AOGD Bulletin November 2019.Indd
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

University of Groningen the Pill and Thrombosis Van Vlijmen, Elizabeth
University of Groningen The pill and thrombosis van Vlijmen, Elizabeth Femma Willemien IMPORTANT NOTE: You are advised to consult the publisher's version (publisher's PDF) if you wish to cite from it. Please check the document version below. Document Version Publisher's PDF, also known as Version of record Publication date: 2016 Link to publication in University of Groningen/UMCG research database Citation for published version (APA): van Vlijmen, E. F. W. (2016). The pill and thrombosis. Rijksuniversiteit Groningen. Copyright Other than for strictly personal use, it is not permitted to download or to forward/distribute the text or part of it without the consent of the author(s) and/or copyright holder(s), unless the work is under an open content license (like Creative Commons). The publication may also be distributed here under the terms of Article 25fa of the Dutch Copyright Act, indicated by the “Taverne” license. More information can be found on the University of Groningen website: https://www.rug.nl/library/open-access/self-archiving-pure/taverne- amendment. Take-down policy If you believe that this document breaches copyright please contact us providing details, and we will remove access to the work immediately and investigate your claim. Downloaded from the University of Groningen/UMCG research database (Pure): http://www.rug.nl/research/portal. For technical reasons the number of authors shown on this cover page is limited to 10 maximum. Download date: 08-10-2021 Financial support for the printing of this thesis was kindly provided by the Dutch Medicines Evaluation Board and UMCG/GUIDE. -
Lactational Amenorrhea Method
Lactational Amenorrhea Method Dr. Raqibat Idris [email protected] From Research to Practice: Training in Sexual and Reproductive Health Research 2017 Objectives of presentation • Define Lactational Amenorrhea Method (LAM) • Understand the mechanism of action of LAM • Know the efficacy of LAM • Know and describe the 3 criteria for LAM • Know the indication and contraindications for LAM • Know the focus and timing of counselling for LAM • List the advantages, disadvantages and health benefits of LAM • Know the elements of programming necessary for the provision of quality LAM services Introduction Breastfeeding delays the return of a woman’s fertility in the first few months following childbirth. Women who breastfeed are less likely to ovulate in this period. When compared with women who breastfeed partially or who do not breastfeed at all, women who breastfeed more intensively are less likely to have a normal ovulation before their first menstrual bleed postpartum (Berens et al., 2015). In a consensus meeting in Bellagio, Italy in 1998, scientists proposed that women who breastfeed fully or nearly fully while they remain amenorrhoeic in the first 6 months postpartum experience up to 98% protection from pregnancy. This formed the basis for the Lactational Amenorrhea Method and has since then been tested and confirmed by other studies (Berens et al., 2015; Van der Wijden et al., 2003; WHO, 1999). Berens P, Labbok M, The Academy of Breastfeeding Medicine. ABM Clinical Protocol #13: Contraception During Breastfeeding, Revised 2015. Breastfeeding Medicine. 2015 Feb;10(1):3-12. The World Health Organization multinational study of breast-feeding and lactational amenorrhea. III. -

Efficacy of a Selective Estrogen Receptor Modulator: 'Ormeloxifene' in Management of Dysfunctional Uterine Bleeding
JSAFOG CLINICALEfficacy PRACTICEof a Selective Estrogen Receptor Modulator: ‘Ormeloxifene’ in Management of Dysfunctional Uterine Bleeding Efficacy of a Selective Estrogen Receptor Modulator: ‘Ormeloxifene’ in Management of Dysfunctional Uterine Bleeding 1Tapan Kumar Bhattacharyya, 2Anusyua Banerji 1Professor and Head, Department of Obstetrics and Gynecology, SRMS Institute of Medical Sciences, Bareilly, Uttar Pradesh India 2Senior Resident, RG Kar Medical College, Kolkata, West Bengal, India Correspondence: Tapan Kumar Bhattacharyya, Professor and Head, Department of Obstetrics and Gynecology, SRMS Institute of Medical Sciences, Bareilly-243202, Uttar Pradesh, India, Phone: 09748236960, e-mail: [email protected] Abstract Background: Ormeloxifene, a third generation selective estrogen receptor modulator, has been claimed to ameliorate symptoms of DUB. This study was undertaken to compare the efficacy of ormeloxifene and norethisterone. Methods: 180 cases of DUB, who have completed child bearing and are above 35 years, were randomly assigned ormeloxifene, progesterone and iron groups. Ormeloxifene group received ormeloxifene for 12 weeks. Norethisterone group received norethisterone for 12 days in every cycle for six cycles. Iron was given as 60 mg of elemental iron daily. Before starting drug therapy, ultrasound, office hysteroscopy and endometrium sampling for histopathology was obtained and repeated at end of follow-up. The side effects and complications of drug ormeloxifene were noted and relief of symptoms and patient acceptability were compared with norethisterone. Results: 81.7% in the ormeloxifene administered subjects marked relief of symptoms with significant reduction of PBAC scores, reduction of blood clots, and rise in hemoglobin levels. Side effects/complications included amenorrhea, urinary incontinence and genital prolapse. The ease of administration of ormeloxifene facilitated compliance and acceptability. -

Sterilization and Abortion Policy Billing Instructions
Sterilization and Abortion Policy Billing Instructions Table of contents Table of contents ...................................................................................................................................... 1 Hysterectomy ............................................................................................................................................ 2 Acknowledgement forms ..................................................................................................................... 2 Prior authorization requirements ......................................................................................................... 2 Covered services ................................................................................................................................... 2 Intrauterine Devices and Subdermal Implants ......................................................................................... 4 Family planning: sterilization .................................................................................................................... 4 Prior authorization requirements ......................................................................................................... 5 Covered services ................................................................................................................................... 5 Abortion .................................................................................................................................................... 6 Claim -

NFP Related Research ……………………………………………
1 Winter/Spring 2000 ● Vol. 11, Nos. 1 and 2 Richard J. Fehring, DNSc, RN, Marquette University College of Nursing In this issue NFP Related Research ……………………………………………. 2 Pregnancy and Breastfeeding …………………………………….. 8 Contraception ……………………………………………………… 11 Research Briefs …………………………………………………….. 14 Under the Microscope ……………………………………………... 19 The Effectiveness of Natural Family Planning, Robert T. Kambic, MSH Current Medical Research is a publication of the Natural Family Planning Program of the United States Conference of Catholic Bishops.© Washington, DC: USCCB, 2011. The managing editor is Theresa Notare, PhD, Assistant Director. Permission is granted to reproduce in whole or in part, in print and/or electronically, with the following statement: Current Medical Research, NFPP/US Conference of Catholic Bishops, Washington, DC, volume # (year): page#. Used with permission. 2 Natural Family Planning United States Physicians Underestimate Effectiveness of Natural Family Planning A recent study conducted by researchers at the University of Missouri-Columbia, found that 79% of physicians in Missouri estimated the best possible effectiveness of natural family planning for avoiding pregnancy to be less than 91%. Sixty-five percent of those surveyed ranked the actual effectiveness of NFP to be 70% or less.1 The purpose of the study was to determine physicians' knowledge and practices of modern methods of NFP. The researchers assumed that modern methods of NFP are important for medical practice in order to help women and couples avoid or achieve pregnancy. A one page questionnaire on knowledge and practice of NFP was created by the researchers and mailed to 840 randomly selected physicians in Missouri. While 69% of the 547 respondents saw women for reproductive needs, only 46% mentioned NFP to at least some women when discussing family planning issues. -

F.8 Ethinylestradiol-Etonogestrel.Pdf
General Items 1. Summary statement of the proposal for inclusion, change or deletion. Here within, please find the evidence to support the inclusion Ethinylestradiol/Etonogestrel Vaginal Ring in the World Health Organization’s Essential Medicines List (EML). Unintended pregnancy is regarded as a serious public health issue both in developed and developing countries and has received growing research and policy attention during last few decades (1). It is a major global concern due to its association with adverse physical, mental, social and economic outcomes. Developing countries account for approximately 99% of the global maternal deaths in 2015, with sub-Saharan Africa alone accounting for roughly 66% (2). Even though the incidence of unintended pregnancy has declined globally in the past decade, the rate of unintended pregnancy remains high, particularly in developing regions. (3) Regarding the use of contraceptive vaginal rings, updated bibliography (4,5,6) states that contraceptive vaginal rings (CVR) offer an effective contraceptive option, expanding the available choices of hormonal contraception. Ethinylestradiol/Etonogestrel Vaginal Ring is a non-biodegradable, flexible, transparent with an outer diameter of 54 mm and a cross-sectional diameter of 4 mm. It contains 11.7 mg etonogestrel and 2.7 mg ethinyl estradiol. When placed in the vagina, each ring releases on average 0.120 mg/day of etonogestrel and 0.015 mg/day of ethinyl estradiol over a three-week period of use. Ethinylestradiol/Etonogestrel Vaginal Ring is intended for women of fertile age. The safety and efficacy have been established in women aged 18 to 40 years. The main advantages of CVRs are their effectiveness (similar or slightly better than the pill), ease of use without the need of remembering a daily routine, user ability to control initiation and discontinuation, nearly constant release rate allowing for lower doses, greater bioavailability and good cycle control with the combined ring, in comparison with oral contraceptives. -

U.S. Medical Eligibility Criteria for Contraceptive Use, 2016
Morbidity and Mortality Weekly Report Recommendations and Reports / Vol. 65 / No. 3 July 29, 2016 U.S. Medical Eligibility Criteria for Contraceptive Use, 2016 U.S. Department of Health and Human Services Centers for Disease Control and Prevention Recommendations and Reports CONTENTS Introduction ............................................................................................................1 Methods ....................................................................................................................2 How to Use This Document ...............................................................................3 Keeping Guidance Up to Date ..........................................................................5 References ................................................................................................................8 Abbreviations and Acronyms ............................................................................9 Appendix A: Summary of Changes from U.S. Medical Eligibility Criteria for Contraceptive Use, 2010 ...........................................................................10 Appendix B: Classifications for Intrauterine Devices ............................. 18 Appendix C: Classifications for Progestin-Only Contraceptives ........ 35 Appendix D: Classifications for Combined Hormonal Contraceptives .... 55 Appendix E: Classifications for Barrier Methods ..................................... 81 Appendix F: Classifications for Fertility Awareness–Based Methods ..... 88 Appendix G: Lactational -

Vaginal Administration of Contraceptives
Scientia Pharmaceutica Review Vaginal Administration of Contraceptives Esmat Jalalvandi 1,*, Hafez Jafari 2 , Christiani A. Amorim 3 , Denise Freitas Siqueira Petri 4 , Lei Nie 5,* and Amin Shavandi 2,* 1 School of Engineering and Physical Sciences, Heriot-Watt University, Edinburgh EH14 4AS, UK 2 BioMatter Unit, École Polytechnique de Bruxelles, Université Libre de Bruxelles, Avenue F.D. Roosevelt, 50-CP 165/61, 1050 Brussels, Belgium; [email protected] 3 Pôle de Recherche en Gynécologie, Institut de Recherche Expérimentale et Clinique, Université Catholique de Louvain, 1200 Brussels, Belgium; [email protected] 4 Fundamental Chemistry Department, Institute of Chemistry, University of São Paulo, Av. Prof. Lineu Prestes 748, São Paulo 05508-000, Brazil; [email protected] 5 College of Life Sciences, Xinyang Normal University, Xinyang 464000, China * Correspondence: [email protected] (E.J.); [email protected] (L.N.); [email protected] (A.S.); Tel.: +32-2-650-3681 (A.S.) Abstract: While contraceptive drugs have enabled many people to decide when they want to have a baby, more than 100 million unintended pregnancies each year in the world may indicate the contraceptive requirement of many people has not been well addressed yet. The vagina is a well- established and practical route for the delivery of various pharmacological molecules, including contraceptives. This review aims to present an overview of different contraceptive methods focusing on the vaginal route of delivery for contraceptives, including current developments, discussing the potentials and limitations of the modern methods, designs, and how well each method performs for delivering the contraceptives and preventing pregnancy. -
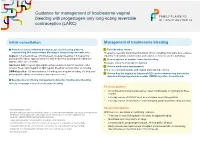
Guidance for Management of Troublesome Vaginal Bleeding with Progestogen-Only Long-Acting Reversible Contraception (LARC)
Guidance for management of troublesome vaginal bleeding with progestogen-only long-acting reversible contraception (LARC) Initial consultation Management of troublesome bleeding Provide accurate Information about expected bleeding patterns, 1. Exclude other causes emphasising that troublesome bleeding is likely to improve with time: Pregnancy, sexually transmitted infections (STIs) including chlamydia, liver-enzyme Implant: 1/5 amenorrhoea, 3/5 infrequent, irregular bleeding, 1/5 frequent or inducing medications (implant only) and vaginal, cervical or uterine pathology prolonged bleeding; approximately 1/2 with frequent or prolonged bleeding will 2. If no suspicion of another cause for bleeding improve after three months. Reassure this is ‘normal’ and not harmful Hormonal IUD: frequent spotting/bleeding common in first 3-5 months; either 3. Advise medication management amenorrhoea, light irregular or light regular bleeding common after six months. Ensure no contraindications and explain risks and side effects DMPA Injection: 1/2 amenorrhoea, 1/6 infrequent irregular bleeding, 1/3 frequent/ prolonged bleeding; amenorrhoea increases over time. 4. Advise that the implant or hormonal IUD can be removed any time or the depot medroxyprogesterone acetate (DMPA) injection discontinued. Be proactive in offering management advice for troublesome bleeding Actively encourage review of troublesome bleeding. First line options: • A combined hormonal contraceptive1 taken continuously or cyclically for three months • Five day course of NSAID2 such as mefenamic acid 500mg bd-tds • Five day course of tranexamic3 acid 500mg bd, particularly if bleeding is heavy Second line options Contraindications include: 1 migraine with aura, personal and family history of venous thromboembolism, risk factor for cardiovascu- With low level, anecdotal or conflicting evidence: lar disease and smoking >35 years of age, active breast cancer. -

Patient Instructions for Post-Vasectomy Fertility Test: Semen Specimen Collection
Patient Instructions for Post-Vasectomy Fertility Test: Semen Specimen Collection Semen specimen 12 weeks after your vasectomy: Twelve weeks (3 months) after your vasectomy, you should collect a semen specimen in the container provided to you by the Urology Department. It is recommended that you have at least 20 ejaculations within the 12-week period after your vasectomy. Depending on the results of your initial sample, you may be asked by your physician to provide another sample. You must utilize an alternate method of contraception until cleared by your physician. You are considered fertile following vasectomy until, as per the American Urological Assn. recommendations, at least one semen analysis shows no fertile sperm. On rare occasions, the vasectomy can fail and the vas deferens tubes can rejoin. Your semen specimen can be brought by yourself to the Urology Clinic only if: It can be in the laboratory within one hour of collection, and It is kept at room temperature during that time. It is suggested, however, that you create your semen specimen while you are at the Urology Clinic. Your semen specimen deposit should be scheduled in advance by Kathy Stevens: call 434-924-9548 or 434- 924-9560. Please note the following important instructions and guidelines for semen collection: The sample should be collected after a minimum of 2 days, and a maximum of 7 days, of sexual abstinence. If you choose to collect the specimen at home, it must be collected in a clean specimen container with a secure lid, such as one with a screw-on cap. -

Hormonal Iuds Are Small ‘T- Shaped’ Plastic Devices That Are Inserted Into the Uterus (Womb)
HORMONAL INTRAUTERINE DEVICES (IUDs) – (Mirena and Kyleena) What are the hormonal intrauterine devices (IUDs)? The hormonal IUDs are small ‘T- shaped’ plastic devices that are inserted into the uterus (womb). The hormonal IUDs contains progestogen. This is a synthetic version of the hormone progesterone made naturally by the ovaries. The hormonal IUDs have a coating (membrane) that controls the slow release of progestogen into the uterus. There are two different hormonal IUDs available in Australia. They are sold as Mirena and Kyleena. How effective are the hormonal IUDs? The hormonal IUDs are more than 99% effective at preventing pregnancy and can last for up to 5 years. They can be used for contraception until 55 years of age if inserted when you are 45 years of age or older. How does the hormonal IUD work? IUDs affect the way sperm move and survive in the uterus (womb), stopping sperm from meeting and fertilising an egg. IUDs can also change the lining of the uterus, making it difficult for a fertilised egg to stick to the lining to start a pregnancy. The hormonal IUDs also work by thickening the fluid around the cervix (opening to the uterus/womb). This helps to prevent sperm from entering. Sometimes the hormonal IUDs can also stop the ovaries from releasing an egg. What are differences between Mirena and Kyleena hormonal IUDs? Both Mirena and Kyleena are very effective methods of contraception that last for up to 5 years. Mirena is 99.9% effective and Kyleena is 99.7% effective. Mirena may be used until 55 years of age if inserted when you are 45 years of age or older, whereas Kyleena needs to be replaced every 5 years for all ages. -
Natural Family Planning
your guide to natural family planning Helping you choose the method of contraception that is best for you natural family planning naturalnatural family family planning planning naturalnatural familynatural family planning planning natural family planning natural family planning familynatural family planning natural family planning natural familynatural planning family planning natural family planning planningnatural family planning natural family planning familynatural planning familynatural family planning planning 2 3 What is the menstrual cycle? Natural family The menstrual cycle is the time from the first day of your period to the day before your next period starts. The average length of the menstrual planning cycle is around 28 days, although many women have longer or shorter cycles and this is normal. This booklet gives information on how natural Regardless of how long or short the cycle is, family planning can help you to avoid pregnancy. ovulation (when the ovaries release an egg) will usually happen around 10–16 days before the Fertility awareness involves being able to identify start of the next period. During your menstrual the signs and symptoms of fertility during cycle: the menstrual cycle so you can plan or avoid O Eggs develop in your ovaries and usually one is pregnancy. released. O The mucus in the cervix (entrance to the uterus – womb) changes to allow sperm to Contents What is the menstrual cycle? .......................................................3 How can I work out how long my menstrual cycle How does natural