Nuvaring (Vaginal Ring) Brown Health Services Patient Education Series
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Which Contraceptive Is Right for You?
IT’S NOT A MATTER OF LUCK! WHICH CONTRACEPTIVE IS RIGHT FOR YOU? @FIUHLP FIU Healthy @FIUHLP FIUHLP @FIUHLPRD Living Program BEFORE YOU GET BUSY…. Prescription/ Can Be Used Pregnancy Doctor’s Protects Contraception Ahead of Time Prevention Visit Need Against STI’s Key Hormonal Available at SHC The N/A Pill/Patch/Ring 90% Yes No N/A Hormonal IUD 99% Yes No N/A Implant 99% Yes No The Shot N/A 99% Yes No Non-Hormonal No Male Condoms 80% No Yes Female Yes Condoms 80% No Yes N/A Copper IUD 99% Yes No Yes Diaphragm 90% Yes No No Spermicide 70% No No Fertility Yes Awareness 75% No No *Pregnancy and STI prevention Sterilization N/A Almost 100% Yes No depends on personal consistent N/A Withdrawal 70% No No Yes and correct use.* Abstinence 100% No Yes Hormonal Spermicide The Pill/Patch/Ring Kills sperm Available in jelly, foam, cream, suppositories, and film Release hormones to inhibit the body’s natural Spermicide must be reapplied every time before sex cyclical hormones to help prevent pregnancy Provides poor protection against pregnancy itself - more Suppress ovulation, thicken the cervical mucus, and effective when used with a barrier method thin the lining of the womb • The Pill must be taken daily. Cervical Cap • The Patch must be replaced weekly. Treated with spermicide • The Ring can be worn for 3 weeks. Can be inserted before sex, and must be left in place 6 hours afterward Hormonal IUD Spermicide must be reapplied every time before sex Requires a doctor’s visit for fitting and another to ensure correct use Thickens cervical mucus and -
Plan C: Copper IUD As Emergency Contraception IMPLEMENTATION TOOLKIT for Administrators and Clinicians
Plan C: Copper IUD as Emergency Contraception IMPLEMENTATION TOOLKIT for Administrators and Clinicians March 2016 Developed by TABLE OF CONTENTS SECTION 1: OVERVIEW ● Introduction Page 1 ● Background Page 2 ● Who It’s For Page 3 ● How to Use It Page 4 ● Additional Considerations Page 5 SECTION 2: ADMINISTRATIVE ● Pre-Implementation Tools Page 6 1.1 Overview: Plan C 1.2 Checklist: Pre-Implementation 1.3 Staff Buy-in 1.4 Checklist: Policies and Procedures 1.5 Sample: Policies and Procedures 1.6 Marketing Plan C 1.7 Sample: Data Collection Tool SECTION 3: CLINICAL ● Implementation Tools Page 21 2.1 The Facts: The Copper-T as Plan C 2.2 Sample: EC Screening Questionnaire 2.3 Triage Scripts 2.4 Contraceptive Counseling 2.5 Eligibility Flowchart: Plan C 2.6 Checklist: Exam Room Preparation 2.7 Checklist: Client-Centered Approach 2.8 Fact Sheet: Copper IUD Aftercare 2.9 Side Effects Management: Steps in the Delivery of Care 2.10 Side Effects Management: Messages, Assessment & Treatment SECTION 4: ADDITIONAL RESOURCES ● Client Education Material: F.A.Q.’s Page 40 ● Client Education Material: EC Chart Page 42 SECTION 5: REFERENCES Page 44 OVERVIEW Introduction The New York State Center of Excellence for Family Planning and Reproductive Health Services (NYS COE) developed this toolkit to support agencies that receive Title X family planning funding through the New York State Department of Health (NYS DOH) Comprehensive Family Planning and Reproductive Health Care Services Program – as well as other sexual and reproductive health service providers – to implement Plan C: Copper IUD as Emergency Contraception (Plan C). -

F.8 Ethinylestradiol-Etonogestrel.Pdf
General Items 1. Summary statement of the proposal for inclusion, change or deletion. Here within, please find the evidence to support the inclusion Ethinylestradiol/Etonogestrel Vaginal Ring in the World Health Organization’s Essential Medicines List (EML). Unintended pregnancy is regarded as a serious public health issue both in developed and developing countries and has received growing research and policy attention during last few decades (1). It is a major global concern due to its association with adverse physical, mental, social and economic outcomes. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (2). Even though the incidence of unintended pregnancy has declined globally in the past decade, the rate of unintended pregnancy remains high, particularly in developing regions. (3) Regarding the use of contraceptive vaginal rings, updated bibliography (4,5,6) states that contraceptive vaginal rings (CVR) offer an effective contraceptive option, expanding the available choices of hormonal contraception. Ethinylestradiol/Etonogestrel Vaginal Ring is a non-biodegradable, flexible, transparent with an outer diameter of 54 mm and a cross-sectional diameter of 4 mm. It contains 11.7 mg etonogestrel and 2.7 mg ethinyl estradiol. When placed in the vagina, each ring releases on average 0.120 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol over a three-week period of use. Ethinylestradiol/Etonogestrel Vaginal Ring is intended for women of fertile age. The safety and efficacy have been established in women aged 18 to 40 years. The main advantages of CVRs are their effectiveness (similar or slightly better than the pill), ease of use without the need of remembering a daily routine, user ability to control initiation and discontinuation, nearly constant release rate allowing for lower doses, greater bioavailability and good cycle control with the combined ring, in comparison with oral contraceptives. -

U.S. Medical Eligibility Criteria for Contraceptive Use, 2016
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 65 / No. 3 July 29, 2016 U.S. Medical Eligibility Criteria for Contraceptive Use, 2016 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS Introduction ............................................................................................................1 Methods ....................................................................................................................2 How to Use This Document ...............................................................................3 Keeping Guidance Up to Date ..........................................................................5 References ................................................................................................................8 Abbreviations and Acronyms ............................................................................9 Appendix A: Summary of Changes from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010 ...........................................................................10 Appendix B: Classifications for Intrauterine Devices ............................. 18 Appendix C: Classifications for Progestin-Only Contraceptives ........ 35 Appendix D: Classifications for Combined Hormonal Contraceptives .... 55 Appendix E: Classifications for Barrier Methods ..................................... 81 Appendix F: Classifications for Fertility Awareness–Based Methods ..... 88 Appendix G: Lactational -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
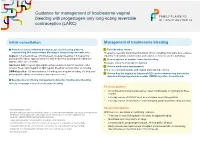
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer. -

Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
HORMONAL INTRAUTERINE DEVICES (IUDs) – (Mirena and Kyleena) What are the hormonal intrauterine devices (IUDs)? The hormonal IUDs are small ‘T- shaped’ plastic devices that are inserted into the uterus (womb). The hormonal IUDs contains progestogen. This is a synthetic version of the hormone progesterone made naturally by the ovaries. The hormonal IUDs have a coating (membrane) that controls the slow release of progestogen into the uterus. There are two different hormonal IUDs available in Australia. They are sold as Mirena and Kyleena. How effective are the hormonal IUDs? The hormonal IUDs are more than 99% effective at preventing pregnancy and can last for up to 5 years. They can be used for contraception until 55 years of age if inserted when you are 45 years of age or older. How does the hormonal IUD work? IUDs affect the way sperm move and survive in the uterus (womb), stopping sperm from meeting and fertilising an egg. IUDs can also change the lining of the uterus, making it difficult for a fertilised egg to stick to the lining to start a pregnancy. The hormonal IUDs also work by thickening the fluid around the cervix (opening to the uterus/womb). This helps to prevent sperm from entering. Sometimes the hormonal IUDs can also stop the ovaries from releasing an egg. What are differences between Mirena and Kyleena hormonal IUDs? Both Mirena and Kyleena are very effective methods of contraception that last for up to 5 years. Mirena is 99.9% effective and Kyleena is 99.7% effective. Mirena may be used until 55 years of age if inserted when you are 45 years of age or older, whereas Kyleena needs to be replaced every 5 years for all ages. -

Condoms & Lubricants
Cornell Health Condoms & Lubricants Live Well to Condoms provide protection against both sexually Learn Well transmitted infections (STI) and pregnancy. Lubricants enhance condom use, as they help Web: prevent condom breakage and can make sexual health.cornell.edu activity more comfortable and pleasurable. There Phone (24/7): are many different kinds of condoms, and cost 607-255-5155 varies from brand to brand. If you have never used condoms, you may want to sample different Fax: brands to find the kind that suit you and your 607-255-0269 partner best. Like condoms, lubricants vary in Appointments: composition and consistency. Experiment to find Monday–Saturday what works best for you and your partner. * Check web for hours, External (sheath) condoms services, providers, Sometimes called “male” condoms, these sheaths and appointment are designed to snugly cover the outside of a information penis. Its tip provides a receptacle to collect Adding lube increases sensation nda also lessens the likelihood of condom breaks 110 Ho Plaza, semen after ejaculation. The sheaths may be made out of latex, polyurethane or animal Ithaca, NY Use condoms before they reach the expiration membrane. They come lubricated and non- 14853-3101 date (check package). Extreme temperatures, lubricated, with spermicide or without, or with a body heat and oil-based lubricants and creams texture or flavor. weaken latex. Do not store condoms in a wallet, Only polyurethane and latex condoms protect pocket or car glove box for more than a few days. * The descriptors against both STIs and pregnancy. (Condoms made Use only water-based or silicone-based lubricants “male” & “female” of animal membrane should be used only for birth with latex condoms. -

Laaketilasto07 2.Pdf
Keskeisiä lukuja lääkkeiden myynnistä ja lääkekorvauksista vuonna 2007 Muutos vuodesta 2006 Lääkkeiden kokonaismyynti 2 500 milj. € 5,9 % avohoidon reseptilääkkeiden myynti (verollisin vähittäismyyntihinnoin) 1 817 milj. € 4,2 % avohoidon itsehoitolääkkeiden myynti (verollisin vähittäismyyntihinnoin) 275 milj. € 15,5 % sairaalamyynti (tukkuohjehinnoin) 408 milj. € 7,5 % Lääkkeistä maksetut korvaukset 1 142 milj. € 3,8 % peruskorvaukset 369 milj. € 0,6 % erityiskorvaukset 662 milj. € 6,8 % lisäkorvaukset 111 milj. € -2,3 % Key figures for medicine sales and their reimbursement in 2007 Change from 2006 Total sales of pharmaceuticals EUR 2,500 million 5.9% prescription medicines in outpatient care (at pharmacy prices with VAT) EUR 1,817 million 4.2% OTC medicines in outpatient care (at pharmacy prices with VAT) EUR 275 million 15.5% sales to hospitals (at wholesale prices) EUR 408 million 7.5% Reimbursement of medicine costs EUR 1,142 million 3.8% Basic Refunds EUR 369 million 0.6% Special Refunds EUR 662 million 6.8% Additional Refunds EUR 111 million -2.3% SUOMEN LÄÄKETILASTO FINNISH STATISTICS ON MEDICINES 2007 Lääkelaitos ja Kansaneläkelaitos National Agency for Medicines and Social Insurance Institution Helsinki 2008 LÄÄKELAITOS KANSANELÄKELAITOS NATIONAL AGENCY SOCIAL INSURANCE FOR MEDICINES INSTITUTION Lääketurvaosasto Tutkimusosasto Department of Safety Research Department and Drug Information Mannerheimintie 103b Nordenskiöldinkatu 12 P.O. Box 55 P.O. Box 450 FI-00301 Helsinki FI-00101 Helsinki Finland Finland Puh. (09) 473 341 Puh. 020 634 11 Tel. +358 9 473 341 Tel. +358 20 634 11 Telekopio (09) 473 34297 Telekopio 020 634 1700 Fax +358 9 473 34297 Fax +358 20 634 1700 ISSN 0786-2180 Kansi / Cover: Kari Piippo Edita Prima Oy Helsinki 2008 SISÄLLYS Kuvaluettelo ..................................................................................................................... -

Etonogestrel/Ethinyl Estradiol Slow Release Vaginal Ring (11.4 Mg/2.6 Mg) to Deliver 120 Mcg Etonogestrel/15 Mcg Ethinyl Estradiol Per Day
PRODUCT MONOGRAPH PrNUVARING® etonogestrel/ethinyl estradiol slow release vaginal ring (11.4 mg/2.6 mg) to deliver 120 mcg etonogestrel/15 mcg ethinyl estradiol per day Contraceptive Vaginal Ring FOR VAGINAL USE ONLY Organon Canada Inc. Date of Revision: 16766 route Transcanadienne Kirkland, Quebec March 25, 2021 www.organon.ca Submission Control No: 249249 NUVARING® Product monograph Page 1 of 59 Table of Contents PART I: HEALTH PROFESSIONAL INFORMATION ......................................................... 3 SUMMARY PRODUCT INFORMATION ........................................................................ 3 INDICATIONS AND CLINICAL USE ............................................................................. 3 CONTRAINDICATIONS ................................................................................................... 3 WARNINGS AND PRECAUTIONS ................................................................................. 4 ADVERSE REACTIONS ................................................................................................. 13 DRUG INTERACTIONS ................................................................................................. 19 DOSAGE AND ADMINISTRATION ............................................................................. 27 OVERDOSAGE ................................................................................................................ 30 ACTION AND CLINICAL PHARMACOLOGY ............................................................ 30 STORAGE AND STABILITY ........................................................................................ -
Progesterone- Releasing Vaginal Ring 8 Key Points for Providers and Clients
Only CHAPTER 8 theEssentials Progesterone- Releasing Vaginal Ring 8 Key Points for Providers and Clients y Suitable for postpartum women who are actively breastfeeding, at least 4 times per day. y A woman places a flexible ring in her vagina. She leaves it in place at all times, every day and night for 90 days. Four rings can be used, one after another, for approximately one year after giving birth. y Start each new ring immediately after removal of the previous ring for greatest effectiveness. Progesterone-Releasing Vaginal Ring Progesterone-Releasing Vaginal y Easy for a woman to insert and remove from her vagina. If her reproductive plans change, she can take out the ring at any time without a provider’s help. What Is the Progesterone-Releasing Vaginal Ring? y A smooth, soft, flexible silicone ring placed in the vagina to prolong lactational amenorrhea (postponing the return of monthly bleeding) and help breastfeeding women space pregnancies. y Continuously releases natural progesterone hormone—like that in a woman’s body—from inside the ring. The hormone passes through the wall of the vagina directly into the bloodstream. This ring does not contain estrogen. y Use of the ring starts 4 to 9 weeks after giving birth. Each ring is kept in place for 90 days. The woman can then replace it with a new ring immediately. Up to 4 rings can be used, one after another, with no breaks. Progesterone-Releasing Vaginal Ring 127 JHU HBk18 - Chapter 6-8.indd 127 1/26/18 09:50 y Works by preventing release of an egg from the ovaries (ovulation). -

Contraception in Adolescents – Regulatory Considerations”
“Contraception in adolescents – regulatory considerations” Wissenschaftliche Prüfungsarbeit zur Erlangung des Titels „Master of Drug Regulatory Affairs“ der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Dr. Julian Paesler aus Münster Bonn 2016 Betreuerin und 1. Referentin: Frau Dr. Ingrid Klingmann Zweiter Referent: Herr Prof. Dr. Niels Eckstein Acknowledgements I would like to express my sincere gratitude to Dr. Ingrid Klingmann for her friendly willingness to function as my “supervising tutor” and for the support and the motivating feedback she gave me during the preparation of this master thesis. Her comments and constructive suggestions were very helpful to me. Besides Dr. Ingrid Klingmann, I would like to thank Prof. Dr. Niels Eckstein for his support and the willingness to function as my “secondary tutor”. Special thanks are also due to my mother, who was willing to proofread this master thesis. I am really thankful for all the support she gave - and still gives – to me, which is way more than what could ever be mentioned here. Table of Contents Table of Contents List of Figures .......................................................................................................................... I List of Tables ......................................................................................................................... III List of Abbreviations ..............................................................................................................