Contraception in Adolescents – Regulatory Considerations”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Format (Sample) Dissertation
Providers’ Knowledge, Perceptions and Views of Prescribing Long-Acting Reversible Contraception to Adolescents in a Southwest Community Health Center Item Type text; Electronic Dissertation Authors Schafer, Stephanie Lynne Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 02/10/2021 06:38:23 Link to Item http://hdl.handle.net/10150/626699 PROVIDERS’ KNOWLEDGE, PERCEPTIONS AND VIEWS OF PRESCRIBING LONG-ACTING REVERSIBLE CONTRACEPTION TO ADOLESCENTS IN A SOUTHWEST COMMUNITY HEALTH CENTER by Stephanie Lynne Schafer ________________________ Copyright © Stephanie Lynne Schafer 2017 A DNP Project Submitted to the Faculty of the COLLEGE OF NURSING In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF NURSING PRACTICE In the Graduate College THE UNIVERSITY OF ARIZONA 2 0 1 7 2 3 STATEMENT BY AUTHOR This DNP Project has been submitted in partial fulfillment of requirements for an advanced degree at The University of Arizona and is deposited in the University Library to be made available to borrowers under rules of the Library. Brief quotations from this DNP Project are allowable without special permission, provided that accurate acknowledgment of source is made. Requests for permission for extended quotation from or reproduction of this manuscript in whole or in part may be granted by the head of the major department or the Dean of the Graduate College when in his or her judgment the proposed use of the material is in the interests of scholarship. -

Assessing the Availability, Service Quality, and Price of Essential Medicines In
Assessing the Availability, Service Quality, and Price of Essential Medicines in Private Pharmacies in Afghanistan Norio Kasahara A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2015 Reading Committee: Louis P. Garrison, Jr., Chair Joseph B. Babigumira Andy Stergachis Program Authorized to Offer Degree: Pharmaceutical Outcomes Research and Policy ©Copyright 2015 Norio Kasahara ii Table of Contents Abstract ................................................................................................................................................................................... ................................................................................................ ................................................................................................ .................................................................................. ............... vvv Acknowledgements ................................................................................................................................................................................... ................................................................................................ ................................................................................. ............ viiviivii Summary ................................................................................................................................................................................... ............................................................................................... -
Preven Emergency Contraceptive
9/1/1998 1 Rx Only PREVENÔ Emergency Contraceptive Kit consisting of Emergency Contraceptive Pills and Pregnancy Test Emergency Contraceptive Pills (Levonorgestrel and Ethinyl Estradiol Tablets, USP) and Pregnancy Test The PREVENÔ Emergency Contraceptive Kit is intended to prevent pregnancy after known or suspected contraceptive failure or unprotected intercourse. Emergency contraceptive pills (like all oral contraceptives) do not protect against infection with HIV (the virus that causes AIDS) and other sexually transmitted diseases. DESCRIPTION The PREVENÔ Emergency Contraceptive Kit consists of a patient information book, a urine pregnancy test and four (4) emergency contraceptive pills (ECPs). The pills in the PREVENÔ Emergency Contraceptive Kit are combination oral contraceptives (COCs) which are used to provide postcoital emergency contraception. Each blue film-coated pill contains 0.25 mg levonorgestrel (18,19-Dinorpregn-4-en-20- yn-3-one, 13-Ethyl-17-hydroxy-, (17a)-(-), a totally synthetic progestogen, and 0.05 mg ethinyl estradiol (19-Nor-17a-pregna-1,3,5, (10)-trien-20-yne-3,17-diol). The inactive ingredients present are polacrilin potassium, lactose, magnesium stearate, hydroxypropyl methylcellulose, titanium dioxide, polyethylene glycol, polysorbate 80 and FD&C Blue No.2 Aluminum Lake. MOLECULES TO BE ADDED The Pregnancy Test uses monoclonal antibodies to detect the presence of hCG (Human Chorionic Gonadotropin) in the urine. It is sensitive to 20 – 25 mIU / mL 9/1/1998 2 CLINICAL PHARMACOLOGY ECPs are not effective if the woman is pregnant; they act primarily by inhibiting ovulation. They may also act by altering tubal transport of sperm and/or ova (thereby inhibiting fertilization), and/or possibly altering the endometrium (thereby inhibiting implantation). -

Injectable Birth Control May Raise HIV Infection Risk by 40%
08 January 2018 Injectable birth control may raise HIV infection risk by 40% The intramuscular injectable contraceptive depot medroxyprogesterone acetate, or DMPA, may raise the risk for HIV infection by 40% in women, according to research published recently in Endocrine Reviews. Research indicates alternative contraception methods may help protect women. Professor Janet P. Hapgood, lead author of the review from the University of Cape Town’s (UCT) Department of Molecular and Cell Biology said: “To protect individual and public health, it is important to ensure women in areas with high rates of HIV infection have access to affordable and safe contraceptive options.” In the review, researchers noted that the injectable progestin contraceptive, DMPA, is the major form of hormonal contraceptive used in sub-Saharan Africa, which also has the highest worldwide HIV prevalence, particularly in young women. However, researchers also noted that DMPA may raise the risk for HIV infection by 40% in women. “The increased rate of HIV infection among women using DMPA contraceptive shots is likely due to multiple reasons, including decreases in immune function, and the protective barrier function of the female genital tract. Studying the biology of medroxyprogesterone acetate (MPA) helps us understand what may be driving the increased rate of HIV infection seen in human research,” remarked Hapgood. Increasing the availability of contraceptives that use a different form of progestin than the one found in DMPA could help reduce the risk of HIV transmission. Other forms of contraception, including combined oral contraceptives containing levonorgestrel or the injectable contraceptive norethisterone enanthate (NET-EN), were not associated with increased HIV infection risk. -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

F.8 Ethinylestradiol-Etonogestrel.Pdf
General Items 1. Summary statement of the proposal for inclusion, change or deletion. Here within, please find the evidence to support the inclusion Ethinylestradiol/Etonogestrel Vaginal Ring in the World Health Organization’s Essential Medicines List (EML). Unintended pregnancy is regarded as a serious public health issue both in developed and developing countries and has received growing research and policy attention during last few decades (1). It is a major global concern due to its association with adverse physical, mental, social and economic outcomes. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (2). Even though the incidence of unintended pregnancy has declined globally in the past decade, the rate of unintended pregnancy remains high, particularly in developing regions. (3) Regarding the use of contraceptive vaginal rings, updated bibliography (4,5,6) states that contraceptive vaginal rings (CVR) offer an effective contraceptive option, expanding the available choices of hormonal contraception. Ethinylestradiol/Etonogestrel Vaginal Ring is a non-biodegradable, flexible, transparent with an outer diameter of 54 mm and a cross-sectional diameter of 4 mm. It contains 11.7 mg etonogestrel and 2.7 mg ethinyl estradiol. When placed in the vagina, each ring releases on average 0.120 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol over a three-week period of use. Ethinylestradiol/Etonogestrel Vaginal Ring is intended for women of fertile age. The safety and efficacy have been established in women aged 18 to 40 years. The main advantages of CVRs are their effectiveness (similar or slightly better than the pill), ease of use without the need of remembering a daily routine, user ability to control initiation and discontinuation, nearly constant release rate allowing for lower doses, greater bioavailability and good cycle control with the combined ring, in comparison with oral contraceptives. -

Mycophenolate: OB-GYN Contraception Counseling Referral
Current as of 6/1/2013. This document may not be part of the latest approved REMS. OB/GYN CONTRACEPTION COUNSELING LETTER Reference ID: 3194413 Current as of 6/1/2013. This document may not be part of the latest approved REMS. Letter to Ob/Gyn Contraception Counseling ((Date)) ((Recipient’s Name)) ((Recipient’s Address 1)) ((Recipient’s Address 2)) ((City, State, ZIP)) In reference to: My patient ((Patient’s Name)) Reason for the referral: Contraception counseling Dear Dr ((Recipient’s Last Name)): I am writing to you in reference to the above-named patient who is under my care for ((diagnosis)) and ((insert drug information such as drug name, when patient will begin taking the drug, if treatment has already begun, etc)). This medication contains mycophenolate, which is associated with an increased risk of first trimester pregnancy loss and congenital malformations. It is important that this patient receive contraception counseling about methods that are acceptable for use while taking mycophenolate. Prescribers of mycophenolate participate in the FDA-mandated Mycophenolate REMS (Risk Evaluation and Mitigation Strategy) to ensure that the benefits of mycophenolate outweigh the risks. The following table lists the forms of contraception that are acceptable for use during treatment with mycophenolate. Acceptable Contraception Methods for Females of Reproductive Potential Guide your patients to choose from the following birth control options: Option 1 Intrauterine devices (IUDs) Tubal sterilization Methods to Use Patient’s partner had -

Delaying Menstruation During Holidays. Norethisterone 5Mg Tds
Delaying menstruation during holidays. Norethisterone 5mg tds, started 3 days before the expected menses can be used for the postponement of menstruation and is often prescribed prior to a holiday. The effectiveness of the delay varies between individuals. So what is the problem? A review article in the Journal of Family Planning and Reproductive healthcare ( Mansour 2012) highlighted that owing to the specific structure of norethisterone, it is partly metabolised to ethinyl oestradiol. Chu et al 2007 suggested that a daily dose of norethisterone 5mg tds might be equivalent to taking 20-30mcg combined oral contraceptive pill. Therefore, prescribing therapeutic doses of norethisterone for women with significant risk factors for venous thromboembolism ( VTE) may therefore be inappropriate. Who shouldn’t be given norethisterone? Obese Personal h/o VTE Strong FH of VTE Immobile/wheelchair bound Carriers of thrombophilia Any other condition predisposing to VTE If my patient can’t take norethisterone, what are the alternatives? The metabolism to ethinyl oestradiol occurs with doses of norethisterone 5mg and over and therefore, the concern does not apply to or other progestogens or contraceptive pills containing norethisterone. Mansour suggested Medroxyprogesterone ( MPA ) 10mg three times a day to reduce heavy menstrual bleeding. Dr Sarah Grey (personal communication) recommends 20mg medroxyprogesterone to be taken daily, starting 3 days before the expected onset of menses. However, (MPA) is not licensed for this use and the prescriber should follow the rules of off label prescribing. References Safer prescribing of therapeutic norethisterone for women at risk of venous thromboembolism. Mansour JFPRHC July 2012 Formation of ethinyl oestradiol in women during treatment with norethisterone acetate. -

COMPARISON of the WHO ATC CLASSIFICATION & Ephmra/Intellus Worldwide ANATOMICAL CLASSIFICATION
COMPARISON OF THE WHO ATC CLASSIFICATION & EphMRA/Intellus Worldwide ANATOMICAL CLASSIFICATION: VERSION June 2019 2 Comparison of the WHO ATC Classification and EphMRA / Intellus Worldwide Anatomical Classification The following booklet is designed to improve the understanding of the two classification systems. The development of the two systems had previously taken place separately. EphMRA and WHO are now working together to ensure that there is a convergence of the 2 systems rather than a divergence. In order to better understand the two classification systems, we should pay attention to the way in which substances/products are classified. WHO mainly classifies substances according to the therapeutic or pharmaceutical aspects and in one class only (particular formulations or strengths can be given separate codes, e.g. clonidine in C02A as antihypertensive agent, N02C as anti-migraine product and S01E as ophthalmic product). EphMRA classifies products, mainly according to their indications and use. Therefore, it is possible to find the same compound in several classes, depending on the product, e.g., NAPROXEN tablets can be classified in M1A (antirheumatic), N2B (analgesic) and G2C if indicated for gynaecological conditions only. The purposes of classification are also different: The main purpose of the WHO classification is for international drug utilisation research and for adverse drug reaction monitoring. This classification is recommended by the WHO for use in international drug utilisation research. The EphMRA/Intellus Worldwide classification has a primary objective to satisfy the marketing needs of the pharmaceutical companies. Therefore, a direct comparison is sometimes difficult due to the different nature and purpose of the two systems. -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -

Recommendations for Contraceptive Use, 2013 Adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use, 2Nd Edition
Morbidity and Mortality Weekly Report Early Release / Vol. 62 June 14, 2013 U.S. Selected Practice Recommendations for Contraceptive Use, 2013 Adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use, 2nd Edition Continuing Education Examination available at http://www.cdc.gov/mmwr/cme/conted.html. U.S. Department of Health and Human Services Centers for Disease Control and Prevention Early Release CONTENTS CONTENTS (Continued) Introduction ............................................................................................................1 Appendix A: Summary Chart of U.S. Medical Eligibility Criteria for Methods ....................................................................................................................2 Contraceptive Use, 2010 .................................................................................. 47 How To Use This Document ...............................................................................3 Appendix B: When To Start Using Specific Contraceptive Summary of Changes from WHO SPR ............................................................4 Methods .............................................................................................................. 55 Contraceptive Method Choice .........................................................................4 Appendix C: Examinations and Tests Needed Before Initiation of Maintaining Updated Guidance ......................................................................4 Contraceptive Methods -
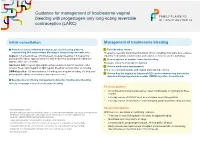
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer.