Rattlesnake Envenomation
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Snake Bite Protocol
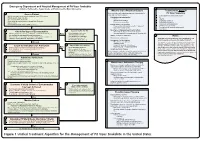
Lavonas et al. BMC Emergency Medicine 2011, 11:2 Page 4 of 15 http://www.biomedcentral.com/1471-227X/11/2 and other Rocky Mountain Poison and Drug Center treatment of patients bitten by coral snakes (family Ela- staff. The antivenom manufacturer provided funding pidae), nor by snakes that are not indigenous to the US. support. Sponsor representatives were not present dur- At the time this algorithm was developed, the only ing the webinar or panel discussions. Sponsor represen- antivenom commercially available for the treatment of tatives reviewed the final manuscript before publication pit viper envenomation in the US is Crotalidae Polyva- ® for the sole purpose of identifying proprietary informa- lent Immune Fab (ovine) (CroFab , Protherics, Nash- tion. No modifications of the manuscript were requested ville, TN). All treatment recommendations and dosing by the manufacturer. apply to this antivenom. This algorithm does not con- sider treatment with whole IgG antivenom (Antivenin Results (Crotalidae) Polyvalent, equine origin (Wyeth-Ayerst, Final unified treatment algorithm Marietta, Pennsylvania, USA)), because production of The unified treatment algorithm is shown in Figure 1. that antivenom has been discontinued and all extant The final version was endorsed unanimously. Specific lots have expired. This antivenom also does not consider considerations endorsed by the panelists are as follows: treatment with other antivenom products under devel- opment. Because the panel members are all hospital- Role of the unified treatment algorithm -
Approach and Management of Spider Bites for the Primary Care Physician
Osteopathic Family Physician (2011) 3, 149-153 Approach and management of spider bites for the primary care physician John Ashurst, DO,a Joe Sexton, MD,a Matt Cook, DOb From the Departments of aEmergency Medicine and bToxicology, Lehigh Valley Health Network, Allentown, PA. KEYWORDS: Summary The class Arachnida of the phylum Arthropoda comprises an estimated 100,000 species Spider bite; worldwide. However, only a handful of these species can cause clinical effects in humans because many Black widow; are unable to penetrate the skin, whereas others only inject prey-specific venom. The bite from a widow Brown recluse spider will produce local symptoms that include muscle spasm and systemic symptoms that resemble acute abdomen. The bite from a brown recluse locally will resemble a target lesion but will develop into an ulcerative, necrotic lesion over time. Spider bites can be prevented by several simple measures including home cleanliness and wearing the proper attire while working outdoors. Although most spider bites cause only local tissue swelling, early species identification coupled with species-specific man- agement may decrease the rate of morbidity associated with bites. © 2011 Elsevier Inc. All rights reserved. More than 100,000 species of spiders are found world- homes and yards in the southwestern United States, and wide. Persons seeking medical attention as a result of spider related species occur in the temperate climate zones across bites is estimated at 50,000 patients per year.1,2 Although the globe.2,5 The second, Lactrodectus, or the common almost all species of spiders possess some level of venom, widow spider, are found in both temperate and tropical 2 the majority are considered harmless to humans. -

Long-Term Effects of Snake Envenoming
toxins Review Long-Term Effects of Snake Envenoming Subodha Waiddyanatha 1,2, Anjana Silva 1,2 , Sisira Siribaddana 1 and Geoffrey K. Isbister 2,3,* 1 Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, Saliyapura 50008, Sri Lanka; [email protected] (S.W.); [email protected] (A.S.); [email protected] (S.S.) 2 South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, University of Peradeniya, Peradeniya 20400, Sri Lanka 3 Clinical Toxicology Research Group, University of Newcastle, Callaghan, NSW 2308, Australia * Correspondence: [email protected] or [email protected]; Tel.: +612-4921-1211 Received: 14 March 2019; Accepted: 29 March 2019; Published: 31 March 2019 Abstract: Long-term effects of envenoming compromise the quality of life of the survivors of snakebite. We searched MEDLINE (from 1946) and EMBASE (from 1947) until October 2018 for clinical literature on the long-term effects of snake envenoming using different combinations of search terms. We classified conditions that last or appear more than six weeks following envenoming as long term or delayed effects of envenoming. Of 257 records identified, 51 articles describe the long-term effects of snake envenoming and were reviewed. Disability due to amputations, deformities, contracture formation, and chronic ulceration, rarely with malignant change, have resulted from local necrosis due to bites mainly from African and Asian cobras, and Central and South American Pit-vipers. Progression of acute kidney injury into chronic renal failure in Russell’s viper bites has been reported in several studies from India and Sri Lanka. Neuromuscular toxicity does not appear to result in long-term effects. -

Venom Evolution Widespread in Fishes: a Phylogenetic Road Map for the Bioprospecting of Piscine Venoms
Journal of Heredity 2006:97(3):206–217 ª The American Genetic Association. 2006. All rights reserved. doi:10.1093/jhered/esj034 For permissions, please email: [email protected]. Advance Access publication June 1, 2006 Venom Evolution Widespread in Fishes: A Phylogenetic Road Map for the Bioprospecting of Piscine Venoms WILLIAM LEO SMITH AND WARD C. WHEELER From the Department of Ecology, Evolution, and Environmental Biology, Columbia University, 1200 Amsterdam Avenue, New York, NY 10027 (Leo Smith); Division of Vertebrate Zoology (Ichthyology), American Museum of Natural History, Central Park West at 79th Street, New York, NY 10024-5192 (Leo Smith); and Division of Invertebrate Zoology, American Museum of Natural History, Central Park West at 79th Street, New York, NY 10024-5192 (Wheeler). Address correspondence to W. L. Smith at the address above, or e-mail: [email protected]. Abstract Knowledge of evolutionary relationships or phylogeny allows for effective predictions about the unstudied characteristics of species. These include the presence and biological activity of an organism’s venoms. To date, most venom bioprospecting has focused on snakes, resulting in six stroke and cancer treatment drugs that are nearing U.S. Food and Drug Administration review. Fishes, however, with thousands of venoms, represent an untapped resource of natural products. The first step in- volved in the efficient bioprospecting of these compounds is a phylogeny of venomous fishes. Here, we show the results of such an analysis and provide the first explicit suborder-level phylogeny for spiny-rayed fishes. The results, based on ;1.1 million aligned base pairs, suggest that, in contrast to previous estimates of 200 venomous fishes, .1,200 fishes in 12 clades should be presumed venomous. -

The Venomous Snakes of Texas Health Service Region 6/5S
The Venomous Snakes of Texas Health Service Region 6/5S: A Reference to Snake Identification, Field Safety, Basic Safe Capture and Handling Methods and First Aid Measures for Reptile Envenomation Edward J. Wozniak DVM, PhD, William M. Niederhofer ACO & John Wisser MS. Texas A&M University Health Science Center, Institute for Biosciences and Technology, Program for Animal Resources, 2121 W Holcombe Blvd, Houston, TX 77030 (Wozniak) City Of Pearland Animal Control, 2002 Old Alvin Rd. Pearland, Texas 77581 (Niederhofer) 464 County Road 949 E Alvin, Texas 77511 (Wisser) Corresponding Author: Edward J. Wozniak DVM, PhD, Texas A&M University Health Science Center, Institute for Biosciences and Technology, Program for Animal Resources, 2121 W Holcombe Blvd, Houston, TX 77030 [email protected] ABSTRACT: Each year numerous emergency response personnel including animal control officers, police officers, wildlife rehabilitators, public health officers and others either respond to calls involving venomous snakes or are forced to venture into the haunts of these animals in the scope of their regular duties. North America is home to two distinct families of native venomous snakes: Viperidae (rattlesnakes, copperheads and cottonmouths) and Elapidae (coral snakes) and southeastern Texas has indigenous species representing both groups. While some of these snakes are easily identified, some are not and many rank amongst the most feared and misunderstood animals on earth. This article specifically addresses all of the native species of venomous snakes that inhabit Health Service Region 6/5s and is intended to serve as a reference to snake identification, field safety, basic safe capture and handling methods and the currently recommended first aide measures for reptile envenomation. -

EMS DIVISION 24.1 Rev. 05/14/2021 PROTOCOL 24 ENVENOMATION, BITES, and STINGS
PROTOCOL 24 ENVENOMATION, BITES, AND STINGS A. North American Pit Vipers B. Coral Snake Bites C. Exotic Snakes D. Brown Recluse Spider Bites E. Black Widow F. Scorpion Stings G. Marine Animal Envenomation H. Marine Animal Stings General Care EMR/BLS 1. Initial Assessment/Care Protocol 1. 2. Attempt to identify the insect, reptile, or animal that caused the injury if it is safe to do so. If unknown or it is a known venomous reptile bite or spider bite, have the FAO contact the Anti-Venom unit. 3. Be alert for the development of any anaphylactic reaction and treat according to the Systemic Reaction Protocol 17. 4. Immobilize the affected area. Keep the patient calm. 5. Remove and secure in a safe location any rings, bracelets, jewelry, etc. that may be in the injured area before swelling becomes too great. 6. Do not apply tourniquets, cold packs, make incisions around the area, or attempt to suction. 7. If unable to contact an Anti-Venom unit, contact the Poison Control Center, 1-800-222-1222 for assistance in managing specific envenomation. Top EMS DIVISION 24.1 Rev. 05/14/2021 PROTOCOL 24 ENVENOMATION, BITES, AND STINGS A. North American Pit Vipers Includes rattlesnakes, copperheads, and cottonmouths. EMR/BLS 1. For any known or suspected bite, refer to Antivenin Bank Procedure 33. Evaluate for specific signs/symptoms: a) Distinct "fang marks" or puncture wounds. b) Swelling and pain at the site. c) Weakness, nausea, and vomiting. d) Paresthesia, fasciculations. e) Numbness and tingling around the face and head. f) Metallic taste, change in taste sensation. -

Epidemiology and Clinical Outcomes of Snakebite in the Elderly: a Toxic Database Study
Clinical Toxicology ISSN: 1556-3650 (Print) 1556-9519 (Online) Journal homepage: http://www.tandfonline.com/loi/ictx20 Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC database study Meghan B. Spyres, Anne-Michelle Ruha, Kurt Kleinschmidt, Rais Vohra, Eric Smith & Angela Padilla-Jones To cite this article: Meghan B. Spyres, Anne-Michelle Ruha, Kurt Kleinschmidt, Rais Vohra, Eric Smith & Angela Padilla-Jones (2018) Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC database study, Clinical Toxicology, 56:2, 108-112, DOI: 10.1080/15563650.2017.1342829 To link to this article: https://doi.org/10.1080/15563650.2017.1342829 Published online: 13 Jul 2017. Submit your article to this journal Article views: 120 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ictx20 CLINICAL TOXICOLOGY, 2018 VOL. 56, NO. 2, 108–112 https://doi.org/10.1080/15563650.2017.1342829 CLINICAL RESEARCH Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC Ã database study Meghan B. Spyresa, Anne-Michelle Ruhab, Kurt Kleinschmidtc, Rais Vohrad, Eric Smithc and Angela Padilla-Jonesb aDepartment of Emergency Medicine, Division of Medical Toxicology, University of Southern California, Los Angeles, CA, USA; bDepartment of Medical Toxicology, Banner-University Medical Center Phoenix, Phoenix, AZ, USA; cDepartment of Emergency Medicine, Univesity of Texas Southwestern Medical Center, Dallas, TX, USA; dDepartment of Emergency Medicine, UCSF Fresno Medical Center, Fresno, CA, USA ABSTRACT ARTICLE HISTORY Introduction: Epidemiologic studies of snakebites in the United States report typical victims to be Received 23 February 2017 young men. -

Snake Venom Detection Kit (SVDK)
SVDK Template In non-urgent situations, serum or plasma may also be used. Other samples such as lymphatic fluid, tissue fluid or extracts may 8. Reading Colour Reactions be used. • Place the test strip on the template provided over page and observe each well continuously over the next 10 minutes whilst the colour develops. Any test sample used in the SVDK must be mixed with Yellow Sample Diluent (YSD-yellow lid), prior to introduction into the The first well to show visible colour, not including the positive control well, is assay. Samples mixed with YSD should be clearly labelled with the patient’s identity and the type of sample used. The volume of diagnostic of the snake’s venom immunotype – see interpretation below. YSD in each sample vial is sufficient to allow retesting of the sample or referral to a reference laboratory for further investigation. Well 1 Tiger Snake Immunotype Snake Venom Detection Kit (SVDK) Note: Strict adherence to the 10 minute observation period after addition of Tiger Snake Antivenom Indicated Detection and Identification of Snake Venom SAMPLE PREPARATION the Chromogen and Peroxide Solutions is essential. Slow development of 1. Prepare the Test Sample. colour in one or more wells after 10 minutes should not be interpreted ENZYME IMMUNOASSAY METHOD • Any test sample used in the SVDK must be mixed with Yellow Sample Diluent (YSD-yellow lid), prior to introduction as positive detection of snake venom. Well 2 Brown Snake Immunotype into the assay. INTERPRETATION OF RESULTS Brown Snake Antivenom Indicated Note: There is enough YSD in one vial to perform two snake venom detection tests. -

First Reported Case of Thrombocytopenia from a Heterodon Nasicus Envenomation T
Toxicon 157 (2019) 12–17 Contents lists available at ScienceDirect Toxicon journal homepage: www.elsevier.com/locate/toxicon Case report First reported case of thrombocytopenia from a Heterodon nasicus envenomation T ∗ Nicklaus Brandehoffa,c, , Cara F. Smithb, Jennie A. Buchanana, Stephen P. Mackessyb, Caitlin F. Bonneya a Rocky Mountain Poison and Drug Center – Denver Health and Hospital Authority, Denver, CO, USA b School of Biological Sciences, University of Northern Colorado, Greeley, CO, USA c University of California, San Francisco-Fresno, Fresno, CA, USA ARTICLE INFO ABSTRACT Keywords: Context: The vast majority of the 2.5 million annual worldwide venomous snakebites are attributed to Viperidae Envenomation or Elapidae envenomations. Of the nearly 2000 Colubridae species described, only a handful are known to cause Colubridae medically significant envenomations. Considered medically insignificant, Heterodon nasicus (Western Hognose Heterodon nasicus Snake) is a North American rear-fanged colubrid common in the legal pet trading industry. Previously reported cases of envenomations describe local pain, swelling, edema, and blistering. However, there are no reported cases of systemic or hematologic toxicity. Case details: A 20-year-old female sustained a bite while feeding a captive H. nasicus causing local symptoms and thrombocytopenia. On day three after envenomation, the patient was seen in the emergency department for persistent pain, swelling, and blistering. At that time, she was found to have a platelet count of 90 × 109/L. Previous routine platelet counts ranged from 315 to 373 × 109/L during the prior two years. Local symptoms peaked on day seven post envenomation. Her local symptoms and thrombocytopenia improved on evaluation four months after envenomation. -

SNAKEBITE ENVENOMATION and DEATH in the DEVELOPING WORLD Luzia S. Cruz, MD
SNAKEBITE ENVENOMATION AND DEATH IN THE DEVELOPING WORLD The purpose of this review is to address the Luzia S. Cruz, MD; Roberto Vargas, MD, MPH; global incidence and management of snake- Antoˆnio Alberto Lopes, MD, MPH, PhD bite envenomation and to describe the clinical characteristics and pathogenesis of envenom- ation by species of the family Viperidae, genera Bothrops and Crotalus, the most INTRODUCTION bite envenomation are reported each common venomous snakes in Brazil. We focus year, with an estimated 35,000–50,000 15,24 on the pathogenesis of the acute renal failure Envenoming from poisonous ani- deaths. In Pakistan, there are 24 induced by these snakes. Envenomation after mals, particularly terrestrial venomous <20,000 snakebite deaths annually. snakebite is an underestimated and neglected In Nepal, there are an estimated 20,000 public health issue responsible for substantial snakes, causes substantial illness and illness and death as well as socioeconomic death and represents an economic snakebites and <200 deaths in hospitals hardship to impoverished populations living in hardship on poor, rural populations annually, predominantly in the eastern 4,24 rural and tropical Africa, Asia, Oceania, and and healthcare systems of tropical and Terai. In Vietnam, from 1992 to Latin America. In developed nations, snake subtropical Africa, Asia, Oceania, and 1998, there were an estimated 300,000 bite typically occurs during recreational activ- 1–25 ities, whereas in developing countries it is an Latin America. Although mortality bites per year, and a case fatality ratio of occupational disease more likely to affect from snakebite is estimated to be one- 22% was reported among plantation young agricultural workers, predominantly tenth that of malaria, no equivalent workers bitten by Malayan pit vipers.24 men. -

A Review on the Scorpaena Plumieri Fish Venom and Its Bioactive Compounds Fabiana V
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Springer - Publisher Connector Campos et al. Journal of Venomous Animals and Toxins including Tropical Diseases (2016) 22:35 DOI 10.1186/s40409-016-0090-7 REVIEW Open Access A review on the Scorpaena plumieri fish venom and its bioactive compounds Fabiana V. Campos1, Thiago N. Menezes1, Pedro F. Malacarne1, Fábio L. S. Costa2, Gustavo B. Naumann1,3, Helena L. Gomes1 and Suely G. Figueiredo1* Abstract The most poisonous fish species found along the Brazilian coast is the spotted scorpionfish Scorpaena plumieri. Though hardly ever life-threatening to humans, envenomation by S. plumieri can be quite hazardous, provoking extreme pain and imposing significant socioeconomic costs, as the victims may require days to weeks to recover from their injuries. In this review we will walk the reader through the biological features that distinguish this species as well as the current epidemiological knowledge related to the envenomation and its consequences. But above all, we will discuss the challenges involved in the biochemical characterization of the S. plumieri venom and its compounds, focusing then on the successful isolation and pharmacological analysis of some of the bioactive molecules responsible for the effects observed upon envenomation as well as on experimental models. Despite the achievement of considerable progress, much remains to be done, particularly in relation to the non-proteinaceous components of the venom. Therefore, further studies are necessary in order to provide a more complete picture of the venom’s chemical composition and physiological effects. Given that fish venoms remain considerably less studied when compared to terrestrial venoms, the exploration of their full potential opens a myriad of possibilities for the development of new drug leads and tools for elucidating the complex physiological processes. -

Post-Exposure Treatment of Ebola Virus Using Passive Immunotherapy: Proposal for a New Strategy Jean-Philippe Chippaux1,4*, Leslie V Boyer2 and Alejandro Alagón3
Chippaux et al. Journal of Venomous Animals and Toxins including Tropical Diseases (2015) 21:3 DOI 10.1186/s40409-015-0003-1 REVIEW Open Access Post-exposure treatment of Ebola virus using passive immunotherapy: proposal for a new strategy Jean-Philippe Chippaux1,4*, Leslie V Boyer2 and Alejandro Alagón3 Abstract Background: Better treatments are urgently needed for the management of Ebola virus epidemics in Equatorial Africa. Methods: We conducted a systematic review of the literature on the use of passive immunotherapy for the treatment or prevention of Ebola virus disease. We placed findings from this review into the context of passive immunotherapy currently used for venom-induced disease, and recent improvements in manufacturing of polyvalent antivenom products. Results: Passive immunotherapy appears to be one of the most promising specific treatments for Ebola. However, its potential has been incompletely evaluated, considering the overall experience and recent improvement of immunotherapy. Development and use of heterologous serum derivatives could protect people exposed to Ebola viruses with reasonable cost and logistics. Conclusion: Hyperimmune equine IgG fragments and purified polyclonal whole IgG deserve further consideration as treatment for exposure to the Ebola virus. Keywords: Ebola, Epidemics, Immunotherapy, Prophylaxis, Africa Introduction human patients was a priority [1]. However, heterologous The epidemic of Ebola virus disease (EVD) currently tak- animal products are not under clinical investigation. ing place in West Africa has revived debate on the treat- Passive immunotherapy of animal origin has been used ment of this severe infection [1]. Experimental treatment for over 120 years to treat bacterial and viral infections, consisting of monoclonal antibodies has been used com- envenomations and drug intoxications [3].