Progesterone- Releasing Vaginal Ring 8 Key Points for Providers and Clients
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

F.8 Ethinylestradiol-Etonogestrel.Pdf
General Items 1. Summary statement of the proposal for inclusion, change or deletion. Here within, please find the evidence to support the inclusion Ethinylestradiol/Etonogestrel Vaginal Ring in the World Health Organization’s Essential Medicines List (EML). Unintended pregnancy is regarded as a serious public health issue both in developed and developing countries and has received growing research and policy attention during last few decades (1). It is a major global concern due to its association with adverse physical, mental, social and economic outcomes. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (2). Even though the incidence of unintended pregnancy has declined globally in the past decade, the rate of unintended pregnancy remains high, particularly in developing regions. (3) Regarding the use of contraceptive vaginal rings, updated bibliography (4,5,6) states that contraceptive vaginal rings (CVR) offer an effective contraceptive option, expanding the available choices of hormonal contraception. Ethinylestradiol/Etonogestrel Vaginal Ring is a non-biodegradable, flexible, transparent with an outer diameter of 54 mm and a cross-sectional diameter of 4 mm. It contains 11.7 mg etonogestrel and 2.7 mg ethinyl estradiol. When placed in the vagina, each ring releases on average 0.120 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol over a three-week period of use. Ethinylestradiol/Etonogestrel Vaginal Ring is intended for women of fertile age. The safety and efficacy have been established in women aged 18 to 40 years. The main advantages of CVRs are their effectiveness (similar or slightly better than the pill), ease of use without the need of remembering a daily routine, user ability to control initiation and discontinuation, nearly constant release rate allowing for lower doses, greater bioavailability and good cycle control with the combined ring, in comparison with oral contraceptives. -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
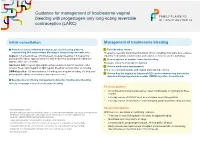
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer. -

Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
HORMONAL INTRAUTERINE DEVICES (IUDs) – (Mirena and Kyleena) What are the hormonal intrauterine devices (IUDs)? The hormonal IUDs are small ‘T- shaped’ plastic devices that are inserted into the uterus (womb). The hormonal IUDs contains progestogen. This is a synthetic version of the hormone progesterone made naturally by the ovaries. The hormonal IUDs have a coating (membrane) that controls the slow release of progestogen into the uterus. There are two different hormonal IUDs available in Australia. They are sold as Mirena and Kyleena. How effective are the hormonal IUDs? The hormonal IUDs are more than 99% effective at preventing pregnancy and can last for up to 5 years. They can be used for contraception until 55 years of age if inserted when you are 45 years of age or older. How does the hormonal IUD work? IUDs affect the way sperm move and survive in the uterus (womb), stopping sperm from meeting and fertilising an egg. IUDs can also change the lining of the uterus, making it difficult for a fertilised egg to stick to the lining to start a pregnancy. The hormonal IUDs also work by thickening the fluid around the cervix (opening to the uterus/womb). This helps to prevent sperm from entering. Sometimes the hormonal IUDs can also stop the ovaries from releasing an egg. What are differences between Mirena and Kyleena hormonal IUDs? Both Mirena and Kyleena are very effective methods of contraception that last for up to 5 years. Mirena is 99.9% effective and Kyleena is 99.7% effective. Mirena may be used until 55 years of age if inserted when you are 45 years of age or older, whereas Kyleena needs to be replaced every 5 years for all ages. -

Nuvaring (Vaginal Ring) Brown Health Services Patient Education Series
NuvaRing (Vaginal Ring) Brown Health Services Patient Education Series You may choose any position that is comfortable for What is the NuvaRing? you: lying down, squatting, or standing with one leg The NuvaRing is a flexible, combined contraceptive propped on a chair. Hold the ring between your vaginal ring, used to prevent pregnancy. NuvaRing thumb and index finger and press the opposite sides contains a combination of progestin and estrogen, of the ring together. Gently push the folded ring two kinds of hormones. The ring is inserted in the into your vagina. vagina and left there for 3 weeks. You then remove it for a 1 week free period. After the ring is inserted, The exact position of the NuvaRing in the vagina is it releases a continuous low dose of hormones into not important for it to work. Most users do not feel your body. The Nuva Ring is 99.7% effective against the ring once it is in place. If you feel discomfort, pregnancy with perfect use, and 93% effective with the NuvaRing is probably not inserted far enough typical use. into your vagina. Just use your finger to gently push What’s in the NuvaRing? NuvaRing further into your vagina. There is no danger of Nuvaring being pushed too far up in the NuvaRing contains two hormones: estrogen and vagina or getting lost. Once inserted keep the progesterone. These hormones are synthetic Nuvaring in place for 3 weeks in a row. You do not versions of naturally occurring hormones. The ring need to remove the ring during sex. -

Laaketilasto07 2.Pdf
Keskeisiä lukuja lääkkeiden myynnistä ja lääkekorvauksista vuonna 2007 Muutos vuodesta 2006 Lääkkeiden kokonaismyynti 2 500 milj. € 5,9 % avohoidon reseptilääkkeiden myynti (verollisin vähittäismyyntihinnoin) 1 817 milj. € 4,2 % avohoidon itsehoitolääkkeiden myynti (verollisin vähittäismyyntihinnoin) 275 milj. € 15,5 % sairaalamyynti (tukkuohjehinnoin) 408 milj. € 7,5 % Lääkkeistä maksetut korvaukset 1 142 milj. € 3,8 % peruskorvaukset 369 milj. € 0,6 % erityiskorvaukset 662 milj. € 6,8 % lisäkorvaukset 111 milj. € -2,3 % Key figures for medicine sales and their reimbursement in 2007 Change from 2006 Total sales of pharmaceuticals EUR 2,500 million 5.9% prescription medicines in outpatient care (at pharmacy prices with VAT) EUR 1,817 million 4.2% OTC medicines in outpatient care (at pharmacy prices with VAT) EUR 275 million 15.5% sales to hospitals (at wholesale prices) EUR 408 million 7.5% Reimbursement of medicine costs EUR 1,142 million 3.8% Basic Refunds EUR 369 million 0.6% Special Refunds EUR 662 million 6.8% Additional Refunds EUR 111 million -2.3% SUOMEN LÄÄKETILASTO FINNISH STATISTICS ON MEDICINES 2007 Lääkelaitos ja Kansaneläkelaitos National Agency for Medicines and Social Insurance Institution Helsinki 2008 LÄÄKELAITOS KANSANELÄKELAITOS NATIONAL AGENCY SOCIAL INSURANCE FOR MEDICINES INSTITUTION Lääketurvaosasto Tutkimusosasto Department of Safety Research Department and Drug Information Mannerheimintie 103b Nordenskiöldinkatu 12 P.O. Box 55 P.O. Box 450 FI-00301 Helsinki FI-00101 Helsinki Finland Finland Puh. (09) 473 341 Puh. 020 634 11 Tel. +358 9 473 341 Tel. +358 20 634 11 Telekopio (09) 473 34297 Telekopio 020 634 1700 Fax +358 9 473 34297 Fax +358 20 634 1700 ISSN 0786-2180 Kansi / Cover: Kari Piippo Edita Prima Oy Helsinki 2008 SISÄLLYS Kuvaluettelo ..................................................................................................................... -

Etonogestrel/Ethinyl Estradiol Slow Release Vaginal Ring (11.4 Mg/2.6 Mg) to Deliver 120 Mcg Etonogestrel/15 Mcg Ethinyl Estradiol Per Day
PRODUCT MONOGRAPH PrNUVARING® etonogestrel/ethinyl estradiol slow release vaginal ring (11.4 mg/2.6 mg) to deliver 120 mcg etonogestrel/15 mcg ethinyl estradiol per day Contraceptive Vaginal Ring FOR VAGINAL USE ONLY Organon Canada Inc. Date of Revision: 16766 route Transcanadienne Kirkland, Quebec March 25, 2021 www.organon.ca Submission Control No: 249249 NUVARING® Product monograph Page 1 of 59 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ......................................................... 3 SUMMARY PRODUCT INFORMATION ........................................................................ 3 INDICATIONS AND CLINICAL USE ............................................................................. 3 CONTRAINDICATIONS ................................................................................................... 3 WARNINGS AND PRECAUTIONS ................................................................................. 4 ADVERSE REACTIONS ................................................................................................. 13 DRUG INTERACTIONS ................................................................................................. 19 DOSAGE AND ADMINISTRATION ............................................................................. 27 OVERDOSAGE ................................................................................................................ 30 ACTION AND CLINICAL PHARMACOLOGY ............................................................ 30 STORAGE AND STABILITY ........................................................................................ -

Contraception in Adolescents – Regulatory Considerations”
“Contraception in adolescents – regulatory considerations” Wissenschaftliche Prüfungsarbeit zur Erlangung des Titels „Master of Drug Regulatory Affairs“ der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Dr. Julian Paesler aus Münster Bonn 2016 Betreuerin und 1. Referentin: Frau Dr. Ingrid Klingmann Zweiter Referent: Herr Prof. Dr. Niels Eckstein Acknowledgements I would like to express my sincere gratitude to Dr. Ingrid Klingmann for her friendly willingness to function as my “supervising tutor” and for the support and the motivating feedback she gave me during the preparation of this master thesis. Her comments and constructive suggestions were very helpful to me. Besides Dr. Ingrid Klingmann, I would like to thank Prof. Dr. Niels Eckstein for his support and the willingness to function as my “secondary tutor”. Special thanks are also due to my mother, who was willing to proofread this master thesis. I am really thankful for all the support she gave - and still gives – to me, which is way more than what could ever be mentioned here. Table of Contents Table of Contents List of Figures .......................................................................................................................... I List of Tables ......................................................................................................................... III List of Abbreviations .............................................................................................................. -

Teen Sexuality and Cystic Fibrosis
Cystic Fibrosis Canada Teen Sexuality and Cystic Fibrosis As a teenager, you probably have many questions about your sexuality and about how cystic fibrosis (CF) might affect your sexual health. Like many teenagers, these kinds of questions are common: “Am I changing more slowly than my friends?” “When will I have my first period?” “When will I start to fill out?” “Why am I still not very tall?” “Why don’t I have signs of a beard yet?” “Why hasn’t my voice changed?” Sometimes, you might feel that you are not developing as quickly as your friends. Try to remember that people grow at their own pace. Look around and you will find others “…puberty begins about your age who do not have cystic fibrosis who 18 months later than the have not yet started to average for individuals develop. The fact remains that puberty with cystic fibrosis.” begins about 18 months later than the average for individuals with cystic fibrosis. It is not unusual for development to start as late as 15 to 17 years of age for girls, and even later for boys. You can help your development by making sure you are getting enough calories and nutrients — this may require eating a lot more than your friends who do not have cystic fibrosis. When should I tell Only you can decide when to tell someone that you have cystic fibrosis; my partner that I there is no right or wrong time. You may not be comfortable confiding in have cystic fibrosis? someone right away, but as the relationship develops, so will opportunities to share your situation. -

4GIRLS Sexual Development Can Start Around the Age of Nine to 13 with Girls Develop at Different Rates
A guide to the female body 4GIRLS Sexual development can start around the age of nine to 13 with Girls develop at different rates. Some girls may have their first period pubic and underarm hair and breasts starting to grow. when they're eight years old, others may be 18. All these changes – known as puberty – take place over several years. I never My boyfriend Is it I think I've got a My period's Can my doctor know when my says I'm frigid wrong I fancy vaginal discharge. period's due because I don't to touch late. What tell my parents should I girls Have I caught want to have myself? something? I'm having sex do? sex? Why do My I feel so I don't want moody? Can you get a Why is one My thighs periods sexually transmitted of my breasts to have sex. are huge. Should I are really I've got infection if you've only smaller than Is something go on a diet? painful C-cup breasts Why had sex once? the other? wrong with am I so me? but tiny hairy? nipples 2 3 Facts about breasts FACTS ABOUT GEnITALS are as GEnitals Like BREASTS get a lot of individual as people's faces – this! attention in our society and many they all look very different. girls worry that theirs don’t measure Take a look at your vulva up to the images around them. (external genital organs) with a mirror … Breasts and nipples tingle or itch while they're developing, but this will stop once they've grown. -

Vaginal Contraceptive Ring (Nuvaring)
University of California, Santa Cruz Student Health Services Vaginal Contraceptive Ring (NuvaRing) How do I use the vaginal ring? 1. Your unused rings may be kept at room temperature for up to 4 months. 2. When you are ready to use the ring, wash your hands thoroughly and remove the ring from its package. 3. Press the edges of the ring together and slide the ring into your vagina. You can do this sitting, standing, lying down, or with one leg up on a stool. There is no special place or position for the ring: once it is in the vagina it will settle into a comfortable position. Very few people report that they can feel the ring once it is in the vagina. 4. Use a back-up method of contraception like condoms for a week after you put your first ring in. After the first ring, you will not need a back-up method when you start a new ring each month. 5. Leave the ring in the vagina for 3 weeks. Some people put a reminder in their calendars, or in their phones to help them remember to take the ring out. Research shows that the ring is still effective if left in for 4 weeks. Some people choose to leave it in for 4 weeks because it is more economical for them. 6. After 3 to 4 weeks, remove the ring, put it in the foil packet or a baggie and discard it in the trash. 7. Leave the ring out for one week (7 days). -

Etonogestrel/Ethinyl Estradiol Vaginal Ring)
Patient Information NuvaRing® (NEW-vah-ring) (etonogestrel/ethinyl estradiol vaginal ring) What is the most important information I should know about NuvaRing? Do not use NuvaRing if you smoke cigarettes and are over 35 years old. Smoking increases your risk of serious cardiovascular side effects (heart and blood vessel problems) from combination hormonal contraceptives (CHCs), including death from heart attack, blood clots or stroke. This risk increases with age and the number of cigarettes you smoke. Hormonal birth control methods help to lower the chances of becoming pregnant. They do not protect against HIV infection (AIDS) and other sexually transmitted infections. What is NuvaRing? NuvaRing (NEW-vah-ring) is a flexible birth control vaginal ring used to prevent pregnancy. NuvaRing contains a combination of a progestin and estrogen, 2 kinds of female hormones. Birth control methods that contain both an estrogen and a progestin are called combination hormonal contraceptives (CHCs). How well does NuvaRing work? Your chance of getting pregnant depends on how well you follow the directions for using NuvaRing. The better you follow the directions, the less chance you have of getting pregnant. Based on the results of a US clinical study, approximately 1 to 3 women out of 100 women may get pregnant during the first year they use NuvaRing. The following chart shows the chance of getting pregnant for women who use different methods of birth control. Each box on the chart contains a list of birth control methods that are similar in effectiveness. The most effective methods are at the top of the chart. The box on the bottom of the chart shows the chance of getting pregnant for women who do not use birth control and are trying to get pregnant.