F.8 Ethinylestradiol-Etonogestrel.Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Levosert 20Microgram/24 Hours Intrauterine Delivery System UK/H/3030/001/DC
PAR Levosert 20microgram/24 hours Intrauterine Delivery System UK/H/3030/001/DC Public Assessment Report Decentralised Procedure LEVOSERT 20MICROGRAM/24 HOURS INTRAUTERINE DELIVERY SYSTEM (levonorgestrel) Procedure No: UK/H/3030/001/DC UK Licence No: PL 30306/0438 ACTAVIS GROUP PTC ehf 1 PAR Levosert 20microgram/24 hours Intrauterine Delivery System UK/H/3030/001/DC LAY SUMMARY Levosert 20 microgram/24 hours Intrauterine Delivery System (levonorgestrel, intrauterine delivery system, 52mg (20 micrograms/24 hours)) This is a summary of the Public Assessment Report (PAR) for Levosert 20 microgram/24 hours Intrauterine Delivery System (PL 30306/0438; UK/H/3030/001/DC, previously PL 34096/0003; UK/H/3030/001/DC). It explains how Levosert 20 microgram/24 hours Intrauterine Delivery System was assessed and its authorisation recommended, as well as its conditions of use. It is not intended to provide practical advice on how to use Levosert 20 microgram/24 hours Intrauterine Delivery System. For practical information about using Levosert 20 microgram/24 hours Intrauterine Delivery System, patients should read the package leaflet or contact their doctor or pharmacist. Levosert 20 microgram/24 hours Intrauterine Delivery System may be referred to as Levosert in this report. What is Levosert and what is it used for? Levosert is an intrauterine delivery system (IUS) for insertion in the womb. It can be used in the following ways: • as an effective method of contraception (prevention of pregnancy); • for heavy menstrual bleeding (heavy periods). Levosert is also useful for reducing menstrual blood flow, so it can be used if you suffer from heavy menstrual bleeding (periods). -

Contraception: Choosing the Right Method for You
Contraception: Choosing the Right Method for You Megan Sax, MD and James L. Whiteside, MD What’s available? Choosing a method of contraception can be overwhelming. The most commonly used methods of reversible contraception in the United States are: hormonal methods the intrauterine device (IUD) the implant barrier methods (e.g. male condom)1 Friends, family, and the Internet are full of stories of failed contraception or bad reactions and these stories can have a big influence that doesn’t always line up with the facts.2 However, knowing these facts is critical to figuring out what type will work best for you. Highly Effective Contraception The best place to start in choosing your contraception is to determine when, if ever, you are planning on starting a family. If you do not wish to become pregnant in the next year, a Long-Acting Reversible Contraceptive (LARC) device may be a good option. LARCs include an implant placed under the skin of the upper, inner arm (brand name Nexplanon) and the IUD. IUDs are placed inside the uterus (see Figure 1). They use copper (brand name ParaGard) or hormones (brand names: Mirena, Lilleta, Skyla, Kyleena) to stop a pregnancy from happening. LARCs are the most effective reversible form of contraception. Less than 1% of users experience unintended pregnancy during the first year of use.3 Currently, the implant Nexplanon is effective for 3 years. The hormonal IUD may be used for 3 to 5 years, depending on the brand. The copper IUD works for 10 years. These devices are inserted and removed by a medical care provider. -
Patch Development with New Drugs Versus Generic Development – Principles and Methods
Patch development with new drugs versus generic development – principles and methods Dr. Barbara Schug SocraTec R&D, Oberursel , Germany www.socratec-pharma.de AGAH Workshop, The new European modified Release Guideline- from cook book to interpretation, Bonn, June 15th –16th, 2015 Some basics Physico-chemical properties / conventional patches small molecule < 500kDa lipophilic potent therapeutic concept which requires low fluctuation Skin controls release rate drug substance dispersed in adhesive matrix Patch controls release rate rate controlling membrane between drug reservoir and skin Currently marketed patches Year Generic (Brand) Names Indication 1979 Scopolamine (Transderm Scop®) Motion sickness 1982 Nitroglycerine (Nitroderm TTS) Angina pectoris 1984 Clonidine (Catapress TTS®) Hypertension 1986 Estradiol (Estraderm®) Menopausal symptoms 1990 Fentanyl (Duragesic®) Chronic pain 1991 Nicotine (Nicoderm®, Habitrol®, Prostep®) Smoking cessation 1993 Testosterone (Androderm®) Testosterone deficiency 1995 Lidocaine/epinephrine (Iontocaine®) Local dermal analgesia 1998 Estradiol/norethindrone (Combipatch®) Menopausal symptoms 1999 Lidocaine (Lidoderm®) Post-herpetic neuralgia pain 2001 Ethinyl estradiol/norelgestromin (OrthoEvra®) Contraception 2003 Estradiol/levonorgestrel (Climara Pro®) Menopause 2003 Oxybutynin (Oxytrol®) Overactive bladder 2004 Lidocaine/ultrasound (SonoPrep®) Local dermal anesthesia Source: modified from Wilson EJ, Three Generations: The Past, Present, and Future of Transdermal Drug Delivery Systems, May 2014 -

Wellness Benefits
Wellness Benefits University of South Alabama This schedule outlines services and items that the University of South Alabama considers a preventive service under this plan. These services must be performed by a physician in the University of South Alabama Health System provider network or by a dermatologist, endocrinologist, durable medical equipment provider, ancillary service provider, urologist, or rheumatologist provider (as applicable) in the entire VIVA HEALTH network. Many of these services are provided as part of an annual physical. This list does not apply to all VIVA HEALTH plans. Please refer to your Summary Plan Description to determine the terms of your health plan. PREVENTIVE SERVICE FREQUENCY/LIMITATIONS Well Baby Visits (Age 0-2) As recommended per guidelines1 Routine screenings, tests, and immunizations As recommended per guidelines Well Child Visits (Age 3-17) One per year at PCP2 Routine screenings, tests, & immunizations As recommended per guidelines HIV screening and counseling As recommended per guidelines Obesity screening As recommended per guidelines Hepatitis B virus screening As recommended per guidelines Sexually transmitted infection counseling Annually Skin cancer behavioral counseling (Beginning at age 10) As recommended per guidelines Routine Physical (Age 18+) One per year at PCP2 Alcohol misuse screening and counseling Annually Blood pressure screening Annually Cholesterol screening As recommended per guidelines Depression screening Annually Diabetes screening As recommended per -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
Recommendations for Contraceptive Use, 2013 Adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use, 2Nd Edition
Morbidity and Mortality Weekly Report Early Release / Vol. 62 June 14, 2013 U.S. Selected Practice Recommendations for Contraceptive Use, 2013 Adapted from the World Health Organization Selected Practice Recommendations for Contraceptive Use, 2nd Edition Continuing Education Examination available at http://www.cdc.gov/mmwr/cme/conted.html. U.S. Department of Health and Human Services Centers for Disease Control and Prevention Early Release CONTENTS CONTENTS (Continued) Introduction ............................................................................................................1 Appendix A: Summary Chart of U.S. Medical Eligibility Criteria for Methods ....................................................................................................................2 Contraceptive Use, 2010 .................................................................................. 47 How To Use This Document ...............................................................................3 Appendix B: When To Start Using Specific Contraceptive Summary of Changes from WHO SPR ............................................................4 Methods .............................................................................................................. 55 Contraceptive Method Choice .........................................................................4 Appendix C: Examinations and Tests Needed Before Initiation of Maintaining Updated Guidance ......................................................................4 Contraceptive Methods -
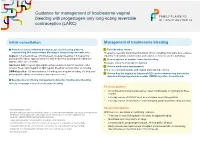
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer. -
Biomedical Technology and Devices Handbook
1140_bookreps.fm Page 1 Tuesday, July 15, 2003 9:47 AM 29 Pharmaceutical Technical Background on Delivery Methods CONTENTS 29.1 Introduction 29.2 Central Nervous System: Drug Delivery Challenges to Delivery: The Blood Brain Barrier • Indirect Routes of Administration • Direct Routes of Administration 29.3 Cardiovascular System: Drug Delivery Chronotherapeutics • Grafts/Stents 29.4 Orthopedic: Drug Delivery Metabolic Bone Diseases 29.5 Muscular System: Drug Delivery 29.6 Sensory: Drug Delivery Ultrasound • Iontophoresis/Electroporation 29.7 Digestive System: Drug Delivery GI Stents • Colonic Drug Delivery 29.8 Pulmonary: Drug Delivery Indirect Routes of Administration • Direct Routes of Robert S. Litman Administration Nova Southeastern University 29.9 Ear, Nose, and Throat: Drug Delivery Maria de la Cova The Ear • The Nose • The Throat 29.10 Lymphatic System: Drug Delivery Icel Gonzalez 29.11 Reproductive System: Drug Delivery University of Memphis Contraceptive Implants • Contraceptive Patch • Male Contraceptive Eduardo Lopez References 29.1 Introduction In the evolution of drug development and manufacturing, drug delivery systems have risen to the forefront in the latest of pharmaceutical advances. There are many new pharmacological entities discov- ered each year, each with its own unique mechanism of action. Each drug will demonstrate its own pharmacokinetic profile. This profile may be changed by altering the drug delivery system to the target site. In order for a drug to demonstrate its pharmacological activity it must be absorbed, transported to the appropriate tissue or target organ, penetrate to the responding subcellular structure, and elicit a response or change an ongoing process. The drug may be simultaneously or sequentially distributed to a variety of tissues, bound or stored, further metabolized to active or inactive products, and eventually © 2004 by CRC Press LLC 1140_bookreps.fm Page 2 Tuesday, July 15, 2003 9:47 AM 29-2 Biomedical Technology and Devices Handbook excreted from the body. -

Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
HORMONAL INTRAUTERINE DEVICES (IUDs) – (Mirena and Kyleena) What are the hormonal intrauterine devices (IUDs)? The hormonal IUDs are small ‘T- shaped’ plastic devices that are inserted into the uterus (womb). The hormonal IUDs contains progestogen. This is a synthetic version of the hormone progesterone made naturally by the ovaries. The hormonal IUDs have a coating (membrane) that controls the slow release of progestogen into the uterus. There are two different hormonal IUDs available in Australia. They are sold as Mirena and Kyleena. How effective are the hormonal IUDs? The hormonal IUDs are more than 99% effective at preventing pregnancy and can last for up to 5 years. They can be used for contraception until 55 years of age if inserted when you are 45 years of age or older. How does the hormonal IUD work? IUDs affect the way sperm move and survive in the uterus (womb), stopping sperm from meeting and fertilising an egg. IUDs can also change the lining of the uterus, making it difficult for a fertilised egg to stick to the lining to start a pregnancy. The hormonal IUDs also work by thickening the fluid around the cervix (opening to the uterus/womb). This helps to prevent sperm from entering. Sometimes the hormonal IUDs can also stop the ovaries from releasing an egg. What are differences between Mirena and Kyleena hormonal IUDs? Both Mirena and Kyleena are very effective methods of contraception that last for up to 5 years. Mirena is 99.9% effective and Kyleena is 99.7% effective. Mirena may be used until 55 years of age if inserted when you are 45 years of age or older, whereas Kyleena needs to be replaced every 5 years for all ages. -

Farr Handouts
4/14/2021 Recent Pharmacological & Faculty Therapeutic Developments in Women’s Health Glen E. Farr, PharmD Professor Emeritus of Clinical Satellite Conference and Live Webcast Pharmacy and Translational Science April 16, 2021 University of Tennessee 9:00 – 12:00 p.m. Central Time College of Pharmacy [email protected] Produced by the Alabama Department of Public Health Video Communications and Distance Learning Division Educational Objectives Still Have • Outline the recent developments, Sugar & guidelines and/or recommendations Spice for pharmacological management of women’s health conditions, with a focus on contraception. • Identify essential information to counsel patients on the therapeutic application of these medications. Edi the Grand Dog’s first visit to our house 1 4/14/2021 2020 Drug Approvals FDA Annual Novel • 53 Novel agents approved Drug Approvals: – Historical previous 10 year average = 40 2011-2020 • 31 Orphan Drugs • 21 “First in Class” 59 53 48 45 46 • 17 Fast-track 39 41 30 • 22 Break-through 27 22 • 30 Priority review 2011 2012 2013 2014 2015 2016 2017 2018 2019 2020 • 12 Accelerated approval FDA.gov Faster FDA Drug Approvals: 3 Question Knowledge Good or Bad? Assessment on • Over the last 4 decades, the FDA has loosened its Contraception requirements for approving new drugs, increasingly accepting less data and more surrogate endpoints in clinical trials, and shortening its reviews. Is this good or bad? • From 1995 to 1997, 80.6% of new drugs were approved on the basis of two pivotal trials — but that number dropped to 52.8% from 2015 to 2017. A number of programs were enacted during the study period that led to faster approvals, such as fast track and the breakthrough therapy designation. -

1 Effects Ethinyl Estradiol Ethinyl Estradiol & Its Effects On
1 Effects Ethinyl Estradiol Ethinyl Estradiol & Its Effects on Cardiovascular Health Mary Eilert Lourdes University Spring 2019 BIO 490 Section A Dr. Anjali Gray 2 Effects Ethinyl Estradiol ABSTRACT Combined hormonal birth control regulates the menstrual cycle in women by manipulating the hormonal level. Combined hormonal contraception utilizes progestin and Ethinyl estradiol, which are synthetics of progesterone and estrogen. These synthetic hormones help regulate ovulation in women and in turn menstruation. Venous thromboembolism (VTE), stroke, and myocardial infarction are all risk factors when taking combined hormonal contraception due to the chemical composition of Ethinyl estradiol. Ethinyl estradiol’s binding mechanism to an estrogen receptor causes clots and therefore a risk for cardiovascular disease. The dosage of Ethinyl estradiol is related to an increased risk for VTE, stroke, and myocardial infarction. Due to the increased threat to cardiovascular health, physicians should screen patient health history carefully when prescribing combined hormonal birth control. Analyzing the risk Ethinyl estradiol poses to cardiovascular health in women can be used to determine if combined hormonal birth control is the ideal choice for contraception. 3 Effects Ethinyl Estradiol INTRODUCTION Birth control, a contraceptive, is frequently prescribed to women of varying ages throughout the United States. Birth control can be used for its primary use as a contraceptive or prescribed as a means of lessening symptoms of reproductive diseases, such as endometriosis. Birth control comes in various forms and methods. Intrauterine devices (IUDs) and birth control implants are forms which are implanted into the women and rely on the release of hormones to regulate the menstrual cycle (Planned Parenthood). -

VTE Prophylaxis in Gynecologic Surgery
ClinicalProviding Information Evidence-based for 25 Years AHC Media LLC Home Page—www.ahcmedia.com CME for Physicians—www.cmeweb.com EDITOR VTE Prophylaxis in Gynecologic Jeffrey T. Jensen, MD, MPH Leon Speroff Professor and Vice Chair for Research Surgery: Quo Vadis? Department of Obstetrics and Gynecology ABSTRACT & COMMENTARY Oregon Health & Science University InsIde Portland Oligohydram- By Robert L. Coleman, MD ASSOCIATE EDITORS nios: A reason Sarah L. Berga, MD Professor and Chair to deliver? Professor, University of Texas; M.D. Anderson Cancer Center, Houston Department of Obstetrics and page 59 Gynecology Vice President for Women’s Dr. Coleman reports no financial relationships relevant to this field of study. Health Services Wake Forest Baptist Health, Winston-Salem, NC Which is Synopsis: Venous thromboembolism (VTE) prophylaxis better: Open, Robert L. Coleman, MD interventions in gynecologic surgery are meritorious, supported Professor, University of laparoscopic, by Level 1 evidence and the subject of multiple guidelines, including Texas; M.D. Anderson Cancer Center, Houston or robotic? those published by the American College of Obstetricians and Gynecologists. However, new evidence suggests nearly Alison Edelman, MD, MPH page 60 Associate Professor, one-third of women undergoing hysterectomy in this country Assistant Director of the still receive no VTE prophylaxis, placing thousands of women at Family Planning Fellowship Special Department of Obstetrics & unnecessary risk for preventable morbidity. Gynecology, Oregon Health feature: & Science University, Portland Do we have a Source: Wright JD, et al. Quality of perioperative venous thromboembolism John C. Hobbins, MD problem? prophylaxis in gynecologic surgery. Obstet Gynecol 2011;118:978-986. Professor, Department of Obstetrics and Gynecology, Obesity and University of Colorado Health contraception he objective of this study was to estimate the use of vte pro- Sciences Center, Denver page 61 Tphylaxis in women undergoing major gynecologic surgery and to Frank W.