Evaluating the Importance of the Carotid Chemoreceptors in Controlling Breathing During Exercise in Man
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Download This PDF File
doi: http://dx.doi.org/10.5016/1806-8774.2009v11pT1 ARBS Annual Review of Biomedical Sciences Theme Topic on “Cell Receptors and Signaling” pdf freely available at http://arbs.biblioteca.unesp.br 2009;11:T1-T50 Story of Muscarinic Receptors, Alkaloids with Muscarinic Significance and of Muscarinic Functions and Behaviors Alexander G Karczmar* Research Service, Edward J. Hines VA Hospital and Department of Pharmacology, Loyola U. Medical Center, IL, USA Received: 23 October 2009; accepted 22 December 2009 Online on 21 February 2010 .Abstract Karczmar AG.. Story of Muscarinic Receptors, Alkaloids with Muscarinic Significance and of Muscarinic Functions and Behaviors. Annu Rev Biomed Sci 2009;11:T1-T50. This review of the studies of the muscarinic receptors, their synaptic activities and their functional and behavioral roles will begin with the history of the research of the autonomic and central nervous systems and their transmitters, the development of the notion of the receptor, and the tale of the significance of muscarine and other alkaloids as well as of organophosphorus (OP) anticholinesterases for these studies; we will then segue into the modern status of muscarinic receptors and of their functional and behavioral expression. © by São Paulo State University – ISSN 1806-8774 Keywords: muscarinic, cholinesterase, cholinergic, nicotinic, curare, atropine, behavior Table of Contents 1. Early Story of the Autonomic and Central Nervous System 2. The Early Story of Pharmacologically Active Alkaloids and of OP AntiChEs 3. From Gaskell’s and Langley’s Definition of Autonomic Nervous System to Loewi’s Demonstration of Peripheral Chemical, Cholinergic Transmission 4. Eccles’s Demonstration of Central Chemical, Cholinergic Transmission and Immediate Post-Ecclessian Studies of Central Nicotinic and Muscarinic Transmission 5. -
Curt Von Euler 528
EDITORIAL ADVISORY COMMITTEE Albert J. Aguayo Bernice Grafstein Theodore Melnechuk Dale Purves Gordon M. Shepherd Larry W. Swanson (Chairperson) The History of Neuroscience in Autobiography VOLUME 1 Edited by Larry R. Squire SOCIETY FOR NEUROSCIENCE 1996 Washington, D.C. Society for Neuroscience 1121 14th Street, NW., Suite 1010 Washington, D.C. 20005 © 1996 by the Society for Neuroscience. All rights reserved. Printed in the United States of America. Library of Congress Catalog Card Number 96-70950 ISBN 0-916110-51-6 Contents Denise Albe-Fessard 2 Julius Axelrod 50 Peter O. Bishop 80 Theodore H. Bullock 110 Irving T. Diamond 158 Robert Galambos 178 Viktor Hamburger 222 Sir Alan L. Hodgkin 252 David H. Hubel 294 Herbert H. Jasper 318 Sir Bernard Katz 348 Seymour S. Kety 382 Benjamin Libet 414 Louis Sokoloff 454 James M. Sprague 498 Curt von Euler 528 John Z. Young 554 Curt von Euler BORN: Stockholm County, Sweden October 22, 1918 EDUCATION: Karolinska Institute, B.M., 1940 Karolinska Institute, M.D., 1945 Karolinska Institute, Ph.D., 1947 APPOINTMENTS: Karolinska Institute (1948) Professor Emeritus, Karolinska Institute (1985) HONORS AND AWARDS (SELECTED): Norwegian Academy of Sciences (foreign member) Curt von Euler conducted pioneering work on the central control of motor systems, brain mechanisms of thermoregulation, and on neural systems that control respiration. Curt von Euler Background ow did I come to devote my life to neurophysiology rather than to a clinical discipline? Why, in the first place, did I choose to study H medicine rather than another branch of biology or other subjects within the natural sciences? And what guided me to make the turns on the road and follow what appeared to be bypaths? There are no simple answers to such questions, but certainly a number of accidental circum- stances have intervened in important ways. -

Contributions of Civilizations to International Prizes
CONTRIBUTIONS OF CIVILIZATIONS TO INTERNATIONAL PRIZES Split of Nobel prizes and Fields medals by civilization : PHYSICS .......................................................................................................................................................................... 1 CHEMISTRY .................................................................................................................................................................... 2 PHYSIOLOGY / MEDECINE .............................................................................................................................................. 3 LITERATURE ................................................................................................................................................................... 4 ECONOMY ...................................................................................................................................................................... 5 MATHEMATICS (Fields) .................................................................................................................................................. 5 PHYSICS Occidental / Judeo-christian (198) Alekseï Abrikossov / Zhores Alferov / Hannes Alfvén / Eric Allin Cornell / Luis Walter Alvarez / Carl David Anderson / Philip Warren Anderson / EdWard Victor Appleton / ArthUr Ashkin / John Bardeen / Barry C. Barish / Nikolay Basov / Henri BecqUerel / Johannes Georg Bednorz / Hans Bethe / Gerd Binnig / Patrick Blackett / Felix Bloch / Nicolaas Bloembergen -

List of Nobel Laureates 1
List of Nobel laureates 1 List of Nobel laureates The Nobel Prizes (Swedish: Nobelpriset, Norwegian: Nobelprisen) are awarded annually by the Royal Swedish Academy of Sciences, the Swedish Academy, the Karolinska Institute, and the Norwegian Nobel Committee to individuals and organizations who make outstanding contributions in the fields of chemistry, physics, literature, peace, and physiology or medicine.[1] They were established by the 1895 will of Alfred Nobel, which dictates that the awards should be administered by the Nobel Foundation. Another prize, the Nobel Memorial Prize in Economic Sciences, was established in 1968 by the Sveriges Riksbank, the central bank of Sweden, for contributors to the field of economics.[2] Each prize is awarded by a separate committee; the Royal Swedish Academy of Sciences awards the Prizes in Physics, Chemistry, and Economics, the Karolinska Institute awards the Prize in Physiology or Medicine, and the Norwegian Nobel Committee awards the Prize in Peace.[3] Each recipient receives a medal, a diploma and a monetary award that has varied throughout the years.[2] In 1901, the recipients of the first Nobel Prizes were given 150,782 SEK, which is equal to 7,731,004 SEK in December 2007. In 2008, the winners were awarded a prize amount of 10,000,000 SEK.[4] The awards are presented in Stockholm in an annual ceremony on December 10, the anniversary of Nobel's death.[5] As of 2011, 826 individuals and 20 organizations have been awarded a Nobel Prize, including 69 winners of the Nobel Memorial Prize in Economic Sciences.[6] Four Nobel laureates were not permitted by their governments to accept the Nobel Prize. -

Physiology News
PN Issue 107 / Summer 2017 Physiology News Open science movement The war to liberate knowledge Future Physiology 13 - 14 December 2017 Leeds, UK A two-day scientific and career development conference organised by early career physiologists. www.physoc.org/futurephysiology Physiology News Editor Roger Thomas We welcome feedback on our membership magazine, or letters and suggestions for (University of Cambridge) articles for publication, including book reviews, from our Members. Editorial Board Please email [email protected] Karen Doyle (NUI Galway) Physiology News is one of the benefits of membership, along with reduced registration rates Rachel McCormick for our high-profile events, free online access to our leading journals,The Journal of Physiology, (University of Liverpool) Experimental Physiology and Physiological Reports, and travel grants to attend scientific Graham Dockray meetings. Membership offers you access to the largest network of physiologists in Europe. (University of Liverpool) Keith Siew Join now to support your career in physiology: (University of Cambridge) Visit www.physoc.org/membership or call 0207 269 5721 Austin Elliott (University of Manchester) Mark Dallas (University of Reading) Membership Fees for 2017 FEES Fiona Hatch Fellow £120 (Cello Health Communications iScience, Medical writer) Member £90 Managing Editor Retired Member – Julia Turan YOUTUBE LOGO SPECS Affiliate £40 [email protected] PRINT on light backgrounds on dark backgrounds Associate £30 standard standard main red gradient bottom PMS 1795C PMS 1815C www.physoc.org C0 M96 Y90 K2 C13 M96 Y81 K54 Undergraduate – white black WHITE BLACK no gradients no gradients C100 M100 Y100 K100 @ThePhySoc C0 M0 Y0 K0 Opinions expressed in articles and letters submitted by, or commissioned from, Members, Affiliates or outside bodies /physoc are not necessarily those of The Physiological Society. -

Image-Brochure-LNLM-2020-LQ.Pdf
NOBEL LAUREATES PARTICIPATING IN LINDAU EVENTS SINCE 1951 Peter Agre | George A. Akerlof | Kurt Alder | Zhores I. Alferov | Hannes Alfvén | Sidney Altman | Hiroshi Amano | Philip W. Anderson | Christian B. Anfinsen | Edward V. Appleton | Werner Arber | Frances H. Arnold | Robert J. Aumann | Julius Axelrod | Abhijit Banerjee | John Bardeen | Barry C. Barish | Françoise Barré-Sinoussi | Derek H. R. Barton | Nicolay G. Basov | George W. Beadle | J. Georg Bednorz | Georg von Békésy |Eric Betzig | Bruce A. Beutler | Gerd Binnig | J. Michael Bishop | James W. Black | Elizabeth H. Blackburn | Patrick M. S. Blackett | Günter Blobel | Konrad Bloch | Felix Bloch | Nicolaas Bloembergen | Baruch S. Blumberg | Niels Bohr | Max Born | Paul Boyer | William Lawrence Bragg | Willy Brandt | Walter H. Brattain | Bertram N. Brockhouse | Herbert C. Brown | James M. Buchanan Jr. | Frank Burnet | Adolf F. Butenandt | Melvin Calvin Thomas R. Cech | Martin Chalfie | Subrahmanyan Chandrasekhar | Pavel A. Cherenkov | Steven Chu | Aaron Ciechanover | Albert Claude | John Cockcroft | Claude Cohen- Tannoudji | Leon N. Cooper | Carl Cori | Allan M. Cormack | John Cornforth André F. Cournand | Francis Crick | James Cronin | Paul J. Crutzen | Robert F. Curl Jr. | Henrik Dam | Jean Dausset | Angus S. Deaton | Gérard Debreu | Petrus Debye | Hans G. Dehmelt | Johann Deisenhofer Peter A. Diamond | Paul A. M. Dirac | Peter C. Doherty | Gerhard Domagk | Esther Duflo | Renato Dulbecco | Christian de Duve John Eccles | Gerald M. Edelman | Manfred Eigen | Gertrude B. Elion | Robert F. Engle III | François Englert | Richard R. Ernst Gerhard Ertl | Leo Esaki | Ulf von Euler | Hans von Euler- Chelpin | Martin J. Evans | John B. Fenn | Bernard L. Feringa Albert Fert | Ernst O. Fischer | Edmond H. Fischer | Val Fitch | Paul J. -

Nobel Prizes List from 1901
Nature and Science, 4(3), 2006, Ma, Nobel Prizes Nobel Prizes from 1901 Ma Hongbao East Lansing, Michigan, USA, Email: [email protected] The Nobel Prizes were set up by the final will of Alfred Nobel, a Swedish chemist, industrialist, and the inventor of dynamite on November 27, 1895 at the Swedish-Norwegian Club in Paris, which are awarding to people and organizations who have done outstanding research, invented groundbreaking techniques or equipment, or made outstanding contributions to society. The Nobel Prizes are generally awarded annually in the categories as following: 1. Chemistry, decided by the Royal Swedish Academy of Sciences 2. Economics, decided by the Royal Swedish Academy of Sciences 3. Literature, decided by the Swedish Academy 4. Peace, decided by the Norwegian Nobel Committee, appointed by the Norwegian Parliament, Stortinget 5. Physics, decided by the Royal Swedish Academy of Sciences 6. Physiology or Medicine, decided by Karolinska Institutet Nobel Prizes are widely regarded as the highest prize in the world today. As of November 2005, a total of 776 Nobel Prizes have been awarded, 758 to individuals and 18 to organizations. [Nature and Science. 2006;4(3):86- 94]. I. List of All Nobel Prize Winners (1901 – 2005): 31. Physics, Philipp Lenard 32. 1906 - Chemistry, Henri Moissan 1. 1901 - Chemistry, Jacobus H. van 't Hoff 33. Literature, Giosuè Carducci 2. Literature, Sully Prudhomme 34. Medicine, Camillo Golgi 3. Medicine, Emil von Behring 35. Medicine, Santiago Ramón y Cajal 4. Peace, Henry Dunant 36. Peace, Theodore Roosevelt 5. Peace, Frédéric Passy 37. Physics, J.J. Thomson 6. Physics, Wilhelm Conrad Röntgen 38. -

En 1904: En 1905: En 1907
Le prix Nobel de physiologie ou de méde- cine a été décerné en 1901: @ EMIL von BEHRING, pour ses travaux sur la strothérapie et spécialement son emplot contre la aiphtérve; en 1902: & RONALD ROSS , pour ses travaux sur lamataria; en 1903: a@ NIELS R. FINSEN, en reconnaissance de ses travaux pour le trattement des maladies et Spéctalement du lupus (lupus vulgaris) & laide de rayons luminenx concentrés ; en 1904: a@ IVAN PETROVITCH PAVLOV, pour ses travaux sur la phystologte de la digestion; en 1905: a@ ROBERT KOCH, pour ses travaux sur la tuberculose,; en 1906: motte & CAMILLO GOLGI et moitit 2 SANTI- AGO RAMON VY CAFAL, pour leurs travaux sur Lanatomie du systeme nerveux; en 1907: a C.L. ALPHONSE LAVERAN, pour ses travaux suv Limportance des protozoatres dans la natssance des maladies; en 1908: motte & PAUL EHRLICH et moitié &@ ELIE METCHNIKOFF pour leurs travaux sur Cimmuntte; en 1909: 3 THEODORE KOCHER, pour ses travaux sur la phystologie, la pathologie et la chirurgie de la glande thyrotde; en 1910: 3) ALBRECHT KOSSEL, pour ses travaux sur les matieres protéiques, conpris les substances nuclétgues , a en IQII: 3 ALLVAR GULLSTRAND, pour ses travaux sur la adioptrigue de Vat; en 1912: g ALEXIS CARREL, pour ses travaux sur la suture des vaisseaux et sur la transplantation des Vatsseaux et des organes; en 1913: 3 CHARLES RICHET, pour ses travaux sur Lanaphylaxte; en IQI4: & ROBERT BARANY, pour ses travaux sur la phystologte et la pathologie de Pappareil vestibulatre; en I9I5—I9I8: le prix wa pas bté distribue; en 1919: a FULES BORDET, pour ses découvertes con- cernant Cimmunite; en 1920: a@ AUGUST KROGH, pour sa découverte du mécanisme captllatromotenr, réglant la mnutriteon des Zissus; en 1921: le prix n'a pas &té adistribué; en 1922: mottté & A. -

BMA Journal Make January 2010.Pmd
Bangladesh Medical Journal 2010; 39(1): 49-51 The Nobel Prize The Nobel Prize is an international award • 1994 - Alfred G. Gilman, Martin Rodbell administered by the Nobel Foundation in Stockholm, • 1993 - Richard J. Roberts, Phillip A. Sharp Sweden. In 1968, Sveriges Riksbank established The • 1992 - Edmond H. Fischer, Edwin G. Krebs Sveriges Riksbank Prize in Economic Sciences in • 1991 - Erwin Neher, Bert Sakmann Memory of Alfred Nobel, founder of the Nobel Prize. • 1990 - Joseph E. Murray, E. Donnall Thomas Each prize consists of a medal, personal diploma, and • 1989 - J. Michael Bishop, Harold E. Varmus a cash award. Every year since 1901, the Nobel Prize • 1988 - Sir James W. Black, Gertrude B. Elion, George H. Hitchings has been awarded for achievements in physics, • 1987 - Susumu Tonegawa chemistry, physiology or medicine, literature and for • 1986 - Stanley Cohen, Rita Levi-Montalcini peace. • 1985 - Michael S. Brown, Joseph L. Goldstein • 1984 - Niels K. Jerne, Georges J.F. Köhler, César Milstein • 1983 - Barbara McClintock • 198 - Sune K. Bergström, Bengt I. Samuelsson, John R. Vane • 1981 - Roger W. Sperry, David H. Hubel, Torsten N. Wiesel • 1980 - Baruj Benacerraf, Jean Dausset, George D. Snell • 1979 - Allan M. Cormack, Godfrey N. Hounsfield • 1978 - Werner Arber, Daniel Nathans, Hamilton O. Smith All Nobel Laureates in Medicine • 1977 - Roger Guillemin, Andrew V. Schally, Rosalyn The Nobel Prize in Physiology or Medicine has been Yalow • 1976 - Baruch S. Blumberg, D. Carleton Gajdusek awarded 100 times to 195 Nobel Laureates between • 1975 - David Baltimore, Renato Dulbecco, Howard M. 1901 and 2009. Temin • 2009 - Elizabeth H. Blackburn, Carol W. Greider, Jack • 1974 - Albert Claude, Christian de Duve, George E. -

The Science Behind the Nobel Prizes in Medicine and Chemistry Is The
FRONTIER A MAGAZINE ABOUT ALLIGATOR BIOSCIENCE AND IMMUNO-ONCOLOGY #2, 2018 The science behind the Nobel Prizes in Medicine and Chemistry is the core in Alligator’s research and development FRONTIER – A MAGAZINE ABOUT ALLIGATOR BIOSCIENCE AND IMMUNO-ONCOLOGY The Nobel Prize in Physiology or Medicine has been awarded to: Alligator carries on the legacy 1901 Emil von Behring 1902 Ronald Ross 1903 Niels Ryberg Finsen 1904 Ivan Pavlov of the Nobel Prize winners in 1905 Robert Koch 1906 Camillo Golgi 1907 Alphonse Laveran Medicine and Chemistry . 1908 Ilja Metjnikov Paul Ehrlich 1909 Theodor Kocher On Monday October 1, it was announced that James P. Allison and Tasuku Honjo 1910 Albrecht Kossel 1911 Allvar Gullstrand had been awarded the 2018 Nobel Prize in Physiology or Medicine for discov- 1912 Alexis Carrel 1913 Charles Richet eries on immune checkpoints – which according to the Nobel Assembly at the 1914 Robert Bárány 1919 Jules Bordet Karolinska Institute “has revolutionized treatment and changed our view of how 1920 August Krogh 1922 Archibald V. Hill cancers can be treated.” Otto Meyerhof 1923 Frederick G. Banting John Macleod I share the opinion of the Nobel Assembly. 1924 Willem Einthoven 1926 Johannes Fibiger The groundbreaking research by James 1927 Julius Wagner- Jauregg Allison and Tasuku Honjo on how the 1928 Charles Nicolle immune system can be used to fight cancer 1929 Christiaan Eijkman Sir Frederick Hopkins has profoundly changed the therapeutic 1930 Karl Landsteiner 1931 Otto Warburg arena. Not only in terms of how we treat 1932 Sir Charles Sherrington cancer but also on the prospect of surviving Edgar Adrian the disease. -

Biologyabc OF
According to new syllabus prescribed by Central Board of Secondary Education (CBSE), New Delhi and State Boards of Uttarakhand, Karnataka (II nd Year PUC), Chhattisgarh, Jharkhand, Punjab, Haryana, Himachal, Kerala, Mizoram, Meghalaya, Nagaland, Assam, Manipur and other States following CBSE & ISC curriculum. BIOLOGYabc OF Class XII PART-I By Dr. B. B. Arora M.Sc., Ph.D., Dip. in French Formerly Head, Deptt. of Botany, Dyal Singh College, Karnal Strictly A. K. Sabharwal in accordance M.Sc., M.Phil. (Gold-Medalist), with the Latest Formerly Head, Deptt. of Zoology, Guidelines and Syllabus S.D. College, Including Panipat Value Based Questions issued by GENERAL EDITORS Dr. Ruchi Arora N.C.E.R.T. / C.B.S.E. Raj Sabharwal Suman Shreya THOROUGHLY REVISED & UPDATED EDITION 2017–2018 MODERN PUBLISHERS (Producers of Quality Textbooks) Price of Part III&:890.00 OUR ADDRESSES IN INDIA New Delhi: MBD House, Gulab Bhawan, 6, Bahadur Shah Zafar Marg Ph. 23317931, 23318301 Mumbai: A-683, T.T.C. Industrial Area, M.I.D.C. Off. Thane-Belapur Road, Navi Mumbai Ph. 32996410, 27780821, 8691053365 Chennai: No. 26 B/2 SIDCO Estate, North Phase, Pataravakkam Ambattur Industrial Estate, Ambattur Ph. 26359376, 26242350 Chennai: Plot No. 3018, Old Y Block, 3rd Street, 12th Main Road, Anna Nagar West, Chennai Ph. 23741471 Kolkata: 6DW\DP%XLOGLQJ'5D¿$KPHG.LGZDL0DUJ Ph. 22296863, 22161670 Jalandhar City: MBD House, Railway Road Ph. 2458388, 2459046, 2455663 Bengaluru:VW0DLQ,QGXVWULDO7RZQ 1HDU&KRZGHVKZDUL.DO\DQ0DQWDS :HVWRI&KRUG5RDG5DMDMLQDJDU Ph. 23103329, 23104667 Hyderabad: 3-4-492, Varun Towers, Barkatpura Ph. 27564788, 9985820001 Ernakulam: Surabhi Building, South Janatha Road, Palarivattom Ph. -
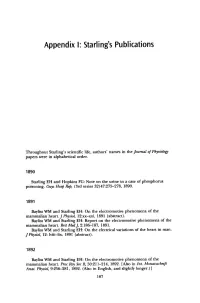
Appendix I: Starling's Publications
Appendix I: Starling's Publications Throughout Starling's scientific life, authors' names in the Journal of Physiology papers were in ilIphabetical order. 1890 Starling EH and Hopkins FG: Note on the urine in a case of phosphorus poisoning. Guys Hosp Rep, (3rd series 32)47:27!>-278, 1890. 1891 Bayliss WM and Starling EH: On the electromotive phenomena of the mammalian heart.] Physio~ 12:xx-xxi, 1891 (abstract). Bayliss WM and Starling EH: Report on the electromotive phenomena of the mammalian heart. Brit MedJ, 2:186-187, 1891. Bayliss WM and Starling EH: On the electrical variations of the heart in man. ] Physio~ 12: lviii-lix, 1891 (abstract). 1892 Bayliss WM and Starling EH: On the electromotive phenomena of the mammalian heart. Proc Roy Soc B, 50:211-214, 1892. [Also in Int. Monatsschrift Anat. Physiol, 9:256-281, 1892. (Also in English, and slightly longer.) I 187 188 Appendix I: Starling's Publications Bayliss WM and Starling EH: On some points in the innervation of the mammalian heart. J Physio~ 13:407-418, 1892. Starling EH and Bayliss WM: Note on a form of blood pressure manometer. Guys Hosp Rep (3rd series 33), 48:307-310, 1892. Starling EH: Elements of Human Physiolofry. P. Blakiston, Son, and Co., Philadel phia, 1892. [This work went through 8 editions, the last by J. and A. Churchill, London, in 1907.] 1893 Starling EH: Contributions to the physiology of lymph secretion. (From Breslau)] Physio~ 14:131-153, 1893. Starling EH: Zum Aufsuchen des Peptons in Gewebsflussigkeiten. Zhl Physio~ 6: 395-396, 1893. [Four of Starling's lectures were published in Guy's Hospital Gazette (new series, 7) in 1893.They were on lymph, coagulation of the blood, inflammation (and chemotaxis), and diabetes.] 1894 Starling EH and Tubby AH: On the absorption from and secretion into the serous cavities.