Nomination Background: N-(3-Chloroallyl)Hexaminium Chloride
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Formaldehyde Test Kit Utility
HHS Public Access Author manuscript Author ManuscriptAuthor Manuscript Author Cutan Ocul Manuscript Author Toxicol. Author Manuscript Author manuscript; available in PMC 2019 June 01. Published in final edited form as: Cutan Ocul Toxicol. 2019 June ; 38(2): 112–117. doi:10.1080/15569527.2018.1471485. Undeclared Formaldehyde Levels in Patient Consumer Products: Formaldehyde Test Kit Utility Jason E. Ham1, Paul Siegel1,*, and Howard Maibach2 1Health Effects Laboratory Division, National Institute for Occupational Safety and Health, Morgantown, WV, USA 2Department of Dermatology, School of Medicine, University of California-San Francisco, San Francisco, CA, USA Abstract Formaldehyde allergic contact dermatitis (ACD) may be due to products with free formaldehyde or formaldehyde-releasing agents, however, assessment of formaldehyde levels in such products is infrequently conducted. The present study quantifies total releasable formaldehyde from “in-use” products associated with formaldehyde ACD and tests the utility of commercially available formaldehyde spot test kits. Personal care products from 2 patients with ACD to formaldehyde were initially screened at the clinic for formaldehyde using a formaldehyde spot test kit. Formaldehyde positive products were sent to the laboratory for confirmation by gas chromatography-mass spectrometry. In addition, 4 formaldehyde spot test kits were evaluated for potential utility in a clinical setting. Nine of the 10 formaldehyde spot test kit positive products obtained from formaldehyde allergic patients had formaldehyde with total releasable formaldehyde levels ranging from 5.4 to 269.4 μg/g. Of these, only 2 shampoos tested listed a formaldehyde-releasing agent in the ingredients or product literature. Subsequently, commercially available formaldehyde spot test kits were evaluated in the laboratory for ability to identify formaldehyde in personal care products. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -

Comparative Analysis of Chlorhexidine Gluconate, Povidone Iodine and Chloroxylenol As Scrubbing Solution
British Journal of Pharmacology and Toxicology 1(2): 93-95, 2010 ISSN: 2044-2467 © Maxwell Scientific Organization, 2010 Submitted date: May 20, 2010 Accepted date: August 21, 2010 Published date: November 15, 2010 Comparative Analysis of Chlorhexidine Gluconate, Povidone Iodine and Chloroxylenol as Scrubbing Solution 1A.S. Yakubu, 1A.A. Abubakar, 2M.D. Salihu, 1A. Jibril and 1I. Isah 1Department of Veterinary Medicine, Surgery and Theriogenology 2Department of Veterinary Public Health and Preventive Medicine, Usmanu Danfodiyo University, Sokoto Abstract: The study was carried out to determine the efficacy of stock concentration of the commonly used disinfectant as scrub solution for surgical site in goats. The evaluation of efficacy and safety of commercially available disinfectant and antiseptic (0.3% Chlorhexidine gluconate, 0.4% Chloroxylenol and 4% Povidone iodine) as scrub solution for surgical site, using stock concentration was assessed in thirty (30) Red Sokoto goats undergoing non elective surgical procedures at Usmanu Danfodiyo University, Veterinary Teaching Hospital and Zonal Veterinary Clinic, Sokoto. Colony counting was used to quantify skin bacteria Colony Forming Unit (CFU) at surgical site before and after skin preparation. Reduction of CFU before and after preparation was significant with all the three disinfectants compared (p<0.05) and the result shows that Povidone iodine and Chloroxylenol to be less effecacious than Chlorhexidine gluconate when mean colony forming unit after two minute of preparing the surgical sites. -

Disinfection of Tonometers a Report by the American Academy of Ophthalmology
Ophthalmic Technology Assessment Disinfection of Tonometers A Report by the American Academy of Ophthalmology Anna K. Junk, MD,1 Philip P. Chen, MD,2 Shan C. Lin, MD,3 Kouros Nouri-Mahdavi, MD,4 Sunita Radhakrishnan, MD,5 Kuldev Singh, MD, MPH,6 Teresa C. Chen, MD7 Objective: To examine the efficacy of various disinfection methods for reusable tonometer prisms in eye care and to highlight how disinfectants can damage tonometer tips and cause subsequent patient harm. Methods: Literature searches were conducted last in October 2016 in the PubMed and the Cochrane Library databases for original research investigations. Reviews, non-English language articles, nonophthalmology articles, surveys, and case reports were excluded. Results: The searches initially yielded 64 unique citations. After exclusion criteria were applied, 10 labo- ratory studies remained for this review. Nine of the 10 studies used tonometer prisms and 1 used steel discs. The infectious agents covered in this assessment include adenovirus 8 and 19, herpes simplex virus (HSV) 1 and 2, human immunodeficiency virus 1, hepatitis C virus, enterovirus 70, and variant Creutzfeldt-Jakob disease. All 4 studies of adenovirus 8 concluded that after sodium hypochlorite (dilute bleach) disinfection, the virus was undetectable, but only 2 of the 4 studies found that 70% isopropyl alcohol (e.g., alcohol wipes or soaks) eradicated all viable virus. All 3 HSV studies concluded that both sodium hypochlorite and 70% isopropyl alcohol eliminated HSV. Ethanol, 70% isopropyl alcohol, dilute bleach, and mechanical cleaning all lack the ability to remove cellular debris completely, which is necessary to prevent prion transmission. Therefore, single-use tonometer tips or disposable tonometer covers should be considered when treating patients with suspected prion disease. -

Formaldehyde May Be Found in Cosmetic Products Even When Unlabelled
Open Med. 2015; 10: 323-328 Research Article Open Access Laura Malinauskiene*, Audra Blaziene, Anzelika Chomiciene, Marléne Isaksson Formaldehyde may be found in cosmetic products even when unlabelled Abstract: Concomitant contact allergy to formaldehyde reliable method for detecting formaldehyde presence in and formaldehyde-releasers remains common among cosmetic products. patients with allergic contact dermatitis. Concentration of free formaldehyde in cosmetic products within allowed Keywords: chromotropic acid; formaldehyde; formalde- limits have been shown to induce dermatitis from short- hyde-releaser; high-performance liquid chromatography term use on normal skin. DOI 10.1515/med-2015-0047 The aim of this study was to investigate the formalde- Received: February 2, 2015; accepted: May 28, 2015 hyde content of cosmetic products made in Lithuania. 42 samples were analysed with the chromotropic acid (CA) method for semi-quantitative formaldehyde deter- mination. These included 24 leave-on (e.g., creams, 1 Introduction lotions) and 18 rinse-off (e.g., shampoos, soaps) products. Formaldehyde is a well-documented contact allergen. Formaldehyde releasers were declared on the labels of 10 Over recent decades, the prevalence of contact allergy to products. No formaldehyde releaser was declared on the formaldehyde has been found to be 8-9% in the USA and label of the only face cream investigated, but levels of free 2-3% in European countries [1]. formaldehyde with the CA method was >40 mg/ml and Formaldehyde as such is very seldomly used in cosmetic when analysed with a high-performance liquid chromato- products anymore, but preservatives releasing formalde- graphic method – 532 ppm. According to the EU Cosmetic hyde in the presence of water are widely used in many directive, if the concentration of formaldehyde is above cosmetic products (e.g., shampoos, creams, etc.), topical 0.05% a cosmetic product must be labelled “contains medications and household products (e.g., dishwashing formaldehyde“. -

Allergic Contact Dermatitis from Formaldehyde Exposure
DOI: 10.5272/jimab.2012184.255 Journal of IMAB - Annual Proceeding (Scientific Papers) 2012, vol. 18, book 4 ALLERGIC CONTACT DERMATITIS FROM FORMALDEHYDE EXPOSURE Maya Lyapina1, Angelina Kisselova-Yaneva 2, Assya Krasteva2, Mariana Tzekova -Yaneva2, Maria Dencheva-Garova2 1) Department of Hygiene, Medical Ecology and Nutrition, Medical Faculty, 2) Department of Oral and Image Diagnostic, Faculty of Dental Medicine, Medical University, Sofia,Bulgaria ABSTRACT atmospheric air, tobacco smoke, use of cosmetic products Formaldehyde is a ubiquitous chemical agent, a part and detergents, and in less extend – water and food of our outdoor and indoor working and residential consumption (11, 81). It is released into the atmosphere environment. Healthcare workers in difficult occupations are through fumes from automobile exhausts without catalytic among the most affected by formaldehyde exposure. convertors and by manufacturing facilities that burn fossil Formaldehyde is an ingredient of some dental materials. fuels in usual concentration about 1-10 ppb. Uncontrolled Formaldehyde is well-known mucous membrane irritant and forest fires and the open burning of waste also give off a primary skin sensitizing agent associated with both contact formaldehyde. It is believed that the daily exposure from dermatitis (Type IV allergy), and immediate, anaphylactic atmospheric air is up to 0.1 mg (35, 43, 44). reactions (Type I allergy). Inhalation exposure to According to the WHO industrial emissions could formaldehyde was identified as a potential cause of asthma. appear at each step of production, use, transportation, or Quite a few investigations are available concerning health deposition of formaldehyde-containing products. issues for dental students following formaldehyde exposure. Formaldehyde emissions are detected from various Such studies would be beneficial for early diagnosis of industries – energy industry, wood and paper product hypersensitivity, adequate prophylactic, risk assessment and industries, textile production and finishing, chemical management of their work. -

Disinfection and Sterilization
Disinfection and Sterilization William A. Rutala, Ph.D., M.P.H. University of North Carolina (UNC) Health Care System and UNC at Chapel Hill, NC Disinfection and Sterilization z HICPAC Guideline z Provide overview of disinfection and sterilization principles z Emerging pathogens and prions z Current Research Clostridium difficile Ophthalmic equipment (applanation tonometers) Infrared coagulation Microfiber mops Computer keyboards QUAT absorption Failure to follow disinfection/sterilization principles and patient exposures 1 disinfectionandsterilization.org Disinfection and Sterilization in Healthcare Facilities WA Rutala, DJ Weber, and HICPAC, “In press” z Overview Last CDC guideline in 1985 274 pages (>130 pages preamble, 21 pages recommendations, glossary of terms, tables/figures, >1000 references) Evidence-based guideline Cleared by HICPAC February 2003 Reviewed by OMB Publication in December 2006 2 Efficacy of Disinfection/Sterilization Influencing Factors Cleaning of the object Organic and inorganic load present Type and level of microbial contamination Concentration of and exposure time to disinfectant/sterilant Nature of the object Temperature and relative humidity 3 Disinfection and Sterilization EH Spaulding believed that how an object will be disinfected depended on the object’s intended use. CRITICAL - objects which enter normally sterile tissue or the vascular system or through which blood flows should be sterile. SEMICRITICAL - objects that touch mucous membranes or skin that is not intact require a disinfection process (high-level disinfection [HLD]) that kills all microorganisms but high numbers of bacterial spores. NONCRITICAL -objects that touch only intact skin require low-level disinfection. 4 Processing “Critical” Patient Care Objects Classification: Critical objects enter normally sterile tissue or vascular system, or through which blood flows. -

Safety Assessment of Imidazolidinyl Urea As Used in Cosmetics
Safety Assessment of Imidazolidinyl Urea as Used in Cosmetics Status: Re-Review for Panel Review Release Date: May 10, 2019 Panel Meeting Date: June 6-7, 2019 The 2019 Cosmetic Ingredient Review Expert Panel members are: Chair, Wilma F. Bergfeld, M.D., F.A.C.P.; Donald V. Belsito, M.D.; Ronald A. Hill, Ph.D.; Curtis D. Klaassen, Ph.D.; Daniel C. Liebler, Ph.D.; James G. Marks, Jr., M.D., Ronald C. Shank, Ph.D.; Thomas J. Slaga, Ph.D.; and Paul W. Snyder, D.V.M., Ph.D. The CIR Executive Director is Bart Heldreth, Ph.D. This safety assessment was prepared by Christina L. Burnett, Senior Scientific Analyst/Writer. © Cosmetic Ingredient Review 1620 L Street, NW, Suite 1200 ♢ Washington, DC 20036-4702 ♢ ph 202.331.0651 ♢ fax 202.331.0088 ♢ [email protected] Distributed for Comment Only -- Do Not Cite or Quote Commitment & Credibility since 1976 Memorandum To: CIR Expert Panel Members and Liaisons From: Christina Burnett, Senior Scientific Writer/Analyst Date: May 10, 2019 Subject: Re-Review of the Safety Assessment of Imidazolidinyl Urea Imidazolidinyl Urea was one of the first ingredients reviewed by the CIR Expert Panel, and the final safety assessment was published in 1980 with the conclusion “safe when incorporated in cosmetic products in amounts similar to those presently marketed” (imurea062019origrep). In 2001, after considering new studies and updated use data, the Panel determined to not re-open the safety assessment (imurea062019RR1sum). The minutes from the Panel deliberations of that re-review are included (imurea062019min_RR1). Minutes from the deliberations of the original review are unavailable. -
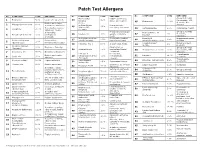
Patch Test Allergens
Patch Test Allergens No. COMPOUND CONC EXPOSURE No. COMPOUND CONC EXPOSURE No. COMPOUND CONC EXPOSURE Mixed dialkyl Rubber accelerator, Group B steroids: 1 Benzocaine 5.0% Local ester anesthetic 24 1.0% fluocinonide, TAC, thiourea assoc. w/ neoprene. 45 Budesonide 0.01% desonide. Also Rubber accelerator, Cl+Me- 2 Mercaptobenzothiazole 1.0% isothiazolinone Preservative in Group D. cutting oils, antifreeze 25 .01% In cosmetics, waxes, (Kathon CG, cosmetics, shampoos. Compositae mix 5.0% Compositae flowers. 3 Colophony 20.0% 46 adhesives. “Rosin.” 100ppm) Group D steroids: In hair dyes, Preservative in topical Hydrocortisone-17- 47 1% Temovate, 4 Paraphenylenediamine 1.0% photographic 26 Paraben mix 12% agents, cosmetics, butyrate Diprosone. chemicals foods. Methyldibromoglutar Preservative against Dimethylol In permanent press 27 0.5% 48 4.5% Imidazolidinyl urea Preservative, onitrile (MDBGN) bacteria and fungi dihydroxyethylene urea clothing. 5 2.0% (Germall 115) formaldehyde releaser Cocamidopropyl In hair and bath 28 Fragrance mix 1 8.0% In cosmetics, foods. 1% 49 ibetaine products. Cinnamic aldehyde 6 1.0% Fragrance. flavoring Disinfectant on (Cinnamyl) Group B steroids: 29 Glutaraldehyde 0.5% medical and dental 50 Triamcinolone acetonide 1.0% fluocinonide, TAC, 7 Amerchol L 101 50.0% Emulsifiers, Emollients equipment desonide. 2-Bromo-2- Preservative, Topical amide Rubber accelerator, 51 Lidocaine 15.0% 8 Carba mix 3.0% 30 nitropropane-l,3-diol 0.5% formaldehyde anesthetic. Adhesive (Bronopol) releaser. Topical amide Neomycin sulfate 20.0% Topical antibiotic. Sesquiterpene 52 Dibucaine hydrochloride 2.5% 9 0.1% Compositae flowers. anesthetic. 31 lactone Mix 10 Thiuram mix 1.0% Rubber accelerator Cosmetics, scents and Lauryl glucoside 3.0% surfactant Fragrance Mix II 14.0% 53 32 flavorings In leather, rubber, Clobetasol-17- plastics, disinfectants, Vehicle for cosmetics, 54 1.0% Group B steroids Formaldehyde 1.0% propionate 11 permanent press 33 Propylene glycol 30.0% topical medications. -

Disinfectant and Antiseptics Pdf
Disinfectant and antiseptics pdf Continue Antiseptics and disinfectants are very similar in that they are both used to kill microorganisms. They differ from each other, albeit in the composition of them, as well as their use. Antiseptics are used on living organisms, such as human skin, to kill any microorganisms living on the surface of the body. Disinfectants are used on non-living things such as countertops and handrails to kill microorganisms living on this inanimate surface. Antiseptics tend to have a lower concentration of a particular biocide, which is used in this product to clean the surface than that of a disinfectant. Since disinfectants are not intended for use on living tissues, but rather inanimate surfaces, they can use a higher concentration of biocide in the product, since there is no skin or tissue to worry about irritants. Antiseptics require a lower concentration of biocides, as too high concentrations of some biocides can cause a large amount of skin irritation. Some examples of antiseptics are mouthwash or hand sanitizer, both of which are safe for contact with your skin and also capable of being extremely effective in killing large numbers of microorganisms. Alcohol, bleach and formaldehyde are examples of various types of disinfectants used to kill microorganisms on the surface of any non-living objects. It is important that people know the difference between antiseptics and disinfectants, as they are both used for similar things, but in different ways. The use of disinfectant as an antiseptic is likely to irritate this tissue. In addition, the use of antiseptic as a disinfectant may result in less sufficient work to clean this surface due to the lower concentration of the biocide. -

August 14, 2019 Docket Nos. FDA-1975-N-0012
DEPARTMENT OF HEALTH AND HUMAN SERVICES Food and Drug Administration Silver Spring MD 20993 August 14, 2019 Docket Nos. FDA-1975-N-0012; FDA-2015-N-0101; and FDA-2016-N-0124 American Cleaning Institute Attention: Richard Sedlak Executive Vice President, Technical and International Affairs 1331 L Street, NW, Suite 650 Washington, DC 20005 Re: Benzalkonium Chloride, Benzethonium Chloride, Chloroxylenol, Ethanol, and Povidone- Iodine Dear Mr. Sedlak: This letter responds to American Cleaning Institute’s (ACI’s) March 12, 2019 request: (1) for a renewal of the extension of the deferral from final rulemaking under the OTC Drug Review on benzalkonium chloride, benzethonium chloride, chloroxylenol, ethanol, and povidone-iodine for use in nonprescription (often referred to as over-the-counter or OTC) consumer antiseptic wash, health care antiseptic, and consumer antiseptic rub drug products. In March 2016, FDA issued letters granting requests to defer three active ingredients—benzalkonium chloride, benzethonium chloride, and chloroxylenol—from inclusion in the final rulemaking for the December 2013 proposed rule for OTC consumer antiseptic washes (78 FR 76444). Similarly, in January 2017, FDA issued letters granting requests to defer six active ingredients—benzalkonium chloride, benzethonium chloride, chloroxylenol, ethanol, povidone-iodine, and isopropyl alcohol—from inclusion in the final rulemaking for the May 2015 proposed rule for OTC health care antiseptics (80 FR 25166). In October 2017, FDA issued letters granting requests to defer three -

Environmental Health Criteria 242
INTERNATIONAL PROGRAMME ON CHEMICAL SAFETY Environmental Health Criteria 242 DERMAL EXPOSURE IOMC INTER-ORGANIZATION PROGRAMME FOR THE SOUND MANAGEMENT OF CHEMICALS A cooperative agreement among FAO, ILO, UNDP, UNEP, UNIDO, UNITAR, WHO, World Bank and OECD This report contains the collective views of an international group of experts and does not necessarily represent the decisions or the stated policy of the World Health Organization The International Programme on Chemical Safety (IPCS) was established in 1980. The overall objec- tives of the IPCS are to establish the scientific basis for assessment of the risk to human health and the environment from exposure to chemicals, through international peer review processes, as a prerequi- site for the promotion of chemical safety, and to provide technical assistance in strengthening national capacities for the sound management of chemicals. This publication was developed in the IOMC context. The contents do not necessarily reflect the views or stated policies of individual IOMC Participating Organizations. The Inter-Organization Programme for the Sound Management of Chemicals (IOMC) was established in 1995 following recommendations made by the 1992 UN Conference on Environment and Development to strengthen cooperation and increase international coordination in the field of chemical safety. The Participating Organizations are: FAO, ILO, UNDP, UNEP, UNIDO, UNITAR, WHO, World Bank and OECD. The purpose of the IOMC is to promote coordination of the policies and activities pursued by the Participating Organizations, jointly or separately, to achieve the sound management of chemicals in relation to human health and the environment. WHO Library Cataloguing-in-Publication Data Dermal exposure. (Environmental health criteria ; 242) 1.Hazardous Substances - poisoning.