Summary of Product Characteristics
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Format (Sample) Dissertation
Providers’ Knowledge, Perceptions and Views of Prescribing Long-Acting Reversible Contraception to Adolescents in a Southwest Community Health Center Item Type text; Electronic Dissertation Authors Schafer, Stephanie Lynne Publisher The University of Arizona. Rights Copyright © is held by the author. Digital access to this material is made possible by the University Libraries, University of Arizona. Further transmission, reproduction or presentation (such as public display or performance) of protected items is prohibited except with permission of the author. Download date 02/10/2021 06:38:23 Link to Item http://hdl.handle.net/10150/626699 PROVIDERS’ KNOWLEDGE, PERCEPTIONS AND VIEWS OF PRESCRIBING LONG-ACTING REVERSIBLE CONTRACEPTION TO ADOLESCENTS IN A SOUTHWEST COMMUNITY HEALTH CENTER by Stephanie Lynne Schafer ________________________ Copyright © Stephanie Lynne Schafer 2017 A DNP Project Submitted to the Faculty of the COLLEGE OF NURSING In Partial Fulfillment of the Requirements For the Degree of DOCTOR OF NURSING PRACTICE In the Graduate College THE UNIVERSITY OF ARIZONA 2 0 1 7 2 3 STATEMENT BY AUTHOR This DNP Project has been submitted in partial fulfillment of requirements for an advanced degree at The University of Arizona and is deposited in the University Library to be made available to borrowers under rules of the Library. Brief quotations from this DNP Project are allowable without special permission, provided that accurate acknowledgment of source is made. Requests for permission for extended quotation from or reproduction of this manuscript in whole or in part may be granted by the head of the major department or the Dean of the Graduate College when in his or her judgment the proposed use of the material is in the interests of scholarship. -

Initial Proposed Smpc Plus Proposed Revisions
1. NAME OF THE MEDICINAL PRODUCT Leticia 28 150 micrograms/30 microgram film-coated tablet 2. QUALITATIVE AND QUANTITATIVE COMPOSITION 21 white or almost white film-coated tablets: Each film-coated tablet contains 150 micrograms desogestrel 30 micrograms ethinylestradiol. Excipient with known effect: 64.3 mg lactose (as lactose monohydrate). 7 green placebo (inactive) film-coated tablets: The tablet does not contain active substances. Excipients with known effect: 37.26 mg lactose anhydrous and 0.003 mg sunset yellow. For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Film-coated tablet. The active tablet is white, or almost white, round shaped, biconvex film-coated tablets of 6 mm diameter, with P8 sign on one side and RG sign on other side. The placebo tablet is green, round, biconvex film-coated tablet, diameter about 6 mm, without engraving. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Oral contraception The decision to prescribe Leticia 28 should take into consideration the individual woman’s current risk factors, particularly those for venous thromboembolism (VTE), and how the risk of VTE with Leticia 28 compares with other combined hormonal contraceptives (CHCs) (see sections 4.3 and 4.4). 4.2 Posology and method of administration Posology How to take Leticia 28 The tablets must be taken in the order directed on the package every day at about the same time of the day. Tablet taking is continuous. One tablet is taken daily for 28 consecutive days. Each subsequent pack is started after the last tablet of the previous pack. During the intake of the 7 placebo tablets bleeding usually occurs. -

Assessing the Availability, Service Quality, and Price of Essential Medicines In
Assessing the Availability, Service Quality, and Price of Essential Medicines in Private Pharmacies in Afghanistan Norio Kasahara A dissertation submitted in partial fulfillment of the requirements for the degree of Doctor of Philosophy University of Washington 2015 Reading Committee: Louis P. Garrison, Jr., Chair Joseph B. Babigumira Andy Stergachis Program Authorized to Offer Degree: Pharmaceutical Outcomes Research and Policy ©Copyright 2015 Norio Kasahara ii Table of Contents Abstract ................................................................................................................................................................................... ................................................................................................ ................................................................................................ .................................................................................. ............... vvv Acknowledgements ................................................................................................................................................................................... ................................................................................................ ................................................................................. ............ viiviivii Summary ................................................................................................................................................................................... ............................................................................................... -

Injectable Birth Control May Raise HIV Infection Risk by 40%
08 January 2018 Injectable birth control may raise HIV infection risk by 40% The intramuscular injectable contraceptive depot medroxyprogesterone acetate, or DMPA, may raise the risk for HIV infection by 40% in women, according to research published recently in Endocrine Reviews. Research indicates alternative contraception methods may help protect women. Professor Janet P. Hapgood, lead author of the review from the University of Cape Town’s (UCT) Department of Molecular and Cell Biology said: “To protect individual and public health, it is important to ensure women in areas with high rates of HIV infection have access to affordable and safe contraceptive options.” In the review, researchers noted that the injectable progestin contraceptive, DMPA, is the major form of hormonal contraceptive used in sub-Saharan Africa, which also has the highest worldwide HIV prevalence, particularly in young women. However, researchers also noted that DMPA may raise the risk for HIV infection by 40% in women. “The increased rate of HIV infection among women using DMPA contraceptive shots is likely due to multiple reasons, including decreases in immune function, and the protective barrier function of the female genital tract. Studying the biology of medroxyprogesterone acetate (MPA) helps us understand what may be driving the increased rate of HIV infection seen in human research,” remarked Hapgood. Increasing the availability of contraceptives that use a different form of progestin than the one found in DMPA could help reduce the risk of HIV transmission. Other forms of contraception, including combined oral contraceptives containing levonorgestrel or the injectable contraceptive norethisterone enanthate (NET-EN), were not associated with increased HIV infection risk. -
COMPARISON of the WHO ATC CLASSIFICATION & Ephmra/Intellus Worldwide ANATOMICAL CLASSIFICATION
COMPARISON OF THE WHO ATC CLASSIFICATION & EphMRA/Intellus Worldwide ANATOMICAL CLASSIFICATION: VERSION June 2019 2 Comparison of the WHO ATC Classification and EphMRA / Intellus Worldwide Anatomical Classification The following booklet is designed to improve the understanding of the two classification systems. The development of the two systems had previously taken place separately. EphMRA and WHO are now working together to ensure that there is a convergence of the 2 systems rather than a divergence. In order to better understand the two classification systems, we should pay attention to the way in which substances/products are classified. WHO mainly classifies substances according to the therapeutic or pharmaceutical aspects and in one class only (particular formulations or strengths can be given separate codes, e.g. clonidine in C02A as antihypertensive agent, N02C as anti-migraine product and S01E as ophthalmic product). EphMRA classifies products, mainly according to their indications and use. Therefore, it is possible to find the same compound in several classes, depending on the product, e.g., NAPROXEN tablets can be classified in M1A (antirheumatic), N2B (analgesic) and G2C if indicated for gynaecological conditions only. The purposes of classification are also different: The main purpose of the WHO classification is for international drug utilisation research and for adverse drug reaction monitoring. This classification is recommended by the WHO for use in international drug utilisation research. The EphMRA/Intellus Worldwide classification has a primary objective to satisfy the marketing needs of the pharmaceutical companies. Therefore, a direct comparison is sometimes difficult due to the different nature and purpose of the two systems. -

Innovative Practices Among Publicly Operated Family Planning Centers
Innovative Practices Among Publicly Operated Family Planning Centers COMPANION WORKBOOK Innovative Practices Among Publicly Operated Family Planning Centers COMPANION WORKBOOK Table of Contents CDPHE “Sustainability Coordinator” Job Description ................................................ 1 HCCMS Organizational History ............................................................................. 4 DHEC Regional Map ............................................................................................. 5 HCCMS Organizational Chart ............................................................................... 6 Sample Supply Requisition Sheet ............................................................................ 7 Sample Job Aid of Available Birth Control ............................................................... 9 Example Title X and FQHC Sliding Fee Scale ......................................................... 10 Example Guideline for Contraception ................................................................... 12 Example Contraception Wall Chart ....................................................................... 14 Example Clinical Guideline .................................................................................. 15 Sample Adolescent Services Policy ........................................................................ 17 South Carolina Campaign to Prevent Teen Pregnancy Mission Statement ........................................................................ 19 “One Key Question” Educational -
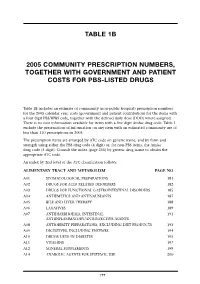
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

Variation in Serum Biomarkers with Sex and Female Hormonal Status: Implications for Clinical Tests Received: 11 February 2016 Jordan M
www.nature.com/scientificreports OPEN Variation in serum biomarkers with sex and female hormonal status: implications for clinical tests Received: 11 February 2016 Jordan M. Ramsey1, Jason D. Cooper1, Brenda W. J. H. Penninx2,* & Sabine Bahn1,3,* Accepted: 11 May 2016 Few serum biomarker tests are implemented in clinical practice and recent reports raise concerns Published: 31 May 2016 about poor reproducibility of biomarker studies. Here, we investigated the potential role of sex and female hormonal status in this widespread irreproducibility. We examined 171 serum proteins and small molecules measured in 1,676 participants from the Netherlands Study of Depression and Anxiety. Concentrations of 96 molecules varied with sex and 66 molecules varied between oral contraceptive pill users, postmenopausal females, and females in the follicular and luteal phases of the menstrual cycle (FDR-adjusted p-value <0.05). Simulations of biomarker studies yielded up to 40% false discoveries when patient and control groups were not matched for sex and up to 41% false discoveries when premenopausal females were not matched for oral contraceptive pill use. High accuracy (over 90%) classification tools were developed to label samples with sex and female hormonal status where this information was not collected. Serum proteomic biomarkers have enormous potential for early diagnosis, quantification of disease risk, prog- nosis, and treatment response prediction and monitoring. They have been investigated for autoimmune dis- ease and arthritis1,2, cancer3–5, cardiovascular disease6, mental and neurological disorders7–12, kidney function13, and other applications. Despite the increasing number of published serum biomarker studies (Supplementary Fig. 1), translation of these findings from the laboratory to clinical tools has proved challenging14,15. -

The Effects of Hormonal Contraception on the Voice: History of Its Evolution in the Literature
CARE OF THE PROFESSIONAL VOICE Robert T. Sataloff, Associate Editor The Effects of Hormonal Contraception on the Voice: History of its Evolution in the Literature Jennifer Rodney and Robert T. Sataloff [Modified from J. Rodney and R.T. Sataloff, “The Effects of Hormonal Contraception on the Voice: History of its Evolution in the Literature,” Journal of Voice 30, no. 6 (November 2016): 726–730; with permission.] INTRODUCTION: THE MENSTRUAL CYCLE AND THE VOICE The fluctuation of hormones in the menstrual cycle has significant effects on the voice.1 Singing teachers should be familiar with the vocal effects of Jennifer Rodney hormones and of hormonal medications such as oral contraceptives (birth control pills), especially in light of recent changes in their chemistry and effects. Vocal symptoms, known as dysphonia premenstrualis, accompany the better known symptoms of premenstrual syndrome (PMS) during the luteal phase of the menstrual cycle.2 The most common symptoms of dys- phonia premenstrualis are difficulty singing high notes, decreased flexibil- ity, huskiness, fuzziness, breathiness, decreased volume, difficulty bridging passaggios and intonation problems.3 Davis and Davis concluded that, on average, singers experience 33 general symptoms of PMS and 3 symptoms of dysphonia premenstrualis.4 Chae et al. showed that approximately 57% participants met the DSM IV criteria for PMS and also had acoustic evidence Robert T. Sataloff of dysphonia premenstrualis, whereas the PMS-negative group did not.5 The risk of vocal stress and possible damage during the premenstrual period led many European opera houses to offer singers contracts that included “grace days” during their premenstrual period. This accommodation is no longer followed in Europe and was never practiced generally in the United States.6 The mechanisms that cause these symptoms lie not just in the actions of the hormones themselves, but also in the cyclic fluctuation of hormone levels. -

Contraception in Adolescents – Regulatory Considerations”
“Contraception in adolescents – regulatory considerations” Wissenschaftliche Prüfungsarbeit zur Erlangung des Titels „Master of Drug Regulatory Affairs“ der Mathematisch-Naturwissenschaftlichen Fakultät der Rheinischen Friedrich-Wilhelms-Universität Bonn vorgelegt von Dr. Julian Paesler aus Münster Bonn 2016 Betreuerin und 1. Referentin: Frau Dr. Ingrid Klingmann Zweiter Referent: Herr Prof. Dr. Niels Eckstein Acknowledgements I would like to express my sincere gratitude to Dr. Ingrid Klingmann for her friendly willingness to function as my “supervising tutor” and for the support and the motivating feedback she gave me during the preparation of this master thesis. Her comments and constructive suggestions were very helpful to me. Besides Dr. Ingrid Klingmann, I would like to thank Prof. Dr. Niels Eckstein for his support and the willingness to function as my “secondary tutor”. Special thanks are also due to my mother, who was willing to proofread this master thesis. I am really thankful for all the support she gave - and still gives – to me, which is way more than what could ever be mentioned here. Table of Contents Table of Contents List of Figures .......................................................................................................................... I List of Tables ......................................................................................................................... III List of Abbreviations .............................................................................................................. -

Summary of Product Characteristics
SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Vellena 75 micrograms / 20 micrograms Coated tablets Vellena 75 micrograms / 30 micrograms Coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Active ingredients: Vellena: Each tablet contains 75 micrograms gestodene and 20 micrograms ethinylestradiol Vellena: Each tablet contains 75 micrograms gestodene and 30 micrograms ethinylestradiol Excipients with known effect: Vellena contains 38 mg lactose monohydrate and 20 mg sucrose For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Coated tablet. White, round, biconvex sugar coated tablets, both sides are without imprinting. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Oral contraception. The decision to prescribe Vellena should take into consideration the individual woman’s current risk factors, particularly those for venous thromboembolism (VTE), and how the risk of VTE with Vellena compares with other combined hormonal contraceptives (CHCs) (see sections 4.3 and 4.4) 4.2 Posology and method of administration How to take Vellena The tablets should be taken in the order indicated on the package, every day at approximately the same time. One tablet per day should be taken for 21 days. Each subsequent pack should be started after a 7-day tablet-free interval during which time a withdrawal bleeding will occur. This bleeding usually starts on the 2nd or 3rd day after taking the last tablet, and may not stop until the next pack is started. How to start taking Vellena If no preceding hormonal contraceptive use in the past month Taking of the tablets should begin on the first day of the woman’s natural cycle (i.e. -

Family Planning (Birth Control) By: Phd. Nuha Al-Wendawi 2018-2019
Family planning (Birth control) By: phD. Nuha Al-Wendawi 2018-2019 Maternal and Neonate Nursing Department b Objectives: To help the students identify methods of birth control and its benefits. Introduction There are a number of methods available to help prevent pregnancy, with some of the most popular including condoms and birth control pills. Deciding which method is right can be tough because there are many issues to consider, including costs, future pregnancy plans, side effects, and others. Family planning allows people to attain their desired number of children and determine the spacing of pregnancies. Benefits of family planning / contraception Promotion of family planning – and ensuring access to preferred contraceptive methods for women and couples . Contraceptive methods / Modern methods Effectiveness How it Method Description to prevent Comments works pregnancy Prevents >99% with Combined Contains two the release correct and Reduces risk oral hormones of eggs consistent use of endometrial contraceptives (estrogen and from the and ovarian (COCs) or 92% as progestogen) ovaries cancer “the pill” commonly (ovulation) used 99% with Thickens Can be used Progestogen- Contains only correct and cervical while only pills progestogen consistent use mucous to breastfeeding; Effectiveness How it Method Description to prevent Comments works pregnancy (POPs) or hormone, not block must be taken "the minipill" estrogen sperm and at the same egg from 90–97% as time each day meeting commonly and used prevents ovulation Health-care provider must