A CLINICO-EPIDEMIOLOGICAL STUDY of BITES by SPIDERS of the GENUS Phoneutria
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

By Phoneutria Nigriventer (Aranae: Ctenidae) in Atlantic Forest, South-East of Brazil
Herpetology Notes, volume 10: 369-371 (2017) (published online on 03 July 2017) Predation on Physalaemus olfersii (Anura: Leptodactylidae) by Phoneutria nigriventer (Aranae: Ctenidae) in Atlantic Forest, South-east of Brazil Mariana Pedrozo1,*, Lucas de Souza Almeida2, Matheus de Toledo Moroti3 and Diego José Santana3 Anurans are essential in trophic chains (Duellman and mm of snout-vent length in males and 22.4–41.1 mm Trueb, 1994), and are preyed upon many vertebrates and in females (Cassini et al. 2010), and is distributed in invertebrates (Toledo et al., 2007). Usually, predation the Atlantic Rain Forest domain and its influence areas, on anurans by invertebrates occurs mostly during from the municipality of Santa Teresa, state of Espírito larval and adult stages, but they also attack on anuran Santo, southern region of the states of Minas Gerais and spawns (Downie et al., 1995; Santos, 2009). Among São Paulo (Cassini et al. 2010). Ctenid spiders of the the invertebrates that may feed on anurans, there are genus Phoneutria have already been reported as anuran records of beetles, waterbugs, ants, spiders and crabs predators (Rego et al., 2005, Santana et al., 2009, Caldart (Duellman and Trueb, 1994; Toledo et al., 2005; Caldart et al., 2011, Pacheco et al., 2016), and are nocturnal with et al., 2011). Predation events, involving anurans and wandering habits, which actively seek their prey (Lucas, invertebrates, may be trivial in nature, however these 1988). According to Brazil et al. (2009), Phoneutria records are dependent of fortuitous observations nigriventer (Keyserling, 1891) has a wide distribution, (Pombal Jr, 2007; Santana et al., 2009). -
Snake Bite Protocol
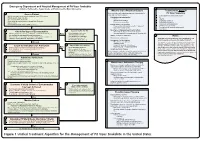
Lavonas et al. BMC Emergency Medicine 2011, 11:2 Page 4 of 15 http://www.biomedcentral.com/1471-227X/11/2 and other Rocky Mountain Poison and Drug Center treatment of patients bitten by coral snakes (family Ela- staff. The antivenom manufacturer provided funding pidae), nor by snakes that are not indigenous to the US. support. Sponsor representatives were not present dur- At the time this algorithm was developed, the only ing the webinar or panel discussions. Sponsor represen- antivenom commercially available for the treatment of tatives reviewed the final manuscript before publication pit viper envenomation in the US is Crotalidae Polyva- ® for the sole purpose of identifying proprietary informa- lent Immune Fab (ovine) (CroFab , Protherics, Nash- tion. No modifications of the manuscript were requested ville, TN). All treatment recommendations and dosing by the manufacturer. apply to this antivenom. This algorithm does not con- sider treatment with whole IgG antivenom (Antivenin Results (Crotalidae) Polyvalent, equine origin (Wyeth-Ayerst, Final unified treatment algorithm Marietta, Pennsylvania, USA)), because production of The unified treatment algorithm is shown in Figure 1. that antivenom has been discontinued and all extant The final version was endorsed unanimously. Specific lots have expired. This antivenom also does not consider considerations endorsed by the panelists are as follows: treatment with other antivenom products under devel- opment. Because the panel members are all hospital- Role of the unified treatment algorithm -
Approach and Management of Spider Bites for the Primary Care Physician
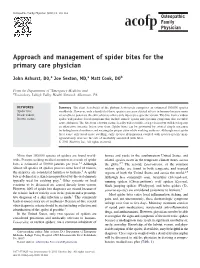
Osteopathic Family Physician (2011) 3, 149-153 Approach and management of spider bites for the primary care physician John Ashurst, DO,a Joe Sexton, MD,a Matt Cook, DOb From the Departments of aEmergency Medicine and bToxicology, Lehigh Valley Health Network, Allentown, PA. KEYWORDS: Summary The class Arachnida of the phylum Arthropoda comprises an estimated 100,000 species Spider bite; worldwide. However, only a handful of these species can cause clinical effects in humans because many Black widow; are unable to penetrate the skin, whereas others only inject prey-specific venom. The bite from a widow Brown recluse spider will produce local symptoms that include muscle spasm and systemic symptoms that resemble acute abdomen. The bite from a brown recluse locally will resemble a target lesion but will develop into an ulcerative, necrotic lesion over time. Spider bites can be prevented by several simple measures including home cleanliness and wearing the proper attire while working outdoors. Although most spider bites cause only local tissue swelling, early species identification coupled with species-specific man- agement may decrease the rate of morbidity associated with bites. © 2011 Elsevier Inc. All rights reserved. More than 100,000 species of spiders are found world- homes and yards in the southwestern United States, and wide. Persons seeking medical attention as a result of spider related species occur in the temperate climate zones across bites is estimated at 50,000 patients per year.1,2 Although the globe.2,5 The second, Lactrodectus, or the common almost all species of spiders possess some level of venom, widow spider, are found in both temperate and tropical 2 the majority are considered harmless to humans. -

Accidents Caused by Spider Bites
Open Journal of Animal Sciences, 2014, 4, 113-117 Published Online June 2014 in SciRes. http://www.scirp.org/journal/ojas http://dx.doi.org/10.4236/ojas.2014.43015 Accidents Caused by Spider Bites Annelise Carla Camplesi1*, Sthefani Soares Albernaz1, Karina Paes Burger1, Carla Fredrichsen Moya-Araujo2 1School of Agriculture and Veterinary Science, Sao Paulo State University—UNESP, Jaboticabal, Brazil 2School of Veterinary Medicine—FIO, Ourinhos, Brazil Email: *[email protected] Received 9 April 2014; revised 15 May 2014; accepted 22 May 2014 Copyright © 2014 by authors and Scientific Research Publishing Inc. This work is licensed under the Creative Commons Attribution International License (CC BY). http://creativecommons.org/licenses/by/4.0/ Abstract Accidents caused by spider bites occur in many countries and represent a public health problem due to their high severity and occurrence of fatal accidents. In Veterinary Medicine, the incidence of arachnidism is considered nonexistent in large animals, as their thick skin cannot be pierced, rare in cats and common in dogs, particularly due to their exploratory and curious habit, and the habitats of venomous animals, such as the arachnids, located close to urban areas. The aim of this review is to describe the characteristics and distribution of spiders, the mechanism of action of the venom, clinical signs, diagnosis and treatment of accidents caused by arachnids of genera Loxos- celes sp., Phoneutria sp., Latrodectus sp., and suborder Mygalomorphae. Keywords Arachnids, Clinical Signs, Diagnosis, Treatment 1. Introduction Spiders are the second largest order of arachnids, with more than 41,000 species described. Practically all of them are venomous, but only some of them have potential significance to human medicine and veterinary medi- cine, due to their venom toxicity, habitat of species, among other factors [1]. -

Long-Term Effects of Snake Envenoming
toxins Review Long-Term Effects of Snake Envenoming Subodha Waiddyanatha 1,2, Anjana Silva 1,2 , Sisira Siribaddana 1 and Geoffrey K. Isbister 2,3,* 1 Faculty of Medicine and Allied Sciences, Rajarata University of Sri Lanka, Saliyapura 50008, Sri Lanka; [email protected] (S.W.); [email protected] (A.S.); [email protected] (S.S.) 2 South Asian Clinical Toxicology Research Collaboration, Faculty of Medicine, University of Peradeniya, Peradeniya 20400, Sri Lanka 3 Clinical Toxicology Research Group, University of Newcastle, Callaghan, NSW 2308, Australia * Correspondence: [email protected] or [email protected]; Tel.: +612-4921-1211 Received: 14 March 2019; Accepted: 29 March 2019; Published: 31 March 2019 Abstract: Long-term effects of envenoming compromise the quality of life of the survivors of snakebite. We searched MEDLINE (from 1946) and EMBASE (from 1947) until October 2018 for clinical literature on the long-term effects of snake envenoming using different combinations of search terms. We classified conditions that last or appear more than six weeks following envenoming as long term or delayed effects of envenoming. Of 257 records identified, 51 articles describe the long-term effects of snake envenoming and were reviewed. Disability due to amputations, deformities, contracture formation, and chronic ulceration, rarely with malignant change, have resulted from local necrosis due to bites mainly from African and Asian cobras, and Central and South American Pit-vipers. Progression of acute kidney injury into chronic renal failure in Russell’s viper bites has been reported in several studies from India and Sri Lanka. Neuromuscular toxicity does not appear to result in long-term effects. -

Venom Evolution Widespread in Fishes: a Phylogenetic Road Map for the Bioprospecting of Piscine Venoms
Journal of Heredity 2006:97(3):206–217 ª The American Genetic Association. 2006. All rights reserved. doi:10.1093/jhered/esj034 For permissions, please email: [email protected]. Advance Access publication June 1, 2006 Venom Evolution Widespread in Fishes: A Phylogenetic Road Map for the Bioprospecting of Piscine Venoms WILLIAM LEO SMITH AND WARD C. WHEELER From the Department of Ecology, Evolution, and Environmental Biology, Columbia University, 1200 Amsterdam Avenue, New York, NY 10027 (Leo Smith); Division of Vertebrate Zoology (Ichthyology), American Museum of Natural History, Central Park West at 79th Street, New York, NY 10024-5192 (Leo Smith); and Division of Invertebrate Zoology, American Museum of Natural History, Central Park West at 79th Street, New York, NY 10024-5192 (Wheeler). Address correspondence to W. L. Smith at the address above, or e-mail: [email protected]. Abstract Knowledge of evolutionary relationships or phylogeny allows for effective predictions about the unstudied characteristics of species. These include the presence and biological activity of an organism’s venoms. To date, most venom bioprospecting has focused on snakes, resulting in six stroke and cancer treatment drugs that are nearing U.S. Food and Drug Administration review. Fishes, however, with thousands of venoms, represent an untapped resource of natural products. The first step in- volved in the efficient bioprospecting of these compounds is a phylogeny of venomous fishes. Here, we show the results of such an analysis and provide the first explicit suborder-level phylogeny for spiny-rayed fishes. The results, based on ;1.1 million aligned base pairs, suggest that, in contrast to previous estimates of 200 venomous fishes, .1,200 fishes in 12 clades should be presumed venomous. -

The Venomous Snakes of Texas Health Service Region 6/5S
The Venomous Snakes of Texas Health Service Region 6/5S: A Reference to Snake Identification, Field Safety, Basic Safe Capture and Handling Methods and First Aid Measures for Reptile Envenomation Edward J. Wozniak DVM, PhD, William M. Niederhofer ACO & John Wisser MS. Texas A&M University Health Science Center, Institute for Biosciences and Technology, Program for Animal Resources, 2121 W Holcombe Blvd, Houston, TX 77030 (Wozniak) City Of Pearland Animal Control, 2002 Old Alvin Rd. Pearland, Texas 77581 (Niederhofer) 464 County Road 949 E Alvin, Texas 77511 (Wisser) Corresponding Author: Edward J. Wozniak DVM, PhD, Texas A&M University Health Science Center, Institute for Biosciences and Technology, Program for Animal Resources, 2121 W Holcombe Blvd, Houston, TX 77030 [email protected] ABSTRACT: Each year numerous emergency response personnel including animal control officers, police officers, wildlife rehabilitators, public health officers and others either respond to calls involving venomous snakes or are forced to venture into the haunts of these animals in the scope of their regular duties. North America is home to two distinct families of native venomous snakes: Viperidae (rattlesnakes, copperheads and cottonmouths) and Elapidae (coral snakes) and southeastern Texas has indigenous species representing both groups. While some of these snakes are easily identified, some are not and many rank amongst the most feared and misunderstood animals on earth. This article specifically addresses all of the native species of venomous snakes that inhabit Health Service Region 6/5s and is intended to serve as a reference to snake identification, field safety, basic safe capture and handling methods and the currently recommended first aide measures for reptile envenomation. -

Rattlesnake Envenomation
Rattlesnake Bite Reviewers: Shawn M. Varney, Authors: Laura Morrison, MD / Ryan Chuang, MD MD Target Audience: Emergency Medicine Residents (junior and senior level postgraduate learners), Medical Students Primary Learning Objectives: 1. Recognize signs and symptoms of a venomous snakebite. 2. Recognize the indications for antivenom administration. 3. Recognize potentially dangerous complications of a snakebite and antivenom administration. Secondary Learning Objectives: detailed technical/behavioral goals, didactic points 1. Obtain medication history and evaluate for use of anticoagulant medications 2. Discuss importance of reevaluation of local effects 3. Describe the importance of removing tourniquets that may have been placed prior to arrival in ED 4. Describe the types of toxicity that can result from rattlesnake envenomation Critical actions checklist: 1. Obtain peripheral IV access (in contralateral arm) 2. Order coagulation studies (CBC, platelets, INR, fibrinogen) 3. Administer antivenom 4. Stop antivenom infusion when anaphylactic/anaphylactoid reaction to antivenom develops 5. Provide volume resuscitation for anaphylactic/anaphylactoid reaction 6. Administer medications for anaphylaxis 7. Consult Poison Center/Toxicologist 8. Admit to the MICU Environment: Emergency Department treatment area 1. Room Set Up – ED critical care area a. Manikin Set Up – Mid or high fidelity simulator b. Props – Standard ED equipment 2. Distractors – ED noise, alarming monitor For Examiner Only CASE SUMMARY SYNOPSIS OF HISTORY/ Scenario Background This is a case of a 32-year-old man who is brought to the emergency department reporting a snakebite by a prairie rattlesnake while working in the local zoo that afternoon. He reports severe pain at the site and progressive swelling up his arm since the bite 2-3 hours ago. -

Redalyc.ACCIDENTS CAUSED by PHONEUTRIA NIGRIVENTER
Revista de Pesquisa Cuidado é Fundamental Online E-ISSN: 2175-5361 [email protected] Universidade Federal do Estado do Rio de Janeiro Brasil Barbosa de Medeiros, Stephanie; Fernandes Dutra Pereira, Camila Dannyelle; da Silva Ribeiro, Joyce Laíse; Gurgel Guerra Fernandes, Liva; Delfino de Medeiros, Priscilla; Viera Tourinho, Francis Solange ACCIDENTS CAUSED BY PHONEUTRIA NIGRIVENTER: DIAGNOSIS AND NURSING INTERVENTIONS Revista de Pesquisa Cuidado é Fundamental Online, vol. 5, núm. 4, octubre-diciembre, 2013, pp. 467-474 Universidade Federal do Estado do Rio de Janeiro Rio de Janeiro, Brasil Available in: http://www.redalyc.org/articulo.oa?id=505750942042 How to cite Complete issue Scientific Information System More information about this article Network of Scientific Journals from Latin America, the Caribbean, Spain and Portugal Journal's homepage in redalyc.org Non-profit academic project, developed under the open access initiative ISSN 2175-5361 DOI: 10.9789/2175-5361.2013v5n4p467 Medeiros SB, Pereira CDFD, Ribeiro JLS et al. Accidents caused by… INTEGRATIVE REVIEW OF LITERATURE ACCIDENTS CAUSED BY PHONEUTRIA NIGRIVENTER: DIAGNOSIS AND NURSING INTERVENTIONS ACIDENTES CAUSADOS POR PHONEUTRIA NIGRIVENTER: DIAGNÓSTICOS E INTERVENÇÕES DE ENFERMAGEM ACCIDENTES CAUSADOS POR PHONEUTRIA NIGRIVENTER: DIAGNÓSTICOS E INTERVENCIONES DE ENFERMERÍA Stephanie Barbosa de Medeiros1, Camila Dannyelle Fernandes Dutra Pereira2, Joyce Laíse da Silva Ribeiro3, Liva Gurgel Guerra Fernandes4, Priscilla Delfino de Medeiros5, Francis Solange Viera Tourinho6 ABSTRACT Objective: To identify the main nursing diagnostic labels and the respective interventions through the main clinical manifestations presented by individuals poisoned by the venom of the spider Phoneutria nigriventer found in the literature. Method: Integrative review of literature consulted in PubMed and BVS databases, printed publications and official websites related to the theme. -

West Nile Virus in Brazil
pathogens Article West Nile Virus in Brazil Érica Azevedo Costa 1,†, Marta Giovanetti 2,3,† , Lilian Silva Catenacci 4,† , Vagner Fonseca 3,5,6,† , Flávia Figueira Aburjaile 3,† , Flávia L. L. Chalhoub 2, Joilson Xavier 3 , Felipe Campos de Melo Iani 7 , Marcelo Adriano da Cunha e Silva Vieira 8, Danielle Freitas Henriques 9, Daniele Barbosa de Almeida Medeiros 9, Maria Isabel Maldonado Coelho Guedes 1 , Beatriz Senra Álvares da Silva Santos 1 , Aila Solimar Gonçalves Silva 1, Renata de Pino Albuquerque Maranhão 10, Nieli Rodrigues da Costa Faria 2, Renata Farinelli de Siqueira 11 , Tulio de Oliveira 5, Karina Ribeiro Leite Jardim Cavalcante 12, Noely Fabiana Oliveira de Moura 12, Alessandro Pecego Martins Romano 12, Carlos F. Campelo de Albuquerque 13, Lauro César Soares Feitosa 14 , José Joffre Martins Bayeux 15 , Raffaella Bertoni Cavalcanti Teixeira 16 , Osmaikon Lisboa Lobato 17 , Silvokleio da Costa Silva 17 , Ana Maria Bispo de Filippis 2, Rivaldo Venâncio da Cunha 18, José Lourenço 19 and Luiz Carlos Junior Alcantara 2,3,* 1 Departamento de Medicina Veterinária Preventiva, Universidade Federal de Minas Gerais, Belo Horizonte 31270-901, Brazil; [email protected] (É.A.C.); [email protected] (M.I.M.C.G.); [email protected] (B.S.Á.d.S.S.); [email protected] (A.S.G.S.) 2 Laboratório de Flavivírus, Instituto Oswaldo Cruz, Fundação Oswaldo Cruz, Rio de Janeiro 21040-360, Brazil; [email protected] (M.G.); fl[email protected] (F.L.L.C.); [email protected] (N.R.d.C.F.); ana.bispo@ioc.fiocruz.br -

EMS DIVISION 24.1 Rev. 05/14/2021 PROTOCOL 24 ENVENOMATION, BITES, and STINGS
PROTOCOL 24 ENVENOMATION, BITES, AND STINGS A. North American Pit Vipers B. Coral Snake Bites C. Exotic Snakes D. Brown Recluse Spider Bites E. Black Widow F. Scorpion Stings G. Marine Animal Envenomation H. Marine Animal Stings General Care EMR/BLS 1. Initial Assessment/Care Protocol 1. 2. Attempt to identify the insect, reptile, or animal that caused the injury if it is safe to do so. If unknown or it is a known venomous reptile bite or spider bite, have the FAO contact the Anti-Venom unit. 3. Be alert for the development of any anaphylactic reaction and treat according to the Systemic Reaction Protocol 17. 4. Immobilize the affected area. Keep the patient calm. 5. Remove and secure in a safe location any rings, bracelets, jewelry, etc. that may be in the injured area before swelling becomes too great. 6. Do not apply tourniquets, cold packs, make incisions around the area, or attempt to suction. 7. If unable to contact an Anti-Venom unit, contact the Poison Control Center, 1-800-222-1222 for assistance in managing specific envenomation. Top EMS DIVISION 24.1 Rev. 05/14/2021 PROTOCOL 24 ENVENOMATION, BITES, AND STINGS A. North American Pit Vipers Includes rattlesnakes, copperheads, and cottonmouths. EMR/BLS 1. For any known or suspected bite, refer to Antivenin Bank Procedure 33. Evaluate for specific signs/symptoms: a) Distinct "fang marks" or puncture wounds. b) Swelling and pain at the site. c) Weakness, nausea, and vomiting. d) Paresthesia, fasciculations. e) Numbness and tingling around the face and head. f) Metallic taste, change in taste sensation. -

Epidemiology and Clinical Outcomes of Snakebite in the Elderly: a Toxic Database Study
Clinical Toxicology ISSN: 1556-3650 (Print) 1556-9519 (Online) Journal homepage: http://www.tandfonline.com/loi/ictx20 Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC database study Meghan B. Spyres, Anne-Michelle Ruha, Kurt Kleinschmidt, Rais Vohra, Eric Smith & Angela Padilla-Jones To cite this article: Meghan B. Spyres, Anne-Michelle Ruha, Kurt Kleinschmidt, Rais Vohra, Eric Smith & Angela Padilla-Jones (2018) Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC database study, Clinical Toxicology, 56:2, 108-112, DOI: 10.1080/15563650.2017.1342829 To link to this article: https://doi.org/10.1080/15563650.2017.1342829 Published online: 13 Jul 2017. Submit your article to this journal Article views: 120 View related articles View Crossmark data Full Terms & Conditions of access and use can be found at http://www.tandfonline.com/action/journalInformation?journalCode=ictx20 CLINICAL TOXICOLOGY, 2018 VOL. 56, NO. 2, 108–112 https://doi.org/10.1080/15563650.2017.1342829 CLINICAL RESEARCH Epidemiology and clinical outcomes of snakebite in the elderly: a ToxIC Ã database study Meghan B. Spyresa, Anne-Michelle Ruhab, Kurt Kleinschmidtc, Rais Vohrad, Eric Smithc and Angela Padilla-Jonesb aDepartment of Emergency Medicine, Division of Medical Toxicology, University of Southern California, Los Angeles, CA, USA; bDepartment of Medical Toxicology, Banner-University Medical Center Phoenix, Phoenix, AZ, USA; cDepartment of Emergency Medicine, Univesity of Texas Southwestern Medical Center, Dallas, TX, USA; dDepartment of Emergency Medicine, UCSF Fresno Medical Center, Fresno, CA, USA ABSTRACT ARTICLE HISTORY Introduction: Epidemiologic studies of snakebites in the United States report typical victims to be Received 23 February 2017 young men.