Comparison Between the Clinical Efficacy of Linagliptin and Sitagliptin
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Treatment of Diabetes Mellitus
TREATMENT OF DIABETES MELLITUS DIABETES is a condition that affects how the body makes energy from food. Food is broken down into sugar (glucose) in the body and released into the blood. When the blood sugar level rises after a meal, insulin responds to let the sugar into the cells to be used as energy. In diabetes, the body either does not make enough insulin or it stops responding to insulin as well as it should. This results in sugar staying in the blood and leads to serious health problems over time. DIAGNOSIS OF DIABETES1 • A1C Test: Lab test measuring average blood sugar over past two to three months • Fasting Blood Sugar Test: Lab test measuring blood sugar after eight hours of no food or drink • Oral Glucose Tolerance Test (OGTT): Measures blood sugar before and two hours after drinking a specific sugary liquid • Random Blood Sugar Test: Measures blood sugar at a moment in time, without any kind of preparation (like fasting) FASTING BLOOD ORAL GLUCOSE TOLERANCE RANDOM BLOOD RESULT A1C TEST SUGAR TEST TEST SUGAR TEST Diabetes ≥ 6.5% ≥126 mg/dL ≥ 200 mg/dL ≥ 200 mg/dL Prediabetes 5.7 – 6.4% 100 – 125 mg/dL 140 – 199 mg/dL N/A Normal < 5.7% ≤99 mg/dL < 140 mg/dL N/A NON-DRUG TREATMENTS2 THERAPY COST WHAT TO EXPECT Diet (Mediterranean diet) and exercise (30 minutes a day, five days a week of moderate- Weight loss $-$$ intensity exercise); 7% weight loss decreases risk of diabetes3 Psychological intervention $$-$$$ Psychotherapy may reduce diabetic distress and improve glycemic control4,5 nationalcooperativerx.com PRESCRIPTION TREATMENTS -

Supplementary Material
Supplementary material Table S1. Search strategy performed on the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL). 1. Randomi*ed study OR random allocation OR Randomi*ed controlled trial OR Random* Control* trial OR RCT Epidemiological study 2. sodium glucose cotransporter 2 OR sodium glucose cotransporter 2 inhibitor* OR sglt2 inhibitor* OR empagliflozin OR dapagliflozin OR canagliflozin OR ipragliflozin OR tofogliflozin OR ertugliflozin OR sotagliflozin OR sergliflozin OR remogliflozin 3. 1 AND 2 1 Table S2. Safety outcomes of empagliflozin and linagliptin combination therapy compared with empagliflozin or linagliptin monotherapy in treatment naïve type 2 diabetes patients Safety outcome Comparator 1 Comparator 2 I2 RR [95% CI] Number of events Number of events / / total subjects total subjects i. Empagliflozin + linagliptin vs empagliflozin monotherapy Empagliflozin + Empagliflozin linagliptin monotherapy ≥ 1 AE(s) 202/272 203/270 77% 0.99 [0.81, 1.21] ≥ 1 drug-related 37/272 38/270 0% 0.97 [0.64, 1.47] AE(s) ≥ 1 serious AE(s) 13/272 19/270 0% 0.68 [0.34, 1.35] Hypoglycaemia* 0/272 5/270 0% 0.18 [0.02, 1.56] UTI 32/272 25/270 29% 1.28 [0.70, 2.35] Events suggestive 12/272 13/270 9% 0.92 [0.40, 2.09] of genital infection i. Empagliflozin + linagliptin vs linagliptin monotherapy Empagliflozin + Linagliptin linagliptin monotherapy ≥ 1 AE(s) 202/272 97/135 0% 1.03 [0.91, 1.17] ≥ 1 drug-related 37/272 17/135 0% 1.08 [0.63, 1.84] AE(s) ≥ 1 serious AE(s) 13/272 2/135 0% 3.22 [0.74, 14.07] Hypoglycaemia* 0/272 1/135 NA 0.17 [0.01, 4.07] UTI 32/272 12/135 0% 1.32 [0.70, 2.49] Events suggestive 12/272 4/135 0% 1.45 [0.47, 4.47] of genital infection RR, relative risk; AE, adverse event; UTI, urinary tract infection. -

Januvia (Sitagliptin) Tablets
CENTER FOR DRUG EVALUATION AND RESEARCH Approval Package for: APPLICATION NUMBER: NDA 021995/S-013 Trade Name: JANUVIA Generic Name: Sitagliptin Sponsor: Merck & Co., Inc. Approval Date: 12/28/2009 Indications: JANUVIA is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 021995/S-013 CONTENTS Reviews / Information Included in this NDA Review. Approval Letter X Other Action Letters X Labeling X Summary Review Officer/Employee List Office Director Memo Cross Discipline Team Leader Review Medical Review(s) X Chemistry Review(s) Environmental Assessment Pharmacology Review(s) X Statistical Review(s) Microbiology Review(s) Clinical Pharmacology/Biopharmaceutics Review(s) Risk Assessment and Risk Mitigation Review(s) X Proprietary Name Review(s) Other Review(s) X Administrative/Correspondence Document(s) X CENTER FOR DRUG EVALUATION AND RESEARCH APPLICATION NUMBER: NDA 021995/S-013 APPROVAL LETTER DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 NDA 021995/S-013 SUPPLEMENT APPROVAL Merck & Co., Inc. Attention: Richard J. Swanson, Ph.D. Director, Regulatory Affairs P.O. Box 1000, UG2C-50 North Wales, PA 19454-1099 Dear Dr. Swanson: Please refer to your supplemental new drug application (S-013) dated and received March 5, 2009, submitted under section 505(b) of the Federal Food, Drug, and Cosmetic Act (FDCA) for Januvia (sitagliptin) tablets. We also refer to your supplemental new drug application (b) (4) dated and received November 13, 2009. Your submission of November 13, 2009, also constitutes a complete response to our October 16, 2009, action letter for supplemental application S-013. -

Pharmacokinetics of Omarigliptin, a Once-Weekly Dipeptidyl Peptidase-4 Inhibitor
Available online a t www.derpharmachemica.com ISSN 0975-413X Der Pharma Chemica, 2016, 8(12):292-295 CODEN (USA): PCHHAX (http://derpharmachemica.com/archive.html) Mini-review: Pharmacokinetics of Omarigliptin, a Once-weekly Dipeptidyl Peptidase-4 Inhibitor Nermeen Ashoush a,b aClinical Pharmacy and Pharmacy Practice Department, Faculty of Pharmacy, British University in Egypt, El- Sherouk city, Cairo 11837, Egypt. bHead of Health Economics Unit, Center for Drug Research and Development (CDRD), Faculty of Pharmacy, British University in Egypt, El-Sherouk city, Cairo 11837, Egypt. _____________________________________________________________________________________________ ABSTRACT The dipeptidyl peptidase-4 (DPP-4) inhibitors are novel oral hypoglycemic drugs which have been in clinical use for the past 10 years. The drugs are safe, weight neutral and widely prescribed. There are currently many gliptins approved by FDA, namely sitagliptin, vildagliptin, saxagliptin, linagliptin, alogliptin with several more in advanced stages of development. The gliptins may possess cardiovascular protective effects and their administration may promote β-cell survival; claims currently being evaluated in clinical and preclinical studies. The gliptins are an optional second-line therapy after metformin; they are generally well tolerated with low risk of hypoglycemia. The various compounds differ with respect to their pharmacokinetic properties; however, their clinical efficacy appears to be similar. The clinical differences between the various compounds -

TREATMENT of TYPE 2 DIABETES with BIPHASIC INSULIN ANALOGUES *Ali A
TREATMENT OF TYPE 2 DIABETES WITH BIPHASIC INSULIN ANALOGUES *Ali A. Rizvi Professor of Medicine, Department of Medicine and Director, Division of Endocrinology, University of South Carolina School of Medicine, Columbia, South Carolina, USA *Correspondence to [email protected] Disclosure: The author has received grant support, as principal investigator at the University of South Carolina site, from the National Institutes of Health (NIH) for the SPRINT Trial (Contract Number: HHSN268200900040C, ClinicalTrials.gov Identifier: NCT01206062). The contents of this paper do not necessarily represent the views of the NIH. Received: 29.03.16 Accepted: 09.09.16 Citation: EMJ Diabet. 2016;4[1]:74-83. ABSTRACT The majority of patients with Type 2 diabetes require insulin therapy for treating hyperglycaemia. There are several regimens available for insulin initiation and maintenance. Insulin analogues have been developed to mimic normal physiology as closely as possible. Biphasic analogues can target both fasting and postprandial hyperglycaemia, with the added advantage of being premixed and thus convenient for the patient. A practical and feasible option is to initiate insulin with one or more biphasic preparations at mealtimes, thus providing both basal and prandial coverage. Individual titration of dose and frequency of daily injections with biphasic insulin preparations has the potential for improving glycaemic control with a high degree of patient acceptance. Drawbacks include a more rigid regimen, a relative lack of flexibility, and a somewhat higher degree of glycaemic variability and hypoglycaemia when compared to multiple daily basal-bolus injections. Awareness of the advantages and limitations of biphasic insulin analogues can assist clinicians in their appropriate use for the treatment of patients with Type 2 diabetes. -

Sitagliptin: a New Class of Oral Drug for Type 2 Diabetes
JK SCIENCE DRUG REVIEW Sitagliptin: a New Class of Oral Drug for Type 2 Diabetes Dinesh K. Badyal, Jasleen Kaur Introduction Pharmacokinetics Type 2 diabetes is the most common form of the Bioavailability of sitagliptin is approximately 87%. Half- disease, accounting for about 90% to 95 % of all diagnosed life is between 8-14 hours. It is 38% bound to plasma cases of diabetes. In type 2 diabetes, the body does not proteins. It undergoes limited metabolism via CYP3A4 produce enough insulin or the cells ignore the insulin. and CYP2C8. Elimination is mainly through urine (5, 6). Over time, high blood sugar levels can increase the risk Clinical Use for serious complications, including heart disease, In October 2006, the U.S. Food and Drug blindness, nerve damage and kidney damage (1). Any Administration (FDA) approved sitagliptin as new oral hypoglycemic drug that can increase the control monotherapy and as add-on therapy to either of two other of blood glucose with fewer adverse effects in patients types of oral diabetes medications, metformin or with diabetes may be welcomed. Sitagliptin is the first thiazolidinediones to improve blood glucose control in and only prescription medication in a new class of oral patients with type 2 diabetes when diet and exercise are antihyperglycemic agents, which enhance the body's own not enough (5). In March, 2007 it was approved in ability to lower blood glucose when it is elevated (2). European Union. Sitagliptin is currently approved in 42 Mechanism of Action countries (7). The recommended dose of sitagliptin is Sitagliptin prolongs the activity of proteins that increase 100 mg once daily. -

Safety and Efficacy of Omarigliptin (MK-3102), a Novel Once-Weekly
2106 Diabetes Care Volume 38, November 2015 fi Wayne H.-H. Sheu,1 Ira Gantz,2 Safety and Ef cacy of Omarigliptin Menghui Chen,2 Shailaja Suryawanshi,2 Arpana Mirza,2 Barry J. Goldstein,2 (MK-3102), a Novel Once-Weekly Keith D. Kaufman,2 and Samuel S. Engel2 DPP-4 Inhibitor for the Treatment of Patients With Type 2 Diabetes Diabetes Care 2015;38:2106–2114 | DOI: 10.2337/dc15-0109 OBJECTIVE This study was conducted to determine the optimal dose of omarigliptin, a once- weekly (q.w.) dipeptidyl peptidase IV (DPP-4) inhibitor, for the treatment of patients with type 2 diabetes and evaluate the long-term safety of that dose. RESEARCH DESIGN AND METHODS In a multicenter, double-blind, 12-week, dose-range finding study, 685 oral antihy- perglycemic agent-na¨ıve or washed-out subjects with type 2 diabetes were random- ized to one of five once-weekly doses of omarigliptin (0.25 mg, 1 mg, 3 mg, 10 mg, or 25 mg) or placebo. The primary efficacy end point was change from baseline in HbA1c, and secondary end points were 2-h postmeal glucose (PMG) and fasting plasma glucose (FPG). Analysis included all patients who received at least one dose of the study medication. Subjects who completed the base study were eligible to enter a 66-week extension study. RESULTS Once-weekly treatment for 12 weeks with omarigliptin provided dose-related reduc- 1Division of Endocrinology and Metabolism, De- partment of Internal Medicine, Taichung Veterans EMERGING TECHNOLOGIES AND THERAPEUTICS tions in HbA , 2-h PMG, and FPG. -

Januvia (Sitagliptin)
UnitedHealthcare Pharmacy Clinical Pharmacy Programs Program Number 2021 P 3084-7 Program Step Therapy – Diabetes Medications- DPP4 Inhibitors Medication Januvia (sitagliptin)*, Janumet (sitagliptin/metformin immediate- release)*, Janumet XR (sitagliptin/metformin extended-release)* P&T Approval Date 10/2016, 10/2017, 1/2018, 10/2019, 4/2020, 5/2020, 5/2021 Effective Date 8/1/2021; Oxford only: 8/1/2021 1. Background: Januvia (sitagliptin)* is indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus. Janumet (sitagliptin/metformin)* and Janumet XR (sitagliptin/metformin extended-release)* are indicated as an adjunct to diet and exercise to improve glycemic control in adults with type 2 diabetes mellitus when treatment with both sitagliptin and metformin/metformin extended-release is appropriate. 2. Coverage Criteriaa: A. Januvia* will be approved based on the following criterion: 1. History of a three month trial resulting in a therapeutic failure, contraindication (e.g. risk factors for heart failure), or intolerance to both of the following (list reason for therapeutic failure, contraindication, or intolerance)b: a. Tradjenta (linagliptin) -AND- b. One of the following: (1) Nesina (alogliptin) (2) Onglyza (saxagliptin) Authorization will be issued for 12 months B. Janumet* and Janumet XR* will be approved based on the following criterion: 1. History of a three month trial resulting in a therapeutic failure, contraindication (e.g. risk factors for heart failure), or intolerance to all of the following (list reason for therapeutic failure, contraindication, or intolerance)b: a. Jentadueto (linagliptin/metformin immediate-release)/Jentadueto XR (linagliptin/metformin extended-release) -AND- b. -

Assessment of the Pharmacokinetic Interaction Between the Novel DPP-4 Inhibitor Linagliptin Andasulfonylurea,Glyburide,Inhealthysubjects
Drug Metab. Pharmacokinet. 26 (2): 123129 (2011). Copyright © 2011 by the Japanese Society for the Study of Xenobiotics (JSSX) Regular Article Assessment of the Pharmacokinetic Interaction between the Novel DPP-4 Inhibitor Linagliptin andaSulfonylurea,Glyburide,inHealthySubjects Ulrike GRAEFE-MODY1,*, Peter ROSE2,ArneRING2,KerstinZANDER2, Mario IOVINO2 and Hans-Juergen WOERLE1 1Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany 2Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach, Germany Full text of this paper is available at http://www.jstage.jst.go.jp/browse/dmpk Summary: The aim of this study was to investigate the effect of the dipeptidyl peptidase-4 inhibitor linagliptin on the pharmacokinetics of glyburide (a CYP2C9 and CYP3A4 substrate) and vice versa.This randomized, open-label, three-period, two-way crossover study examined the effects of co-administration of multiple oral doses of linagliptin (5 mg/day © 6 days) and single doses of glyburide (1.75 mg/day © 1day)on the relative bioavailability of either compound in healthy subjects (n = 20, age 1855 years). Coadmin- istration of glyburide did not alter the steady-state pharmacokinetics of linagliptin. Geometric mean ratios (GMRs) [90% CI] for (linagliptin + glyburide)/linagliptin AUC¸,ss and Cmax,ss were 101.7% [97.7105.8%] and 100.8% [89.0114.3%], respectively. For glyburide, there was a slight reduction in exposure of ³14% when coadministered with linagliptin (GMRs [90% CI] for (glyburide + linagliptin)/glyburide AUC0¨ and Cmax were 85.7% [79.892.1%] and 86.2% [79.693.3%], respectively). However, this was not seen as clinically relevant due to the absence of a reliable doseresponse relationship and the known large pharmacokinetic interindividual variability of glyburide. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -
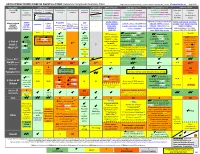
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances The
International Journal of Molecular Sciences Article The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances the Contractile Recovery of Mouse Hearts at a Concentration Equivalent to that Achieved with Standard Dosing in Humans 1, 1, 1 1 Sri Nagarjun Batchu y, Veera Ganesh Yerra y , Youan Liu , Suzanne L. Advani , Thomas Klein 2 and Andrew Advani 1,* 1 Keenan Research Center for Biomedical Science and Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON M5B 1T8, Canada; [email protected] (S.N.B.); [email protected] (V.G.Y.); [email protected] (Y.L.); [email protected] (S.L.A.) 2 Department of Cardiometabolic Diseases Research, Boehringer Ingelheim Pharma GmbH & Co. KG, 88397 Biberach, Germany; [email protected] * Correspondence: [email protected]; Tel.: +1-416-864-6060 (ext. 8413) These authors contributed equally to this work. y Received: 14 June 2020; Accepted: 9 August 2020; Published: 11 August 2020 Abstract: Despite a similar mechanism of action underlying their glucose-lowering effects in type 2 diabetes, dipeptidyl peptidase-4 (DPP-4) inhibitors have diverse molecular structures, raising the prospect of agent-specific, glucose-independent actions. To explore the issue of possible DPP-4 inhibitor cardiac heterogeneity, we perfused different DPP-4 inhibitors to beating mouse hearts ex vivo, at concentrations equivalent to peak plasma levels achieved in humans with standard dosing. We studied male and female mice, young non-diabetic mice, and aged diabetic high fat diet-fed mice and observed that linagliptin enhanced recovery after ischemia-reperfusion, whereas sitagliptin, alogliptin, and saxagliptin did not.