Initial Proposed Smpc Plus Proposed Revisions
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
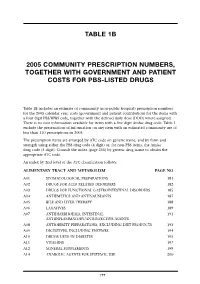
Table 1B 2005 Community Prescription Numbers, Together with Government
TABLE 1B 2005 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1B includes an estimate of community (non-public hospital) prescription numbers for the 2005 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 exclude the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2005. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit) or, for non-PBS items, the Amfac drug code (5 digit). Consult the index (page 255) by generic drug name to obtain the appropriate ATC code. An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 181 A02 DRUGS FOR ACID RELATED DISORDERS 182 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 185 A04 ANTIEMETICS AND ANTINAUSEANTS 187 A05 BILE AND LIVER THERAPY 188 A06 LAXATIVES 189 A07 ANTIDIARRHOEALS, INTESTINAL 191 ANTIINFLAMMATORY/ANTIINFECTIVE AGENTS A08 ANTIOBESITY PREPARATIONS, EXCLUDING DIET PRODUCTS 193 A09 DIGESTIVES, INCLUDING ENZYMES 194 A10 DRUGS USED IN DIABETES 195 A11 VITAMINS 197 A12 MINERAL SUPPLEMENTS 199 A14 ANABOLIC AGENTS FOR SYSTEMIC USE 200 177 BLOOD AND BLOOD FORMING ORGANS B01 ANTITHROMBOTIC AGENTS 201 B02 ANTIHAEMORRHAGICS 203 B03 -

Variation in Serum Biomarkers with Sex and Female Hormonal Status: Implications for Clinical Tests Received: 11 February 2016 Jordan M
www.nature.com/scientificreports OPEN Variation in serum biomarkers with sex and female hormonal status: implications for clinical tests Received: 11 February 2016 Jordan M. Ramsey1, Jason D. Cooper1, Brenda W. J. H. Penninx2,* & Sabine Bahn1,3,* Accepted: 11 May 2016 Few serum biomarker tests are implemented in clinical practice and recent reports raise concerns Published: 31 May 2016 about poor reproducibility of biomarker studies. Here, we investigated the potential role of sex and female hormonal status in this widespread irreproducibility. We examined 171 serum proteins and small molecules measured in 1,676 participants from the Netherlands Study of Depression and Anxiety. Concentrations of 96 molecules varied with sex and 66 molecules varied between oral contraceptive pill users, postmenopausal females, and females in the follicular and luteal phases of the menstrual cycle (FDR-adjusted p-value <0.05). Simulations of biomarker studies yielded up to 40% false discoveries when patient and control groups were not matched for sex and up to 41% false discoveries when premenopausal females were not matched for oral contraceptive pill use. High accuracy (over 90%) classification tools were developed to label samples with sex and female hormonal status where this information was not collected. Serum proteomic biomarkers have enormous potential for early diagnosis, quantification of disease risk, prog- nosis, and treatment response prediction and monitoring. They have been investigated for autoimmune dis- ease and arthritis1,2, cancer3–5, cardiovascular disease6, mental and neurological disorders7–12, kidney function13, and other applications. Despite the increasing number of published serum biomarker studies (Supplementary Fig. 1), translation of these findings from the laboratory to clinical tools has proved challenging14,15. -

Summary of Product Characteristics
SUMMARY OF PRODUCT CHARACTERISTICS 1 1. NAME OF THE MEDICINAL PRODUCT Vellena 75 micrograms / 20 micrograms Coated tablets Vellena 75 micrograms / 30 micrograms Coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Active ingredients: Vellena: Each tablet contains 75 micrograms gestodene and 20 micrograms ethinylestradiol Vellena: Each tablet contains 75 micrograms gestodene and 30 micrograms ethinylestradiol Excipients with known effect: Vellena contains 38 mg lactose monohydrate and 20 mg sucrose For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Coated tablet. White, round, biconvex sugar coated tablets, both sides are without imprinting. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Oral contraception. The decision to prescribe Vellena should take into consideration the individual woman’s current risk factors, particularly those for venous thromboembolism (VTE), and how the risk of VTE with Vellena compares with other combined hormonal contraceptives (CHCs) (see sections 4.3 and 4.4) 4.2 Posology and method of administration How to take Vellena The tablets should be taken in the order indicated on the package, every day at approximately the same time. One tablet per day should be taken for 21 days. Each subsequent pack should be started after a 7-day tablet-free interval during which time a withdrawal bleeding will occur. This bleeding usually starts on the 2nd or 3rd day after taking the last tablet, and may not stop until the next pack is started. How to start taking Vellena If no preceding hormonal contraceptive use in the past month Taking of the tablets should begin on the first day of the woman’s natural cycle (i.e. -

NON-INTERVENTIONAL STUDY REPORT 12 March 2020
B2311061 FINAL NON-INTERVENTIONAL STUDY REPORT 12 March 2020 NON-INTERVENTIONAL (NI) STUDY REPORT PASS information Title Drug Utilization Study of conjugated oestrogens/ bazedoxifene (CE/BZA) in the European Union (EU) Protocol number B2311061 Version identifier of the final study report Final Report Version 1.0 Date 12 March 2020 EU Post Authorisation Study (PAS) EUPAS 11604 register number Active substance Conjugated oestrogens/bazedoxifene (CE/BZA) Medicinal product DUAVIVE® modified-release tablets Product reference EU MA number: EU/1/14/960/001 (EU marketing authorisation granted 16 December 2014) Procedure number EMEA/H/C/002314/MEA 003 Marketing Authorisation Holder (MAH) Pfizer Europe MA EEIG Joint PASS No Research question and objectives Describe baseline characteristics and utilization patterns of EU patients initiating Duavive or oestrogen + progestin (E+P) combination hormone replacement therapy (HRT). Country(-ies) of study All EU countries where CE/BZA was commercially available in 2016-2018 and where adequate data sources are available: Belgium, France, Italy, the Netherlands, Spain and UK. 090177e19308d210\Approved\Approved On: 13-Mar-2020 10:57 (GMT) PFIZER CONFIDENTIAL Page 1 of 210 Page 1 B2311061 FINAL NON-INTERVENTIONAL STUDY REPORT 12 March 2020 Author Margarita Shlaen, MPH Dorothea von Bredow, PhD IQVIA Commercial GmbH & Co. OHG Landshuter Allee 10 D-80637 Munich Germany 090177e19308d210\Approved\Approved On: 13-Mar-2020 10:57 (GMT) PFIZER CONFIDENTIAL Page 2 of 210 Page 2 B2311061 FINAL NON-INTERVENTIONAL STUDY REPORT 12 March 2020 Marketing Authorisation Holder(s) Marketing Authorisation Holder(s) Pfizer Europe MA EEIG Boulevard de la Plaine 17 1050 Bruxelles Belgium MAH contact person Vera Frajzyngier, PhD, MPH Director, Safety Surveillance and Research Pfizer P: 001-212-733-5942 Email: [email protected] This document contains confidential information belonging to Pfizer. -

Table 1 2008 Community Prescription Numbers
TABLE 1 2008 COMMUNITY PRESCRIPTION NUMBERS, TOGETHER WITH GOVERNMENT AND PATIENT COSTS FOR PBS-LISTED DRUGS Table 1 includes an estimate of community prescription numbers for the 2008 calendar year, costs (government and patient contribution) for the items with a four digit PBS/RPBS code, together with the defined daily dose (DDD) where assigned. There is no cost information available for items with a five digit Amfac drug code. Table 1 excludes the presentation of information on any item with an estimated community use of less than 110 prescriptions in 2008. The prescription items are arranged by ATC code on generic name, and by form and strength using either the PBS drug code (4 digit plus alpha) or, for non-PBS items, the Amfac drug code (5 digit). Note that in this edition, “Item type” has been added to distinguish between PBS drug code and non-PBS drug code, for instance, P refers to PBS drug code and A refers to Amfac drug code. Note that Anatomical Therapeutic Chemical (ATC) classification index with Defined Daily Doses (DDDs) 2009 is used in all statistics published in this edition (refer to WHO collaborating Centre for Drug Statistics Methodology, ATC classification index with DDDs 2009). An index by 2nd level of the ATC classification follows: ALIMENTARY TRACT AND METABOLISM PAGE NO A01 STOMATOLOGICAL PREPARATIONS 41 A02 DRUGS FOR ACID RELATED DISORDERS 42 A03 DRUGS FOR FUNCTIONAL GASTROINTESTINAL DISORDERS 44 A04 ANTIEMETICS AND ANTINAUSEANTS 45 A05 BILE AND LIVER THERAPY 46 A06 LAXATIVES 47 A07 ANTIDIARRHOEALS, INTESTINAL -

Reseptregisteret 2014–2018 the Norwegian Prescription Database 2014–2018
LEGEMIDDELSTATISTIKK 2019:2 Reseptregisteret 2014–2018 The Norwegian Prescription Database 2014–2018 Reseptregisteret 2014–2018 The Norwegian Prescription Database 2014–2018 Christian Lie Berg Kristine Olsen Solveig Sakshaug Utgitt av Folkehelseinstituttet / Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2019 Tittel/Title: Legemiddelstatistikk 2019:2 Reseptregisteret 2014–2018 / The Norwegian Prescription Database 2014–2018 Forfattere/Authors: Christian Berg, redaktør/editor Kristine Olsen Solveig Sakshaug Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no / The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon / Contact information: Folkehelseinstituttet / Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8406-014-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2014–2018 [The Norwegian Prescription Database 2014–2018] Legemiddelstatistikk 2019:2, Oslo, Norge: Folkehelseinstituttet, 2019. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian -

Trinovum Tabletten Stand: 08.2012
Fachinformation TriNovum Tabletten Stand: 08.2012 1. BEZEICHNUNG DES ARZNEIMITTELS wieder aufgenommen und zwar unabhängig Einnahme von TriNovum am Tag nach dem TriNovum Tabletten vom Einsetzen und der Dauer der Entzugsblu- üblichen Ring- bzw. Pflaster-freien Intervall tung. begonnen werden. 2. QUALITATIVE UND QUANTITATIVE ZU- Beim ersten Anwendungszyklus sollte die Wechsel von einem Gestagenmonopräparat SAMMENSETZUNG Einnahme am ersten Tag der Menstruation (Minipille, Injektionspräparat, Implantat): Norethisteron und Ethinylestradiol beginnen. Bei einem Wechsel von einem oralen Kontra- 1 Zykluspackung enthält 7 weiße, 7 hellrosa Bei vorschriftsmäßiger Einnahme von zeptivum, das nur ein Gestagen enthält („Mi- und 7 rosa Tabletten TriNovum besteht ab dem ersten Tag der nipille“), auf TriNovum, muss mit TriNovum Einnahme ein sicherer Konzeptionsschutz, direkt im Anschluss an die letzte Minipille 1 weiße Tablette enthält: auch während der 7-tägigen Einnahmepause. begonnen werden. Die Umstellung von einem 0,50 mg Norethisteron Implantat muss am Tag des Entfernens und 0,035 mg Ethinylestradiol 4.2.2 Kinder und Jugendliche von einem Injektionspräparat zu dem Zeit- 1 hellrosa Tablette enthält: Die Sicherheit und Verträglichkeit von punkt erfolgen, an dem die nächste Injekti- 0,75 mg Norethisteron TriNovum Tabletten wurde für Frauen im on fällig wäre. In jedem Fall ist während der 0,035 mg Ethinylestradiol reproduktiven Alter ermittelt. Die pubertäre ersten 7 Tage der Einnahme von TriNovum 1 rosa Tablette enthält: Entwicklung in den ersten Jahren -

The Selection and Use of Essential Medicines
This report contains the collective views of an international group of experts and does not necessarily represent the decisions or the stated policy of the World Health Organization WHO Technical Report Series 933 THE SELECTION AND USE OF ESSENTIAL MEDICINES Report of the WHO Expert Committee, 2005 (including the 14th Model List of Essential Medicines) World Health Organization Geneva 2006 i WHO Library Cataloguing-in-Publication Data WHO Expert Committee on the Selection and Use of Essential Medicines (14th : 2005: Geneva, Switzerland) The selection and use of essential medicines : report of the WHO Expert Committee, 2005 : (including the 14th model list of essential medicines). (WHO technical report series ; 933) 1.Essential drugs — standards 2.Formularies — standards 3.Drug information services — organization and administration 4.Drug utilization 5. Pharmaceutical preparations — classification 6.Guidelines I.Title II.Title: 14th model list of essential medicines III.Series. ISBN 92 4 120933 X (LC/NLM classification: QV 55) ISSN 0512-3054 © World Health Organization 2006 All rights reserved. Publications of the World Health Organization can be obtained from WHO Press, World Health Organization, 20 Avenue Appia, 1211 Geneva 27, Switzerland (tel.: +41 22 791 2476; fax: +41 22 791 4857; email: [email protected]). Requests for permission to reproduce or translate WHO publica- tions — whether for sale or for noncommercial distribution — should be addressed to WHO Press, at the above address (fax: +41 22 791 4806; email: [email protected]). The designations employed and the presentation of the material in this publication do not imply the expression of any opinion whatsoever on the part of the World Health Organization concerning the legal status of any country, territory, city or area or of its authorities, or concerning the delimitation of its frontiers or boundaries. -

DK/H/0926/01-02/DC, Gestinyl 20/75 and 30/75, Ethinylestradiol
SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Gestinyl 20 20 micrograms / 75 micrograms Coated tablets Gestinyl 30 30 micrograms / 75 micrograms Coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Active ingredients: Gestinyl 20: Each tablet contains 20 micrograms ethinylestradiol and 75 micrograms gestodene Gestinyl 30: Each tablet contains 30 micrograms ethinylestradiol and 75 micrograms gestodene Excipients with known effect: Gestinyl 20 contains 38 mg lactose monohydrate and 20 mg sucrose Gestinyl 30 contains 38 mg lactose monohydrate and 20 mg sucrose For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Coated tablet. White, round, biconvex sugar coated tablets, both sides are without imprinting. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Oral contraception. The decision to prescribe Gestinyl 20 and Gestinyl 30 should take into consideration the individual woman’s current risk factors, particularly those for venous thromboembolism (VTE), and how the risk of VTE with Gestinyl 20 and Gestinyl 30 compares with other Combined Hormonal Contraceptives, CHCs (see sections 4.3 and 4.4). 4.2 Posology and method of administration How to take Gestinyl 20 and Gestinyl 30 The tablets should be taken in the order indicated on the package, every day at approximately the same time. One tablet per day should be taken for 21 days. Each subsequent pack should be started after a 7-day tablet-free interval during which time a withdrawal bleeding will occur. This bleeding usually starts on the 2nd or 3rd day after taking the last tablet, and may not stop until the next pack is started. -

ICCB-L Plate (10 Mm / 3.33 Mm) ICCB-L Well Vendor ID Chemical Name
ICCB-L Plate ICCB-L Therapeutic Absorption Protein FDA Additional info Additional info Vendor_ID Chemical_Name CAS number Therapeutic class Target type Target names (10 mM / 3.33 mM) Well effect tissue binding approved type detail Pharmacological 3712 / 3716 A03 Prestw-1 Azaguanine-8 134-58-7 Oncology Antineoplastic tool 3712 / 3716 A05 Prestw-2 Allantoin 97-59-6 Dermatology Antipsoriatic Carbonic 3712 / 3716 A07 Prestw-3 Acetazolamide 59-66-5 Metabolism Anticonvulsant Enzyme Carbonic anhydrase GI tract Yes anhydrase Potential Plasmatic New therapeutic 3712 / 3716 A09 Prestw-4 Metformin hydrochloride 1115-70-4 Endocrinology Anorectic GI tract Yes anticancer proteins use agent Chemical Plasmatic classification Quaternary 3712 / 3716 A11 Prestw-5 Atracurium besylate 64228-81-5 Neuromuscular Curarizing Yes proteins (according ATC ammonium code) 3712 / 3716 A13 Prestw-6 Isoflupredone acetate 338-98-7 Endocrinology Anti-inflammatory Therapeutic Amiloride-sensitive classification Potassium- 3712 / 3716 A15 Prestw-7 Amiloride hydrochloride dihydrate 17440-83-4 Metabolism Antihypertensive LGIC GI tract Yes sodium channel, ENaC (according ATC sparing agent code) 3712 / 3716 A17 Prestw-8 Amprolium hydrochloride 137-88-2 Infectiology Anticoccidial Veterinary use Poultry Therapeutic Solute carrier family 12 Plasmatic classification Low-ceiling 3712 / 3716 A19 Prestw-9 Hydrochlorothiazide 58-93-5 Metabolism Antihypertensive Carrier GI tract Yes member 3 proteins (according ATC diuretic code) Chemical classification 3712 / 3716 A21 Prestw-10 Sulfaguanidine -

Gestodene/Ethinylestradiol, Coated Tablets, DK/H/1148/001-002, 12.11.2018
Gestodene/Ethinylestradiol, coated tablets, DK/H/1148/001-002, 12.11.2018 SUMMARY OF PRODUCT CHARACTERISTICS 1. NAME OF THE MEDICINAL PRODUCT Vellena 75 micrograms / 20 micrograms Coated tablets Vellena 75 micrograms / 30 micrograms Coated tablets 2. QUALITATIVE AND QUANTITATIVE COMPOSITION Active ingredients: Vellena: Each tablet contains 75 micrograms gestodene and 20 micrograms ethinylestradiol Vellena: Each tablet contains 75 micrograms gestodene and 30 micrograms ethinylestradiol Excipients with known effect: Vellena contains 38 mg lactose monohydrate and 20 mg sucrose For the full list of excipients, see section 6.1. 3. PHARMACEUTICAL FORM Coated tablet. White, round, biconvex sugar coated tablets, both sides are without imprinting. 4. CLINICAL PARTICULARS 4.1 Therapeutic indications Oral contraception. The decision to prescribe Vellena should take into consideration the individual woman’s current risk factors, particularly those for venous thromboembolism (VTE), and how the risk of VTE with Vellena compares with other combined hormonal contraceptives (CHCs) (see sections 4.3 and 4.4) 4.2 Posology and method of administration How to take Vellena The tablets should be taken in the order indicated on the package, every day at approximately the same time. One tablet per day should be taken for 21 days. Each subsequent pack should be started after a 7-day tablet-free interval during which time a withdrawal bleeding will occur. This bleeding usually starts on the 2nd or 3rd day after taking the last tablet, and may not stop until the next pack is started. How to start taking Vellena If no preceding hormonal contraceptive use in the past month Taking of the tablets should begin on the first day of the woman’s natural cycle (i.e. -

Evaluation of Carcinogenicity Studies of Medicinal Products for Human Use Authorised Via the European Centralised Procedure
Regulatory Toxicology and Pharmacology xxx (2011) xxx–xxx Contents lists available at ScienceDirect Regulatory Toxicology and Pharmacology journal homepage: www.elsevier.com/locate/yrtph Evaluation of carcinogenicity studies of medicinal products for human use authorised via the European centralised procedure (1995–2009) ⇑ Anita Friedrich a, , Klaus Olejniczak b a Granzer Regulatory Consulting and Services, Zielstattstrasse 44, 81379 Munich, Germany b Federal Institute for Drugs and Medical Devices, Kurt-Georg-Kiesinger-Allee 3, 53175 Bonn, Germany article info abstract Article history: Carcinogenicity data of medicinal products for human use that have been authorised via the European Received 25 October 2010 centralised procedure (CP) between 1995 and 2009 were evaluated. Carcinogenicity data, either from Available online xxxx long-term rodent carcinogenicity studies, transgenic mouse studies or repeat-dose toxicity studies were available for 144 active substances contained in 159 medicinal products. Out of these compounds, 94 Keywords: (65%) were positive in at least one long-term carcinogenicity study or in repeat-dose toxicity studies. Medicinal products Fifty compounds (35%) showed no evidence of a carcinogenic potential. Out of the 94 compounds with Carcinogenicity positive findings in either carcinogenicity or repeat-dose toxicity studies, 33 were positive in both mice Rodents and rats, 40 were positive in rats only, and 21 were positive exclusively in mice. Long-term carcinogenic- ity studies in two rodent species were available for 116 compounds. Data from one long-term carcinoge- nicity study in rats and a transgenic mouse model were available for eight compounds. For 13 compounds, carcinogenicity data were generated in only one rodent species. One compound was exclu- sively tested in a transgenic mouse model.