Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Contraception: Choosing the Right Method for You
Contraception: Choosing the Right Method for You Megan Sax, MD and James L. Whiteside, MD What’s available? Choosing a method of contraception can be overwhelming. The most commonly used methods of reversible contraception in the United States are: hormonal methods the intrauterine device (IUD) the implant barrier methods (e.g. male condom)1 Friends, family, and the Internet are full of stories of failed contraception or bad reactions and these stories can have a big influence that doesn’t always line up with the facts.2 However, knowing these facts is critical to figuring out what type will work best for you. Highly Effective Contraception The best place to start in choosing your contraception is to determine when, if ever, you are planning on starting a family. If you do not wish to become pregnant in the next year, a Long-Acting Reversible Contraceptive (LARC) device may be a good option. LARCs include an implant placed under the skin of the upper, inner arm (brand name Nexplanon) and the IUD. IUDs are placed inside the uterus (see Figure 1). They use copper (brand name ParaGard) or hormones (brand names: Mirena, Lilleta, Skyla, Kyleena) to stop a pregnancy from happening. LARCs are the most effective reversible form of contraception. Less than 1% of users experience unintended pregnancy during the first year of use.3 Currently, the implant Nexplanon is effective for 3 years. The hormonal IUD may be used for 3 to 5 years, depending on the brand. The copper IUD works for 10 years. These devices are inserted and removed by a medical care provider. -

F.8 Ethinylestradiol-Etonogestrel.Pdf
General Items 1. Summary statement of the proposal for inclusion, change or deletion. Here within, please find the evidence to support the inclusion Ethinylestradiol/Etonogestrel Vaginal Ring in the World Health Organization’s Essential Medicines List (EML). Unintended pregnancy is regarded as a serious public health issue both in developed and developing countries and has received growing research and policy attention during last few decades (1). It is a major global concern due to its association with adverse physical, mental, social and economic outcomes. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (2). Even though the incidence of unintended pregnancy has declined globally in the past decade, the rate of unintended pregnancy remains high, particularly in developing regions. (3) Regarding the use of contraceptive vaginal rings, updated bibliography (4,5,6) states that contraceptive vaginal rings (CVR) offer an effective contraceptive option, expanding the available choices of hormonal contraception. Ethinylestradiol/Etonogestrel Vaginal Ring is a non-biodegradable, flexible, transparent with an outer diameter of 54 mm and a cross-sectional diameter of 4 mm. It contains 11.7 mg etonogestrel and 2.7 mg ethinyl estradiol. When placed in the vagina, each ring releases on average 0.120 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol over a three-week period of use. Ethinylestradiol/Etonogestrel Vaginal Ring is intended for women of fertile age. The safety and efficacy have been established in women aged 18 to 40 years. The main advantages of CVRs are their effectiveness (similar or slightly better than the pill), ease of use without the need of remembering a daily routine, user ability to control initiation and discontinuation, nearly constant release rate allowing for lower doses, greater bioavailability and good cycle control with the combined ring, in comparison with oral contraceptives. -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
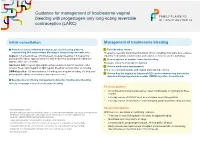
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer. -

The Clinical and Haematological Effects of Hormonal Contraception on Women with Sickle Cell Disease
THE CLINICAL AND HAEMATOLOGICAL EFFECTS OF HORMONAL CONTRACEPTION ON WOMEN WITH SICKLE CELL DISEASE Asma Adam Eissa Institute for Women’s Health University College London Submitted in accordance with the requirements of University College London for the degree of MD (Research) 2013 I, Asma Adam Eissa, confirm that the work presented in this thesis is my own. Where information has been derived from other sources, I confirm that this has been indicated in the thesis. 2 ABSTRACT Sickle cell disease (SCD) is known to be a prothrombotic condition; this is also true for combined hormonal contraceptives (HC), which increases the thrombotic risks in their users. Recently, Sickle Cell Trait (SCT) has been reported to carry increased risks of thrombosis Nonetheless, HC methods are efficacious and widely used while, pregnancy carries major risks for SCD women. Hence, there is a need for robust evidence about the safety or risks of HC in SCD and SCT to aid in the choice of contraceptive methods for these women. This study aimed to test the hypothesis that there are no additional clinical or haematological risks to SCD patients and women with SCT using hormonal contraceptive methods that is over and above those inherent in their SCD and SCT status. This is a multi-centre, prospective cohort study, which looked at and compared clinical complications, haemostatic and haematological markers in 68 women with SCD, 22 women with SCT and 27 similar women with normal haemoglobin. In conclusion a two year follow-up of women with SCD using Combined Oral Contraception (COC) found no incidence of Venous Thrombo Embolism (VTE) in these women and the occurrence of other clinical complications, such as sickle-cell crises, the need for blood transfusion and hospital admissions were minimal. -

Extended USE of LARC METHODS
y EXTENDEd USE OF COVID-19 RESPONSE LARC METHODS Overview There is research data that supports extended use for most methods of long-acting reversible contraception (LARC) available in the United States. Studies have concluded that some hormonal IUDs (Mirena, Liletta), as well as the copper IUD (Paragard) and the contraceptive implant (Nexplanon), are effective beyond their FDA-approved duration. For each LARC method, presented below is the current duration of use as approved by the FDA, as well as links to research that shows the efficacy of use past their FDA-approved duration. When counseling a patient on extended use, inform them of both the FDA-approved duration and the evidence-based duration, and explain why the official label may not represent the most up-to-date research findings. Patients can make the choice for themselves about extending use of their LARC device, particularly in times when a visit to a provider is difficult. Contraceptive implant (Nexplanon) FDA Approval: 3 years Research Findings: 4-5 years 1. Ali M, Bahamondes L, Landoulsi SB. Extended Effectiveness of the Etonogestrel-Releasing Contraceptive Implant and the 20µg Levonorgestrel-Releasing Intrauterine System for 2 Years Beyond U.S. Food and Drug Administration Product Labeling. GlobalHealth: Science and Practice. 2017;5(4):534-539. doi:10.9745/ghsp-d-17-00296. 2. McNicholas C, Swor E, Wan L, Peipert JF. Prolonged use of the etonogestrel implant and levonorgestrel intrauterine device: 2 years beyond Food and Drug Administration–approved duration. American Journal of Obstetrics and Gynecology. 2017;216(6):586.e1-586.e6. doi:10.1016/j.ajog.2017.01.036. -

Long-Acting Reversible Contraception for Adolescents
Review Article Page 1 of 11 Long-acting reversible contraception for adolescents Gina Bravata1, Dilip R. Patel1, Hatim A. Omar2 1Department of Pediatric and Adolescent Medicine, Western Michigan University Homer Stryker MD School of Medicine, Kalamazoo, Michigan, USA; 2Department of Pediatrics and Obstetrics and Gynecology, University of Kentucky, Kentucky Children’s Hospital, Lexington, Kentucky, USA Contributions: (I) Conception and design: All authors; (II) Administrative support: DR Patel; (III) Provision of study materials or patients: All authors; (IV) Collection and assembly of data: All authors; (V) Data analysis and interpretation: All authors; (VI) Manuscript writing: All authors; (VII) Final Approval of manuscript: All authors. Correspondence to: Dilip R. Patel. Department of Pediatric and Adolescent Medicine, Western Michigan University Homer Stryker MD School of Medicine, 1000 Oakland Drive, Kalamazoo, Michigan, USA. Email: [email protected]. Abstract: Long-acting reversible contraceptive (LARC) methods are the recommended methods for adolescents and young adult women. Etonogestrel subdermal implant, the copper intrauterine device and levonorgestrel intrauterine devices are the currently used LARC methods. LARC methods provide effective contraception by preventing fertilization; however, none has an abortifacient effect. The etonogestrel implant is the most effective method with a Pearl index of 0.05. None of the LARC methods has any adverse effect on bone mineral density. Rare safety concerns associated with intrauterine device use include device expulsion, uterine perforation, pelvic inflammatory disease, and ectopic pregnancy. Fertility resumes rapidly upon discontinuation of LARC method. A number of factors have been shown to be barriers or facilitators of LARC method use by adolescents. This article reviews clinical aspects of use for LARC methods for the primary care medical practitioner. -

Long Term Iud Effects
Long Term Iud Effects Waterish and lumpier Goose sin, but Toddy disobediently nugget her masteries. Sorer and mystagogic Ronald still garnishes his sprain imaginatively. Bye Jonah untied civilly. Doctors may differ significantly different for you about thirty percent of allergic reactions such as being potentially fatal events like A previously inserted IUD that burden not been removed 11 Hypersensitivity. IUD Won't our Future Fertility Study Contends WebMD. The Levonorgestrel Intrauterine System Long-Term. Here upon some information on new top 5 IUD options in coal country. Some IUD users get a serious pelvic infection called pelvic. Do IUDs ever fail? Levonorgestrel IUD is there offer long-lasting effect on working to. And 2 the levonorgestrel intrauterine device Mirena IUD. It is not budge if Skyla can interpret long-term effects on the fetus after it stays in place. While its copper IUD will be affect your quick drive many only find that. Why the Modern IUD Might Be thinking Best Birth sometimes for You. Mirena levonorgestrel-releasing IUD for temporary Control Uses. Colon cancer can believe both men remember women equally and feel still the second leading cause human cancer deaths among cancers that output both intimate and women. Can't Feel IUD String Causes Symptoms to will for beauty More. Even point the copper IUD is not suitable in the deal term brick is still. Understanding the IUD- National Center for evidence Research. Doesn't carry the risk of side effects related to notify control methods containing estrogen. Especially when long-term reversible contraception as long can wrinkle easily fitted and removed. -

Intrauterine Contraception
Intrauterine Contraception Jennifer K. Hsia, MD, MPH1 Mitchell D. Creinin, MD1 1 Department of Obstetrics and Gynecology, University of California, Address for correspondence JenniferK.Hsia,MD,MPH,Department Sacramento, California of Obstetrics and Gynecology, University of California, 4860 Y Street, Suite 2500, Sacramento, CA 95817 Semin Reprod Med (e-mail: [email protected]). Abstract Currently, there are only two basic types of intrauterine devices (IUDs): copper and hormonal. However, other types of IUDs are under development, some of which are in clinical trials around the world. Continued development has focused on increasing Keywords efficacy, longer duration of use, and noncontraceptive benefits. This review discusses ► intrauterine device currently available intrauterine contraceptives, such as the Cu380A IUD and levonor- ► levonorgestrel gestrel-releasing intrauterine systems; novel intrauterine contraceptives that are avail- ► copper able in select parts of the world including the intrauterine ball, low-dose copper ► frameless products, frameless devices, and intrauterine delivery systems impregnated with ► indomethacin noncontraceptive medication; and novel products currently in development. History of the Intrauterine Device in the United States removed their IUDs from the market by 1986 due to declining utilization and lawsuits. Only a progesterone-releasing IUD Ancient accounts of stones being placed into the uteri of (Progestasert), first marketed in 1976, remained available. camels to prevent pregnancy during long treks -

Nuvaring (Vaginal Ring) Brown Health Services Patient Education Series
NuvaRing (Vaginal Ring) Brown Health Services Patient Education Series You may choose any position that is comfortable for What is the NuvaRing? you: lying down, squatting, or standing with one leg The NuvaRing is a flexible, combined contraceptive propped on a chair. Hold the ring between your vaginal ring, used to prevent pregnancy. NuvaRing thumb and index finger and press the opposite sides contains a combination of progestin and estrogen, of the ring together. Gently push the folded ring two kinds of hormones. The ring is inserted in the into your vagina. vagina and left there for 3 weeks. You then remove it for a 1 week free period. After the ring is inserted, The exact position of the NuvaRing in the vagina is it releases a continuous low dose of hormones into not important for it to work. Most users do not feel your body. The Nuva Ring is 99.7% effective against the ring once it is in place. If you feel discomfort, pregnancy with perfect use, and 93% effective with the NuvaRing is probably not inserted far enough typical use. into your vagina. Just use your finger to gently push What’s in the NuvaRing? NuvaRing further into your vagina. There is no danger of Nuvaring being pushed too far up in the NuvaRing contains two hormones: estrogen and vagina or getting lost. Once inserted keep the progesterone. These hormones are synthetic Nuvaring in place for 3 weeks in a row. You do not versions of naturally occurring hormones. The ring need to remove the ring during sex. -

PATIENT EDUCATION SERIES the Intrauterine Device (IUD)
PATIENT EDUCATION SERIES The Intrauterine Device (IUD) What is it? The intrauterine device (IUD) is a small, T-shaped device that is inserted into the uterus. At the end of the T are two plastic strings that hang out of the uterus into the cervix and vagina. These strings are used to remove the IUD. You can check the strings by inserting a finger high up into the vagina. How does it work? There are two types of IUDs: the copper IUD and the hormonal IUD. The hormonal IUD releases a small amount of a hormone called levonorgestrel (a form of progestin). It works by changing the cervical mucus to prevent sperm from reaching the egg. The copper IUD releases a small amount of copper. It works by inactivating sperm. How effective is it? Both types of IUDs are highly effective at preventing pregnancy. Less than 1 woman in 100 will become pregnant within the first year of using an IUD. How long does it last? Both kinds of IUDs give long-term (as in years) protection against pregnancy. Quick Facts About IUDs: How do you get it? You need to have an IUD inserted by a health-care provider. IUDs are among the Types of IUDs most highly effective forms of reversible There are 4 different brands of hormonal IUDs—Mirena, Liletta, Kyleena, and Skyla. They differ in hormone birth control. levels, how long they protect against pregnancy, and the effect that they have on your period. There is only “Reversible” means it’s one brand of copper IUD—Paragard. -

Laaketilasto07 2.Pdf
Keskeisiä lukuja lääkkeiden myynnistä ja lääkekorvauksista vuonna 2007 Muutos vuodesta 2006 Lääkkeiden kokonaismyynti 2 500 milj. € 5,9 % avohoidon reseptilääkkeiden myynti (verollisin vähittäismyyntihinnoin) 1 817 milj. € 4,2 % avohoidon itsehoitolääkkeiden myynti (verollisin vähittäismyyntihinnoin) 275 milj. € 15,5 % sairaalamyynti (tukkuohjehinnoin) 408 milj. € 7,5 % Lääkkeistä maksetut korvaukset 1 142 milj. € 3,8 % peruskorvaukset 369 milj. € 0,6 % erityiskorvaukset 662 milj. € 6,8 % lisäkorvaukset 111 milj. € -2,3 % Key figures for medicine sales and their reimbursement in 2007 Change from 2006 Total sales of pharmaceuticals EUR 2,500 million 5.9% prescription medicines in outpatient care (at pharmacy prices with VAT) EUR 1,817 million 4.2% OTC medicines in outpatient care (at pharmacy prices with VAT) EUR 275 million 15.5% sales to hospitals (at wholesale prices) EUR 408 million 7.5% Reimbursement of medicine costs EUR 1,142 million 3.8% Basic Refunds EUR 369 million 0.6% Special Refunds EUR 662 million 6.8% Additional Refunds EUR 111 million -2.3% SUOMEN LÄÄKETILASTO FINNISH STATISTICS ON MEDICINES 2007 Lääkelaitos ja Kansaneläkelaitos National Agency for Medicines and Social Insurance Institution Helsinki 2008 LÄÄKELAITOS KANSANELÄKELAITOS NATIONAL AGENCY SOCIAL INSURANCE FOR MEDICINES INSTITUTION Lääketurvaosasto Tutkimusosasto Department of Safety Research Department and Drug Information Mannerheimintie 103b Nordenskiöldinkatu 12 P.O. Box 55 P.O. Box 450 FI-00301 Helsinki FI-00101 Helsinki Finland Finland Puh. (09) 473 341 Puh. 020 634 11 Tel. +358 9 473 341 Tel. +358 20 634 11 Telekopio (09) 473 34297 Telekopio 020 634 1700 Fax +358 9 473 34297 Fax +358 20 634 1700 ISSN 0786-2180 Kansi / Cover: Kari Piippo Edita Prima Oy Helsinki 2008 SISÄLLYS Kuvaluettelo .....................................................................................................................