Non-Surgical and Non-ICU Patients with Type 2
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Higher Mortality Rate in Moderate-To-Severe Thoracoabdominal Injury Patients with Admission Hyperglycemia Than Nondiabetic Normoglycemic Patients
International Journal of Environmental Research and Public Health Article Higher Mortality Rate in Moderate-to-Severe Thoracoabdominal Injury Patients with Admission Hyperglycemia Than Nondiabetic Normoglycemic Patients 1, 2, 1 1 1 Wei-Ti Su y, Shao-Chun Wu y , Sheng-En Chou , Chun-Ying Huang , Shiun-Yuan Hsu , 1, , 3, , Hang-Tsung Liu z * and Ching-Hua Hsieh z * 1 Department of Trauma Surgery, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University and College of Medicine, Kaohsiung 83301, Taiwan; [email protected] (W.-T.S.); [email protected] (S.-E.C.); [email protected] (C.-Y.H.); [email protected] (S.-Y.H.) 2 Department of Anesthesiology, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University and College of Medicine, Kaohsiung 83301, Taiwan; [email protected] 3 Department of Plastic Surgery, Kaohsiung Chang Gung Memorial Hospital, Chang Gung University and College of Medicine, Kaohsiung 83301, Taiwan * Correspondence: [email protected] (H.-T.L.); [email protected] (C.-H.H.) These authors contribute equally to this paper as the first author. y These authors contribute equally to this paper as the corresponding author. z Received: 21 August 2019; Accepted: 23 September 2019; Published: 25 September 2019 Abstract: Background: Hyperglycemia at admission is associated with an increase in worse outcomes in trauma patients. However, admission hyperglycemia is not only due to diabetic hyperglycemia (DH), but also stress-induced hyperglycemia (SIH). This study was designed to evaluate the mortality rates between adult moderate-to-severe thoracoabdominal injury patients with admission hyperglycemia as DH or SIH and in patients with nondiabetic normoglycemia (NDN) at a level 1 trauma center. -

Supplementary Material
Supplementary material Table S1. Search strategy performed on the following databases: PubMed, Embase, the Cochrane Central Register of Controlled Trials (CENTRAL). 1. Randomi*ed study OR random allocation OR Randomi*ed controlled trial OR Random* Control* trial OR RCT Epidemiological study 2. sodium glucose cotransporter 2 OR sodium glucose cotransporter 2 inhibitor* OR sglt2 inhibitor* OR empagliflozin OR dapagliflozin OR canagliflozin OR ipragliflozin OR tofogliflozin OR ertugliflozin OR sotagliflozin OR sergliflozin OR remogliflozin 3. 1 AND 2 1 Table S2. Safety outcomes of empagliflozin and linagliptin combination therapy compared with empagliflozin or linagliptin monotherapy in treatment naïve type 2 diabetes patients Safety outcome Comparator 1 Comparator 2 I2 RR [95% CI] Number of events Number of events / / total subjects total subjects i. Empagliflozin + linagliptin vs empagliflozin monotherapy Empagliflozin + Empagliflozin linagliptin monotherapy ≥ 1 AE(s) 202/272 203/270 77% 0.99 [0.81, 1.21] ≥ 1 drug-related 37/272 38/270 0% 0.97 [0.64, 1.47] AE(s) ≥ 1 serious AE(s) 13/272 19/270 0% 0.68 [0.34, 1.35] Hypoglycaemia* 0/272 5/270 0% 0.18 [0.02, 1.56] UTI 32/272 25/270 29% 1.28 [0.70, 2.35] Events suggestive 12/272 13/270 9% 0.92 [0.40, 2.09] of genital infection i. Empagliflozin + linagliptin vs linagliptin monotherapy Empagliflozin + Linagliptin linagliptin monotherapy ≥ 1 AE(s) 202/272 97/135 0% 1.03 [0.91, 1.17] ≥ 1 drug-related 37/272 17/135 0% 1.08 [0.63, 1.84] AE(s) ≥ 1 serious AE(s) 13/272 2/135 0% 3.22 [0.74, 14.07] Hypoglycaemia* 0/272 1/135 NA 0.17 [0.01, 4.07] UTI 32/272 12/135 0% 1.32 [0.70, 2.49] Events suggestive 12/272 4/135 0% 1.45 [0.47, 4.47] of genital infection RR, relative risk; AE, adverse event; UTI, urinary tract infection. -

Prevention of Stress Hyperglycemia with the Use of DPP-4 Inhibitors in Non-Diabetic Patients Undergoing Non-Cardiac Surgery, a Pilot Study (SITA-SURGERY PILOT TRIAL)
Title: Prevention of stress hyperglycemia with the use of DPP-4 inhibitors in non-diabetic patients undergoing non-cardiac surgery, a Pilot Study (SITA-SURGERY PILOT TRIAL). Principal Investigator: Maya Fayfman, M.D. Instructor of Medicine Department of Medicine/Endocrinology Emory University School of Medicine Co-Investigators: Department of Medicine: Guillermo Umpierrez, MD, Priyathama Vellanki, MD, David Reyes, MD, Georgia Davis, MD, Saumeth Cardona, David Chachkhiani, Clementina Ramos Garrido, David Alfa, and Maria Urrutia Department of Surgery: Sheryl Gabram-Mendola and MD, Mara Schenker, MD Department of Anesthesiology Elizabeth Duggan, MD, Jay Sanford MD and Joanna Schindler MD School of Public Health Limin Peng, PhD Investigator-Sponsor: Guillermo Umpierrez, MD. Division of Endocrinology, Department of Medicine ABSTRACT Approximately 51.4 million surgical procedures are performed in the United States each year.1 Over 40% of patients both with and without diabetes (DM) develop stress hyperglycemia (defined as a BG >140 mg/dl) after general surgery.2,3 Compared to patients without DM, those with DM have higher rates of complications that include wound infections,4,5 acute renal failure,6 longer hospital stay,7,8 and perioperative mortality.8,9 However, non-DM patients with stress hyperglycemia have poor surgical outcome after cardiac surgery with even higher rates of complications and mortality compared to those with DM.10,11 Few observational studies looking at non- cardiac patients have found that stress hyperglycemia is associated -

Assessment of the Pharmacokinetic Interaction Between the Novel DPP-4 Inhibitor Linagliptin Andasulfonylurea,Glyburide,Inhealthysubjects
Drug Metab. Pharmacokinet. 26 (2): 123129 (2011). Copyright © 2011 by the Japanese Society for the Study of Xenobiotics (JSSX) Regular Article Assessment of the Pharmacokinetic Interaction between the Novel DPP-4 Inhibitor Linagliptin andaSulfonylurea,Glyburide,inHealthySubjects Ulrike GRAEFE-MODY1,*, Peter ROSE2,ArneRING2,KerstinZANDER2, Mario IOVINO2 and Hans-Juergen WOERLE1 1Boehringer Ingelheim Pharma GmbH & Co. KG, Ingelheim, Germany 2Boehringer Ingelheim Pharma GmbH & Co. KG, Biberach, Germany Full text of this paper is available at http://www.jstage.jst.go.jp/browse/dmpk Summary: The aim of this study was to investigate the effect of the dipeptidyl peptidase-4 inhibitor linagliptin on the pharmacokinetics of glyburide (a CYP2C9 and CYP3A4 substrate) and vice versa.This randomized, open-label, three-period, two-way crossover study examined the effects of co-administration of multiple oral doses of linagliptin (5 mg/day © 6 days) and single doses of glyburide (1.75 mg/day © 1day)on the relative bioavailability of either compound in healthy subjects (n = 20, age 1855 years). Coadmin- istration of glyburide did not alter the steady-state pharmacokinetics of linagliptin. Geometric mean ratios (GMRs) [90% CI] for (linagliptin + glyburide)/linagliptin AUC¸,ss and Cmax,ss were 101.7% [97.7105.8%] and 100.8% [89.0114.3%], respectively. For glyburide, there was a slight reduction in exposure of ³14% when coadministered with linagliptin (GMRs [90% CI] for (glyburide + linagliptin)/glyburide AUC0¨ and Cmax were 85.7% [79.892.1%] and 86.2% [79.693.3%], respectively). However, this was not seen as clinically relevant due to the absence of a reliable doseresponse relationship and the known large pharmacokinetic interindividual variability of glyburide. -

Combination Use of Insulin and Incretins in Type 2 Diabetes
Canadian Agency for Agence canadienne Drugs and Technologies des médicaments et des in Health technologies de la santé CADTH Optimal Use Report Volume 3, Issue 1C Combination Use of Insulin and July 2013 Incretins in Type 2 Diabetes Supporting Informed Decisions This report is prepared by the Canadian Agency for Drugs and Technologies in Health (CADTH). The report contains a comprehensive review of the existing public literature, studies, materials, and other information and documentation (collectively the “source documentation”) available to CADTH at the time of report preparation. The information in this report is intended to help Canadian health care decision-makers, health care professionals, health systems leaders, and policy-makers make well-informed decisions and thereby improve the quality of health care services. The information in this report should not be used as a substitute for the application of clinical judgment in respect of the care of a particular patient or other professional judgment in any decision-making process, nor is it intended to replace professional medical advice. While CADTH has taken care in the preparation of this document to ensure that its contents are accurate, complete, and up to date as of the date of publication, CADTH does not make any guarantee to that effect. CADTH is not responsible for the quality, currency, propriety, accuracy, or reasonableness of any statements, information, or conclusions contained in the source documentation. CADTH is not responsible for any errors or omissions or injury, loss, or damage arising from or relating to the use (or misuse) of any information, statements, or conclusions contained in or implied by the information in this document or in any of the source documentation. -
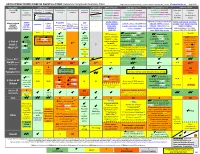
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Color Outcomes Comparison Summary Table
ANTI-HYPERGLYCEMIC DIABETES AGENTS in T2DM: Outcomes Comparison Summary Table L Regier BSP BA, M LeBras PharmD, T Trischuk PharmD, J Bareham BSP, L Lu BSP © www.RxFiles.ca Aug 2021 Drug Class Sulfonylureas TZDs Meglitinides DPP4 Inhibitors GLP1 Agonists *** SGLT2 Inhibitors *** Insulin in T2DM Generic Metformin Gliclazide Glyburide Pioglitazone Rosiglitazone Acarbose Repaglinide Saxagliptin ONGLYZA Liraglutide VICTOZA Empagliflozin JARDIANCE Intensity: Intensity: BRAND (MF) DIAMICRON DIABETA ACTOS, g AVANDIA GLUCOBAY GLUCONORM Sitagliptin JANUVIA Exenatide BYETTA, BYDUREON Canagliflozin INVOKANA Less More GLUCOPHAGE Dulaglutide TRULICITY Dapagliflozin FORXIGA, FARXIGA Alogliptin NESINA (e.g. NPH (Multiple daily GLUCOTROL D/C STEGLATRO Glipizide Nateglinide Semaglutide OZEMPIC, RYBELSUS (PO) Ertugliflozin Linagliptin TRAJENTA HS + MF) doses) STARLIX D/C SPREAD-DIMCAD] Lixisenatide ADLYXINE; ALBIGLUTIDE D/C SAVOR-TIMI 53, EMPA-REG, CANVAS, CREDENCE, T2DM: UKPDS-33,80; ADVANCE, Major trials to UKPDS- ProACTIVE ACE 33,34,80 UKPDS- Meta-analysis. TECOS, EXAMINE LEADER, EXSCEL, FREEDOM CVO, DECLARE, VERTIS-CV (2020), ACCORD, VADT, ORIGIN, DEVOTE support ADVANCE (Prevention (ADOPT; 33,80 Ferwana M. Meta- RECORD interim, PROLOGUE, REWIND, SUSTAIN-6, PIONEER-6, DAPA-HF, DAPA-CKD (2020), T1DM: DCCT/EDIC findings/ analysis 2013. trial: Stop- - some use in (ADOPT) ADOPT, DREAM CARMELINA, EMPEROR-Reduced & -Preserved (Also Boussageon et al. Meta- Outcomes* ADVANCE) SR-Liao 2017; IRIS NIDDM) ELIXA, HARMONY CAROLINA (2020), EMPA-Kidney (2022) analysis. -

The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances The
International Journal of Molecular Sciences Article The Dipeptidyl Peptidase-4 Inhibitor Linagliptin Directly Enhances the Contractile Recovery of Mouse Hearts at a Concentration Equivalent to that Achieved with Standard Dosing in Humans 1, 1, 1 1 Sri Nagarjun Batchu y, Veera Ganesh Yerra y , Youan Liu , Suzanne L. Advani , Thomas Klein 2 and Andrew Advani 1,* 1 Keenan Research Center for Biomedical Science and Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Toronto, ON M5B 1T8, Canada; [email protected] (S.N.B.); [email protected] (V.G.Y.); [email protected] (Y.L.); [email protected] (S.L.A.) 2 Department of Cardiometabolic Diseases Research, Boehringer Ingelheim Pharma GmbH & Co. KG, 88397 Biberach, Germany; [email protected] * Correspondence: [email protected]; Tel.: +1-416-864-6060 (ext. 8413) These authors contributed equally to this work. y Received: 14 June 2020; Accepted: 9 August 2020; Published: 11 August 2020 Abstract: Despite a similar mechanism of action underlying their glucose-lowering effects in type 2 diabetes, dipeptidyl peptidase-4 (DPP-4) inhibitors have diverse molecular structures, raising the prospect of agent-specific, glucose-independent actions. To explore the issue of possible DPP-4 inhibitor cardiac heterogeneity, we perfused different DPP-4 inhibitors to beating mouse hearts ex vivo, at concentrations equivalent to peak plasma levels achieved in humans with standard dosing. We studied male and female mice, young non-diabetic mice, and aged diabetic high fat diet-fed mice and observed that linagliptin enhanced recovery after ischemia-reperfusion, whereas sitagliptin, alogliptin, and saxagliptin did not. -

The Association of Admission Blood Glucose Level with the Clinical Picture and Prognosis in Cardiogenic Shock – Results from the Cardshock Study☆
International Journal of Cardiology 226 (2017) 48–52 Contents lists available at ScienceDirect International Journal of Cardiology journal homepage: www.elsevier.com/locate/ijcard The association of admission blood glucose level with the clinical picture and prognosis in cardiogenic shock – Results from the CardShock Study☆ Anu Kataja a,⁎,1, Tuukka Tarvasmäki a,1,JohanLassusb,1, Jose Cardoso c,1, Alexandre Mebazaa d,1,LarsKøbere,1, Alessandro Sionis f,1, Jindrich Spinar g,1, Valentina Carubelli h,1, Marek Banaszewski i,1, Rossella Marino j,1, John Parissis k,1, Markku S. Nieminen b,1, Veli-Pekka Harjola a,1 a Emergency Medicine, University of Helsinki, Department of Emergency Medicine and Services, Helsinki University Hospital, Helsinki, Finland b Cardiology, University of Helsinki, Heart and Lung Center, Helsinki University Hospital, Helsinki, Finland c CINTESIS - Center for Health Technology and Services Research, Department of Cardiology, Faculty of Medicine, University of Porto, São João Medical Center, Porto, Portugal d INSERM U942, Hopital Lariboisiere, APHP and University Paris Diderot, Paris, France e Rigshospitalet, Copenhagen University Hospital, Division of Heart Failure, Pulmonary Hypertension and Heart Transplantation, Copenhagen, Denmark f Intensive Cardiac Care Unit, Cardiology Department, Hospital de la Santa Creu i Sant Pau, Biomedical Research Institute IIB-Sant Pau, Universitat de Barcelona, Barcelona, Spain g Internal Cardiology Department, University Hospital Brno and Masaryk University, Brno, Czech republic h Division -

Post-Operative Stress Hyperglycemia Is a Predictor of Mortality in Liver
Giráldez et al. Diabetol Metab Syndr (2018) 10:35 https://doi.org/10.1186/s13098-018-0334-5 Diabetology & Metabolic Syndrome RESEARCH Open Access Post‑operative stress hyperglycemia is a predictor of mortality in liver transplantation Elena Giráldez1* , Evaristo Varo2, Ipek Guler3, Carmen Cadarso‑Suarez3, Santiago Tomé2, Patricia Barral1, Antonio Garrote1 and Francisco Gude4 Abstract Background: A signifcant association is known between increased glycaemic variability and mortality in critical patients. To ascertain whether glycaemic profles during the frst week after liver transplantation might be associated with long-term mortality in these patients, by analysing whether diabetic status modifed this relationship. Method: Observational long-term survival study includes 642 subjects undergoing liver transplantation from July 1994 to July 2011. Glucose profles, units of insulin and all variables with infuence on mortality are analysed using joint modelling techniques. Results: Patients registered a survival rate of 85% at 1 year and 65% at 10 years, without diferences in mortal‑ ity between patients with and without diabetes. In glucose profles, however, diferences were observed between patients with and without diabetes: patients with diabetes registered lower baseline glucose values, which gradually rose until reaching a peak on days 2–3 and then subsequently declined, diabetic subjects started from higher values which gradually decreased across the frst week. Patients with diabetes showed an association between mortality and age, Model for End-Stage Liver Disease score (MELD) score and hepatitis C virus; among non-diabetic patients, mortal‑ ity was associated with age, body mass index, malignant aetiology, red blood cell requirements and parenteral nutri‑ tion. Glucose profles were observed to be statistically associated with mortality among patients without diabetes (P 0.022) but not among patients who presented with diabetes prior to transplantation (P 0.689). -

Overnight Caloric Restriction Prior to Cardiac Arrest and Resuscitation Leads to Improved Survival and Neurological Outcome in a Rodent Model
bioRxiv preprint doi: https://doi.org/10.1101/786871; this version posted September 30, 2019. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-NC-ND 4.0 International license. Overnight caloric restriction prior to cardiac arrest and resuscitation leads to improved survival and neurological outcome in a rodent model Matine Azadian1, Guilian Tian1, Afsheen Bazrafkan1, Niki Maki1, Masih Rafi1, Monica Desai1, Ieeshiah Otarola1, Shuhab Zaher1, Ashar Khan1, Yusuf Suri1, Minwei Wang1, Oswald Steward2, Yama Akbari1, 3, 4 1Department of Neurology, School of Medicine, University of California, Irvine, CA, USA 2Reeve-Irvine Research Center, Department of Anatomy and Neurobiology, School of Medicine, University of California, Irvine, CA, USA 3Beckman Laser Institute, University of California, Irvine, CA, USA 4Department of Neurological Surgery, School of Medicine, University of California, Irvine, CA, USA Abstract While interest toward caloric restriction (CR) in various models of brain injury has increased in recent decades, studies have predominantly focused on the benefits of chronic or intermittent CR. The effects of ultra-short, including overnight, CR on acute ischemic brain injury, however, are not well studied. Here, we show that overnight caloric restriction (75% over 14 h) prior to asphyxial cardiac arrest and resuscitation (CA) improves survival and neurological recovery, including complete prevention of neurodegeneration in multiple regions of the brain. We also show that overnight CR normalizes stress-induced hyperglycemia, while significantly decreasing insulin and glucagon production and increasing corticosterone and ketone body production. -

Linagliptin (Tradjenta) for the Treatment of Diabetes Mellitus KAREN WHALEN, Pharmd, BCPS, CDE, and KAREN R
STEPS New Drug Reviews Linagliptin (Tradjenta) for the Treatment of Diabetes Mellitus KAREN WHALEN, PharmD, BCPS, CDE, and KAREN R. SANDO, PharmD, CDE University of Florida College of Pharmacy, Gainesville, Florida STEPS new drug reviews Linagliptin (Tradjenta) is a dipeptidyl-peptidase-4 (DPP-4) inhibitor labeled for the treat- cover Safety, Tolerability, ment of type 2 diabetes mellitus. Similar to sitagliptin (Januvia) and saxagliptin (Onglyza), Effectiveness, Price, and Simplicity. Each indepen- linagliptin delays the breakdown of endogenous incretin hormones such as glucagon-like dent review is provided peptide 1 and glucose-dependent insulinotropic polypeptide. These hormones, when secreted by authors who have no in response to food intake, stimulate postmeal insulin secretion, inhibit glucagon release, financial association with improve satiety, and slow gastric emptying.1,2 Linagliptin can be used alone or in combination the drug manufacturer. with metformin (Glucophage), sulfonylureas, pioglitazone (Actos), or insulin. The series coordinator for AFP is Allen F. Shaugh- nessy, PharmD, Tufts Drug Dosage Dose form Cost* University Family Medicine Residency Program at Linagliptin (Tradjenta) 5 mg daily 5-mg tablet $254 for 30 tablets Cambridge Health Alli- ance, Malden, Mass. *—Estimated retail price of one month’s treatment based on information obtained at http://www.goodrx.com A collection of STEPS pub- (accessed October 1, 2012). lished in AFP is available at http://www.aafp.org/ afp/steps. SAFETY control should be used in patients receiving Few severe adverse effects have been associ- strong inducers of cytochrome P450 3A4 ated with linagliptin. When used alone or or P-glycoprotein, such as rifampin. Lina- with metformin or pioglitazone, linagliptin gliptin is a U.S. -

Diabetes: Putting It All Together to Design a High Value Diabetes Regimen for Your Patient
Diabetes: Putting it all together to design a high value diabetes regimen for your patient Cecilia C. Low Wang, MD Professor of Medicine Division of Endocrinology, Metabolism and Diabetes University of Colorado School of Medicine [email protected] Disclosures • None Objectives • Describe the benefits, side effects/risks, and costs of the newer diabetes medications • Discuss the value of the newer diabetes medications • Make high-value patient-centered decisions when intensifying diabetes therapy Worsening HbA1c • Ms L is a 48 year old woman here for routine f/u • She has Type 2 diabetes (x 5 years; no complications), obesity (BMI 41), chronic knee pain from osteoarthritis, and is postmenopausal s/p TAH 6 yr ago for uterine leiomyomas • You last saw her 6 months ago. At that time, her A1c was 6.4% on metformin 1000 mg BID • You see that her A1c is now 8.5%. • What other information do you need? • How would you intensify her diabetes treatment? “New-onset” diabetes • Mr. B is a 53 year old M hospitalized for NSTEMI and underwent 3v CABG • He had HTN but no other medical history and was on no medications prior to admission • Admission point-of-care (POC) glucose: 263 mg/dL • HbA1c: 11.5% • He agrees that he needs to be on insulin upon discharge • Are there any non-insulin medications that should be considered for him? • How would you design his regimen? ADVANCE: Diabetes complications and A1c relationship CVA CV death • Linear relationship (no threshold) for eye complications • J-curve: Increasing DKD Retinopathy risk with A1c <6.5% for CV and renal complications 6 Zoungas, et al.