagliflozin, a specific sodium glucose cotransporter type 2 liraglutide at week 4, whereas only empagliflozin showed b-cell (SGLT-2) inhibitor, may potentially provide longer efficacy. This sparing effects also at week 8. Although this study cannot be study compared the antidiabetic durability of empagliflozin treat- used to dissociate the absolute antidiabetic efficacy among ment (10 mg/kg p.o.) against glibenclamide (3 mg/kg p.o.) and the different mechanisms of drug action, the study demon- liraglutide (0.2 mg/kg s.c.) on deficient glucose homeostasis and strates that empagliflozin exerts a more sustained improve- b-cell function in Zucker diabetic fatty (ZDF) rats. -

PRESCRIBING INFORMATION ------WARNINGS and PRECAUTIONS------These Highlights Do Not Include All the Information Needed to Use JARDIANCE Safely and Effectively
HIGHLIGHTS OF PRESCRIBING INFORMATION -----------------------WARNINGS AND PRECAUTIONS------------------------ These highlights do not include all the information needed to use JARDIANCE safely and effectively. See full prescribing information for Ketoacidosis: Assess patients who present with signs and symptoms of JARDIANCE. metabolic acidosis for ketoacidosis, regardless of blood glucose level. If suspected, discontinue JARDIANCE, evaluate and treat promptly. JARDIANCE® (empagliflozin tablets), for oral use Before initiating JARDIANCE, consider risk factors for ketoacidosis. Initial U.S. Approval: 2014 Patients on JARDIANCE may require monitoring and temporary discontinuation of therapy in clinical situations known to predispose to ---------------------------RECENT MAJOR CHANGES--------------------------- ketoacidosis. (5.1) Volume Depletion: Before initiating JARDIANCE, assess volume status Indications and Usage (1) 8/2021 and renal function in patients with impaired renal function, elderly Dosage and Administration (2.1) 6/2021 patients, or patients on loop diuretics. Monitor for signs and symptoms Dosage and Administration (2.2) 8/2021 during therapy. (5.2, 6.1) Dosage and Administration (2.3) – Removed 8/2021 Urosepsis and Pyelonephritis: Evaluate patients for signs and symptoms Contraindications (4) 6/2021 of urinary tract infections and treat promptly, if indicated (5.3) Warnings and Precautions (5.1, 5.2) 6/2021 Hypoglycemia: Consider lowering the dose of insulin secretagogue or Warnings and Precautions (5.3, 5.5) 8/2021 insulin to reduce the risk of hypoglycemia when initiating JARDIANCE Warnings and Precautions (5.9) – Removed 6/2021 (5.4) ----------------------------INDICATIONS AND USAGE--------------------------- Necrotizing Fasciitis of the Perineum (Fournier’s Gangrene): Serious, JARDIANCE is a sodium-glucose co-transporter 2 (SGLT2) inhibitor life-threatening cases have occurred in both females and males. -

Clinical Pharmacology Biopharmaceutics Review(S)
CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: 206111Orig1s000 CLINICAL PHARMACOLOGY AND BIOPHARMACEUTICS REVIEW(S) (b) Q=(4) % at 20 minutes for empagliflozin and metformin HCl Review: The Biopharmaceutics review is focused on the evaluation and acceptability of the bioequivalence and dissolution data to support approvability of the proposed FDC tablets. RECOMMENDATION: The bioequivalence results and dissolution method are acceptable. From the Biopharmaceutics perspective, NDA 206111 for Empagliflozin/Metformin Hydrochloride Fixed Dose Combination Tablets is recommended for approval. Signature Signature Digitally signed by Kelly M. Kitchens -S Digitally signed by Tapash K. Ghosh -S DN: c=US, o=U.S. Government, DN: c=US, o=U.S. Government, ou=HHS, Kelly M. Tapash K. ou=FDA, ou=People, ou=HHS, ou=FDA, ou=People, 0.9.2342.19200300.100.1.1=200033657 0.9.2342.19200300.100.1.1=1300148262 , cn=Tapash K. Ghosh -S 4, cn=Kelly M. Kitchens -S Date: 2015.04.15 16:19:26 -04'00' Kitchens -S Date: 2015.04.15 15:55:42 -04'00' Ghosh -S Kelly M. Kitchens, Ph.D. Tapash Ghosh, Ph.D. Acting Biopharmaceutics Lead Acting Biopharmaceutics Branch Chief Office of New Drug Products Office of New Drug Products cc. PSeo. 4 Bioequivalence Study No. 1276.6 8 9 Bioanalytical Results: Analyte Name: Empagliflozin Parameter Standard Curve Samples Concentration (nmol/mL) 1.11 2.22 111 55.4 222 665 998 1110 Inter day Precision 7.5 5.2 2.8 2.3 2.2 2.2 2.6 1.7 (%CV) Inter day Accuracy -0.8 0.6 1.0 0.3 -1.7 0.4 -0.2 0.1 (%bias) Linearity 0.994576 – 0.999437 (range -

SGLT2) Inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM
Sodium-glucose cotransporter-2 (SGLT2) inhibitors (Gliflozins) in Adults with Type 2 Diabetes (T2DM) There are currently four SGLT2 inhibitors (canagliflozin, dapagliflozin, empagliflozin and ertugliflozin) licensed in the UK for the management of adults with T2DM. No head to head trials between the SGLT2 inhibitors have been conducted. As at December 2019, clinical outcome data is available for three of the four SGLT2 inhibitors around their cardiovascular effects in people with T2DM. Ertugliflozin is still to report on this data. This document summarises the key prescribing considerations. NICE Technology Appraisal Recommendation NICE makes recommendations for when SGLT2 inhibitors can be considered in adults with T2DM; Hertfordshire Medicines Management Committee Recommendations are in line with NICE guidance: Monotherapy NICE TA 390: Canagliflozin, Dapagliflozin and Empagliflozin and NICE TA 572: Ertugliflozin as monotherapies for treating T2DM Monotherapy recommended as option in adults for whom metformin is contraindicated or not tolerated and when diet & exercise alone do not provide adequate glycaemic control, only if: •a DPP‑4 inhibitor would otherwise be prescribed and •a sulfonylurea or pioglitazone is not appropriate. Dual therapy NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin, TA 572: Ertugliflozin as combination therapies for treating T2DM In a dual therapy regimen in combination with metformin is recommended as an option, only if: •a sulfonylurea is contraindicated or not tolerated or •the person is at significant risk of hypoglycaemia or its consequences. In combination with insulin NICE TA 315: Canagliflozin, NICE TA288: Dapagliflozin, TA 336: Empagliflozin in combination with insulin with or without other antidiabetic drugs is recommended as an option. -
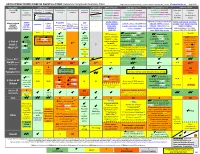
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

Cost-Effectiveness of Empagliflozin Versus Canagliflozin, Dapagliflozin
Emerging technologies, pharmacology and therapeutics Open access Original research BMJ Open Diab Res Care: first published as 10.1136/bmjdrc-2020-001313 on 3 May 2021. Downloaded from Cost-effectivenessofempagliflozin versuscanagliflozin,dapagliflozin,or standardofcareinpatientswithtype2 diabetesandestablished cardiovasculardisease Odette S Reifsnider ,1 Anuraag R Kansal,1 Pranav K Gandhi,2 Lael Cragin,1 Sarah B Brand,1 Egon Pfarr,3 Kyle Fahrbach,4 Anastasia Ustyugova3 To cite: Reifsnider OS, ABSTRACT Kansal AR, Gandhi PK, Introduction Empagliflozin, a sodium- glucose co- Significance of this study et al. Cost- effectiveness transporter-2 (SGLT-2) inhibitor, is approved in the USA of empagliflozin versus to reduce risk of cardiovascular (CV) death in adults What is already known about this subject? canagliflozin, dapagliflozin, with type 2 diabetes mellitus (T2DM) and established CV ► The sodium glucose co- transporter-2 inhibitor (SGLT- or standard of care in 2) empagliflozin is Food and Drug Administration patients with type 2 disease, based on EMPA-REG OUTCOME (Empagliflozin Cardiovascular Outcome Event Trial in Type 2 Diabetes (FDA) approved to reduce the risk of cardiovascular diabetes and established (CV) death in adults with type 2 diabetes mellitus cardiovascular disease. Mellitus Patients) trial results. Empagliflozin reduced major (T2DM) and established CV disease (CVD) based BMJ Open Diab Res Care adverse CV event (MACE) by 14%, CV death by 38%, and 2021;9:e001313. doi:10.1136/ hospitalization for heart failure (HHF) by 35% vs placebo, on the EMPA- REG OUTCOME trial, which showed a bmjdrc-2020-001313 each on top of standard of care (SoC). -

Management of Type 2 Diabetes Mellitus Dr Naomi Achong Endocrinologist MBBS(Hons) Bsc FRACP Phd Overview
Management of Type 2 Diabetes Mellitus Dr Naomi Achong Endocrinologist MBBS(Hons) BSc FRACP PhD Overview • Overview of T2DM & glycaemic targets • Treatment after metformin – newer agents on the market • SGLT2 inhibitors • DPP4 agonists • GLP1 antagonists • Insulin options • Newer options – coformulation Diagnosis • ADS position statement • Criteria: • HbA1c > 6.5% • Fasting glucose > 7mmol/L. • Random glucose > 11.1mmol/L • GTT showing fasting > 7 or 2hr > 11.1mmol/L • Patients with IGT have an increased risk of death and vascular disease (regardless of progression to diabetes) as well as microvascular complications • Risk of progression to T2DM is reduced by 58% with lifestyle modification and 31% with metformin 1.The DECODE Study. Arch Intern Med 2001; 161:397-405 2. Singleton JR et al. Diabetes 2003;52(12):2867-2873 3. Diabetes Prevention Program Research Group. N Engl J Med 2002; 346:393-403 Optimising health outcomes in diabetes • Glucose control • Smoking cessation • Blood pressure control • Lipid management with priority to statins • Some circumstances, antiplatelet therapy ADA/EASD – 2015 position statement • Glycaemic targets need to be individualised • Based on modifiable and non-modifiable factors 1. Inzucchi S.E., Bergenstal R.M., Buse J.B., Diamant M., Ferrannini E., Nauck M. et al Diabetologia. 2015; 58: 429-442 1. Inzucchi S.E. et al. Diabetologia. 2015; 58: 429-442 Importance of glycaemic control GOOD GLYCAEMIC CONTROL Reduces diabetes-related complications Reduces total diabetes-related costs UKPDS1 Retrospective database analysis2 1% mean HbA1c reduction results in: HbA1c ≤7% continuously for 1 year results in . 37% 14% 21% 25% Which included: Myocardial 22% lower diabetes infarction medical costs Diabetes-related 28% lower diabetes mortality Diabetes-related pharmacy costs treatment costs Microvascular complications . -

The Na+/Glucose Cotransporter Inhibitor Canagliflozin Activates
2784 Diabetes Volume 65, September 2016 Simon A. Hawley,1 Rebecca J. Ford,2 Brennan K. Smith,2 Graeme J. Gowans,1 Sarah J. Mancini,3 Ryan D. Pitt,2 Emily A. Day,2 Ian P. Salt,3 Gregory R. Steinberg,2 and D. Grahame Hardie1 The Na+/Glucose Cotransporter Inhibitor Canagliflozin Activates AMPK by Inhibiting Mitochondrial Function and Increasing Cellular AMP Levels Diabetes 2016;65:2784–2794 | DOI: 10.2337/db16-0058 Canagliflozin, dapagliflozin, and empagliflozin, all recently transporters that carry glucose across apical membranes approved for treatment of type 2 diabetes, were derived of polarized epithelial cells against concentration gradi- from the natural product phlorizin. They reduce hypergly- ents, driven by Na+ gradients. SGLT1 is expressed in the cemia by inhibiting glucose reuptake by sodium/glucose small intestine and responsible for most glucose uptake cotransporter (SGLT) 2 in the kidney, without affecting across the brush border membrane of enterocytes, whereas intestinal glucose uptake by SGLT1. We now report that SGLT2 is expressed in the kidney and responsible for most fl canagli ozin also activates AMPK, an effect also seen glucose readsorption in the convoluted proximal tubules. with phloretin (the aglycone breakdown product of The first identified SGLT inhibitor was a natural product, fi phlorizin), but not to any signi cant extent with dapagli- phlorizin, which is broken down in the small intestine to flozin, empagliflozin, or phlorizin. AMPK activation oc- phloretin, the aglycone form (Fig. 1). Although phlorizin curred at canagliflozin concentrations measured in had beneficial effects in hyperglycemic animals (2), it in- human plasma in clinical trials and was caused by hibits SGLT1 and SGLT2, causing adverse gastrointestinal inhibition of Complex I of the respiratory chain, leading effects (3). -

JARDIANCE (Empagliflozin)
HIGHLIGHTS OF PRESCRIBING INFORMATION • Ketoacidosis: Assess patients who present with signs and symptoms of These highlights do not include all the information needed to use metabolic acidosis for ketoacidosis, regardless of blood glucose level. If JARDIANCE safely and effectively. See full prescribing information for suspected, discontinue JARDIANCE, evaluate and treat promptly. JARDIANCE. Before initiating JARDIANCE, consider risk factors for ketoacidosis. Patients on JARDIANCE may require monitoring and temporary JARDIANCE® (empagliflozin) tablets, for oral use discontinuation of therapy in clinical situations known to predispose to Initial U.S. Approval: 2014 ketoacidosis. (5.2) • Acute kidney injury and impairment in renal function: Consider ---------------------------RECENT MAJOR CHANGES--------------------------- temporarily discontinuing in settings of reduced oral intake or fluid Indications and Usage (1) 12/2016 losses. If acute kidney injury occurs, discontinue and promptly treat. Warnings and Precautions (5) 12/2016 Monitor renal function during therapy. (5.3) • Urosepsis and Pyelonephritis: Evaluate patients for signs and symptoms ----------------------------INDICATIONS AND USAGE-------------------------- of urinary tract infections and treat promptly, if indicated (5.4) JARDIANCE is a sodium-glucose co-transporter 2 (SGLT2) inhibitor • Hypoglycemia: Consider lowering the dose of insulin secretagogue or indicated: insulin to reduce the risk of hypoglycemia when initiating JARDIANCE • as an adjunct to diet and exercise to -

Intervention Summary of Information on Empagliflozin in COVID-19
Intervention Empagliflozin 10mg once daily by mouth for up to 28 days (stopped at discharge if sooner) Summary of information on empagliflozin in COVID-19 Sodium glucose co-transporter 2 inhibitors (SGLT-2i), such as empagliflozin, are routinely used in the treatment of type 2 diabetes and have also been shown to have rapid effects in other diseases, such as heart failure1. In COVID-19, they may be beneficial through multiple mechanisms including their impacts on energy metabolism2,3,endothelial function4, oxidative stress4, inflammation5 and haemodynamic decongestion6. The DARE-19 trial compared the SGLT-2i dapagliflozin with placebo for 30 days among 1250 hospitalised COVID-19 patients with mild hypoxia and at least one co-morbid disease risk factor7. The treatment was well-tolerated. The hazard ratio for the composite primary outcome of organ failure or death was 0.80 (95% confidence interval 0.58-1.10)8; although this was not statistically significant the trial lacked power and the results support the rationale for a larger trial. Potential harm Common side effects include genital candidiasis and hypoglycaemia when used in combination with insulin or insulin secretagogues (eg, sulphonylureas). Rare, but important, side effects include ketoacidosis (particularly in type 1 diabetes mellitus). Mitigating measures are described below and in the study protocol. SGLT-2i are not considered to be safe in pregnancy and breastfeeding so these women will be excluded from the comparison. Based on the mode of action, there are no theoretical grounds to modify the dose in elderly patients or those with hepatic impairment. We do not recommend a dose modification in renal impairment as outlined below.