Vaginal Dryness
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Postmenopausal Pharmacotherapy Newsletter
POSTMENOPAUSAL PHARMACOTHERAPY September, 1999 As Canada's baby boomers age, more and more women will face the option of Hormone Replacement Therapy (HRT). The HIGHLIGHTS decision can be a difficult one given the conflicting pros and cons. M This RxFiles examines the role and use of HRT, as well as newer Long term HRT carries several major benefits but also risks SERMS and bisphosphonates in post-menopausal (PM) patients. which should be evaluated on an individual and ongoing basis MContinuous ERT is appropriate for women without a uterus HRT MWomen with a uterus should receive progestagen (at least 12 HRT is indicated for the treatment of PM symptoms such as days per month or continuous low-dose) as part of their HRT vasomotor disturbances and urogenital atrophy, and is considered MLow-dose ERT (CEE 0.3mg) + Ca++ appears to prevent PMO primary therapy for prevention and treatment of postmenopausal MBisphosphinates (e.g. alendronate, etidronate) and raloxifene are osteoporosis (PMO).1 Contraindications are reviewed in Table 2. alternatives to HRT in treating and preventing PMO Although HRT is contraindicated in women with active breast or M"Natural" HRT regimens can be compounded but data is lacking uterine cancer, note that a prior or positive family history of these does not necessarily preclude women from receiving HRT.1 Comparative Safety: Because of differences between products, some side effects may be alleviated by switching from one product Estrogen Replacement Therapy (ERT) 2 to another, particularly from equine to plant sources or from oral to Naturally secreted estrogens include: topical (see Table 3 - Side Effects & Their Management). -

Estrogen Agents, Oral-Transdermal
GEORGIA MEDICAID FEE-FOR-SERVICE ESTROGEN AGENTS, ORAL - TRANSDERMAL PA SUMMARY Preferred Non-Preferred Oral Estrogens Estradiol generic n/a Menest (esterified estrogens) Premarin (estrogens, conjugated) Oral Estrogen/Progestin Combinations Angeliq (drospirenone/estradiol) Bijuva (estradiol/progesterone) Estradiol/norethindrone and all generics for Activella Norethindrone/ethinyl estradiol and all generics for Femhrt Low Dose 0.5/2.5 (norethindrone/ethinyl Femhrt Low Dose estradiol) Jinteli and all generics for Femhrt 1/5 (norethindrone/ethinyl estradiol) Prefest (estradiol/norgestimate) Premphase (conjugated estrogens/medroxyprogesterone) Prempro (conjugated estrogens/medroxyprogesterone) Topical Estrogens Alora (estradiol transdermal patch) Divigel (estradiol topical gel) Estradiol transdermal patch (generic Climara) Elestrin (estradiol topical gel) Evamist (estradiol topical spray solution) Estradiol transdermal patch (generic Vivelle-Dot) Menostar (estradiol transdermal patch) Minivelle (estradiol transdermal patch) Vivelle-Dot (estradiol transdermal patch) Topical Estrogens/Progestin Combination Climara Pro (estradiol/levonorgestrel transdermal patch) n/a Combipatch (estradiol/norethindrone transdermal patch) Oral Selective Estrogen Receptor Modulator (SERMs) Raloxifene generic Duavee (conjugated estrogens/bazedoxifene) Osphena (ospemifene) LENGTH OF AUTHORIZATION: 1 year PA CRITERIA: Bijuva ❖ Approvable for the treatment of moderate to severe vasomotor symptoms associated with menopause in women with an intact uterus who have experienced inadequate response, allergies, contraindications, drug-drug interactions or intolerable side effects to at least two preferred oral estrogen/progestin combination products. Revised 6/29/2020 Norethindrone/Ethinyl Estradiol and All Generics for Femhrt Low Dose ❖ Prescriber must submit a written letter of medical necessity stating the reasons at least two preferred oral estrogen/progestin combination products, one of which must be brand Femhrt Low Dose, are not appropriate for the member. -

F.8 Ethinylestradiol-Etonogestrel.Pdf
General Items 1. Summary statement of the proposal for inclusion, change or deletion. Here within, please find the evidence to support the inclusion Ethinylestradiol/Etonogestrel Vaginal Ring in the World Health Organization’s Essential Medicines List (EML). Unintended pregnancy is regarded as a serious public health issue both in developed and developing countries and has received growing research and policy attention during last few decades (1). It is a major global concern due to its association with adverse physical, mental, social and economic outcomes. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (2). Even though the incidence of unintended pregnancy has declined globally in the past decade, the rate of unintended pregnancy remains high, particularly in developing regions. (3) Regarding the use of contraceptive vaginal rings, updated bibliography (4,5,6) states that contraceptive vaginal rings (CVR) offer an effective contraceptive option, expanding the available choices of hormonal contraception. Ethinylestradiol/Etonogestrel Vaginal Ring is a non-biodegradable, flexible, transparent with an outer diameter of 54 mm and a cross-sectional diameter of 4 mm. It contains 11.7 mg etonogestrel and 2.7 mg ethinyl estradiol. When placed in the vagina, each ring releases on average 0.120 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol over a three-week period of use. Ethinylestradiol/Etonogestrel Vaginal Ring is intended for women of fertile age. The safety and efficacy have been established in women aged 18 to 40 years. The main advantages of CVRs are their effectiveness (similar or slightly better than the pill), ease of use without the need of remembering a daily routine, user ability to control initiation and discontinuation, nearly constant release rate allowing for lower doses, greater bioavailability and good cycle control with the combined ring, in comparison with oral contraceptives. -

Why the Product Labeling for Low-Dose Vaginal Estrogen Should Be Changed
Menopause: The Journal of The North American Menopause Society Vol. 21, No. 9, pp. 911/916 DOI: 10.1097/gme.0000000000000316 * 2014 by The North American Menopause Society EDITORIAL Why the product labeling for low-dose vaginal estrogen should be changed his commentary summarizes the activities of several of a highly effective local treatment of a common condition clinicians and researchers to encourage modifications with medical risks and adverse effects on quality of life. We Tto the labeling of low-dose vaginal estrogen. Motivated contend that the boxed warning for low-dose vaginal es- by concerns of practicing clinicians that the boxed warning on trogen products is unjustified based on several lines of rea- the labels and package inserts for these products overstate po- soning described below, including the following: (a) the tential risks and thus adversely affect patient care, leaders dramatic differences in blood hormone levels achieved by in the field are spearheading an effort to encourage consider- low-dose vaginal estrogen (eg, Vagifem tablets [estradiol ation of alternative labeling, as discussed below. The members 10 Kg], Estring [releasing estradiol 7.5 Kg/d], or comparable of the Working Group on Women’s Health and Well-Being in low-dose vaginal estrogen cream formulations) versus con- Menopause have affiliations with a number of medical socie- ventional systemic estrogen therapy; (b) absence of ran- ties, including The North American Menopause Society, the domized trial evidence or consistent observational evidence American College of Obstetricians and Gynecologists, the En- linking low-dose vaginal estrogen to cancer, cardiovascular docrine Society, the American Society for Reproductive Med- disease, dementia, or any of the other conditions highlighted icine, the International Society for the Study of Women’s in the boxed warning; and (c) absence of evidence that changes in Sexual Health, and other professional organizations. -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
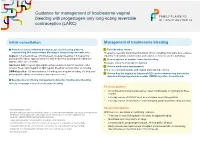
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer. -

Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
HORMONAL INTRAUTERINE DEVICES (IUDs) – (Mirena and Kyleena) What are the hormonal intrauterine devices (IUDs)? The hormonal IUDs are small ‘T- shaped’ plastic devices that are inserted into the uterus (womb). The hormonal IUDs contains progestogen. This is a synthetic version of the hormone progesterone made naturally by the ovaries. The hormonal IUDs have a coating (membrane) that controls the slow release of progestogen into the uterus. There are two different hormonal IUDs available in Australia. They are sold as Mirena and Kyleena. How effective are the hormonal IUDs? The hormonal IUDs are more than 99% effective at preventing pregnancy and can last for up to 5 years. They can be used for contraception until 55 years of age if inserted when you are 45 years of age or older. How does the hormonal IUD work? IUDs affect the way sperm move and survive in the uterus (womb), stopping sperm from meeting and fertilising an egg. IUDs can also change the lining of the uterus, making it difficult for a fertilised egg to stick to the lining to start a pregnancy. The hormonal IUDs also work by thickening the fluid around the cervix (opening to the uterus/womb). This helps to prevent sperm from entering. Sometimes the hormonal IUDs can also stop the ovaries from releasing an egg. What are differences between Mirena and Kyleena hormonal IUDs? Both Mirena and Kyleena are very effective methods of contraception that last for up to 5 years. Mirena is 99.9% effective and Kyleena is 99.7% effective. Mirena may be used until 55 years of age if inserted when you are 45 years of age or older, whereas Kyleena needs to be replaced every 5 years for all ages. -

Chronic Unopposed Vaginal Estrogen Therapy
October, 1999. The Rx Files: Q&A Summary S. Downey BSP, L.D. Regier BSP, BA Chronic Unopposed Vaginal Estrogen Therapy The question of whether progestagen opposition is required in a patient on chronic vaginal estrogen is controversial. The literature is not clear on this matter and the SOGC conference on Menopause did not reach a consensus. Endometrial hyperplasia is directly related to the dose and duration of estrogen therapy. The PEPI study showed that 10 per cent of women taking unopposed estrogen (equivalent to 0.625 mg CEE) will develop complex or atypical endometrial hyperplasia within 1 year. With long-term HRT, it is now considered standard practice to add progestagen opposition to oral estrogen therapy in women with an intact uterus. The case is less clear for vaginal estrogen therapy. The makers of Premarinâ vaginal cream indicate their product is for short term management of urogenital symptoms and the monograph clearly states "precautions recommended with oral estrogen administration should also be observed with this route". In one recent study looking at "Serum and tissue hormone levels of vaginally and orally administered estradiol" (Am J Obstet Gynecol 1999;180:1480-3), serum levels were 10 times higher after vaginal vs. oral administration for exactly the same dose while endometrial concentrations were 70 times higher. This suggests that in some cases very little estrogen is required vaginally to produce significant serum levels and there may be preferential absorption into the endometrium. Hence equivalent vaginal doses may sometimes be much lower on a mg per mg basis compared to oral, largely because of bypassing the "first pass" effect. -

Low-Dose Vaginal Estrogen Therapy
where it works locally to improve the quality of the skin by normalizing its acidity and making it thicker and better lu- bricated. The advantage of using local therapy rather than systemic therapy (i.e. hormone tablets or patches, etc.) is that much lower doses of hormone can be used to achieve good effects in the vagina, while minimizing effects on Low-Dose Vaginal other organs such as the breast or uterus. Vaginal estrogen comes in several forms such as vaginal tablet, creams or gel Estrogen Therapy or in a ring pessary. Is local estrogen therapy safe for me? A Guide for Women Vaginal estrogen preparations act locally on the vaginal 1. Why should I use local estrogen? skin, and minimal, if any estrogen is absorbed into the bloodstream. They work in a similar way to hand or face 2. What is intravaginal estrogen therapy? cream. If you have had breast cancer and have persistent 3. Is local estrogen therapy safe for me? troublesome symptoms which aren’t improving with vagi- 4. Which preparation is best for me? nal moisturizers and lubricants, local estrogen treatment 5. If I am already on HRT, do I need local estrogen may be a possibility. Your Urogynecologist will coordinate the use of vaginal estrogen with your Oncologist. Studies so as well? far have not shown an increased risk of cancer recurrence in women using vaginal estrogen who are undergoing treat- ment of breast cancer or those with history of breast cancer. Which preparation is best for me? Your doctor will be able to advise you on this but most women tolerate all forms of topical estrogen. -

Vaginal Sensitivity to Estrogen As Related to Mammary Tumor Incidence in Mice J.J
Vaginal Sensitivity to Estrogen as Related to Mammary Tumor Incidence in Mice J.J. TRENTIN,PH.D.* (From the Department of Anatomy, Yale Unirersity School of Medicine, New Hauen, Connecticut) The demonstration of the importance of ovarian to estrogen bears no relation to the maternal ex- secretion or exogenous estrogen to a high mam trachromosomal factor. mary tumor incidence in mice was followed by Mühlbock(2,3), from the same laboratory, con numerous studies of the estrous cycles of mice of firmed the higher estrogen requirement (5-7 times different strains, in an attempt to correlate high as much) of the high tumor dba strain as compared mammary tumor incidence with some peculiarity to the low tumor C57 and 020 strains for a com of the cycle. In general, no significant and consist parable degree of vaginal stimulation by either in- ent correlation could be demonstrated in this travaginal or subcutaneous administration of regard. Korteweg and co-workers, however, fo estrogen. cused attention on the possibility that, whereas Sliimkin and Andervont (4) also reported on the outward manifestations of the cycle might be rela vaginal estrogen-sensitivity of three strains of mice tively constant, fundamental differences may exist of known mammary tumor incidence—the C57, in the sensitivity of the genital tissues to estrogen, C, and C3H strains. Again the high tumor strain and that such differences may be related to the was more resistant, the C3H strain requiring twice mammary tumor incidence. Van Gulik and Korte as much estrogen as the low tumor C57 and C, weg (5) reported that of one high tumor and two strains for a positive response in 50 per cent of the low tumor inbred strains, compared with regard to mice. -

Is Vaginal Estrogen Safe If I Had Cancer Or a Heart Attack?
Is Vaginal Estrogen Safe If I had Cancer or a Heart Attack? 27th Annual Primary Health Care of Women Conference Samantha Kempner, MD Assistant Professor Department of Obstetrics and Gynecology Michigan Medicine Please consider the environment before printing this PowerPoint Learning Objectives Describe prevalence and impact of vaginal atrophy for menopausal women Review evidence-based approach to management of vaginal menopausal symptoms Discuss safety of vaginal estrogen for patients with cardiovascular disease or breast cancer Clinical Presentation 52yo G3P2012 calls office with 3rd complaint of dysuria in past 2 months. First time urine culture was obtained and showed E.Coli, second time no improvement on empiric antibiotics, third time culture negative. DDx: ?? Atrophy Sex Med. 2013 Dec: 1 (2): 44-53 D D X Please consider the environment before printing this PowerPoint Clin Med Insights Reprod Health. 2014 Jun 8;8:23-30. Sex Med. 2013 Dec: 1 (2): 44-53 Vulvovaginal Atrophy GSM (genitourinary syndrome of menopause) Impacts up to 85% of menopausal women Up to 70% of women do not discuss condition with a healthcare provider Symptoms include: • Vaginal or vulvar dryness • Dyspareunia • Discharge • Worsening Incontinence • Itching • UTIs Rx: Non-Hormonal Hormonal Other Medications Vaginal lubricants (use Local low-dose vaginal Prasterone (Vaginal DHEA) during intercourse) estrogen is the most • FDA approved vaginal Replens, Vagisil effective treatment for suppository Moisturizer, KY moderate to severe GSM: • MOA likely local Liquibeads -

Nuvaring (Vaginal Ring) Brown Health Services Patient Education Series
NuvaRing (Vaginal Ring) Brown Health Services Patient Education Series You may choose any position that is comfortable for What is the NuvaRing? you: lying down, squatting, or standing with one leg The NuvaRing is a flexible, combined contraceptive propped on a chair. Hold the ring between your vaginal ring, used to prevent pregnancy. NuvaRing thumb and index finger and press the opposite sides contains a combination of progestin and estrogen, of the ring together. Gently push the folded ring two kinds of hormones. The ring is inserted in the into your vagina. vagina and left there for 3 weeks. You then remove it for a 1 week free period. After the ring is inserted, The exact position of the NuvaRing in the vagina is it releases a continuous low dose of hormones into not important for it to work. Most users do not feel your body. The Nuva Ring is 99.7% effective against the ring once it is in place. If you feel discomfort, pregnancy with perfect use, and 93% effective with the NuvaRing is probably not inserted far enough typical use. into your vagina. Just use your finger to gently push What’s in the NuvaRing? NuvaRing further into your vagina. There is no danger of Nuvaring being pushed too far up in the NuvaRing contains two hormones: estrogen and vagina or getting lost. Once inserted keep the progesterone. These hormones are synthetic Nuvaring in place for 3 weeks in a row. You do not versions of naturally occurring hormones. The ring need to remove the ring during sex.