Assessment of the Antibiotic Resistance Effects of Biocides
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
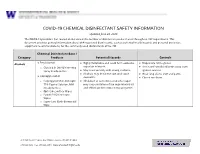
EH&S COVID-19 Chemical Disinfectant Safety Information
COVID-19 CHEMICAL DISINFECTANT SAFETY INFORMATION Updated June 24, 2020 The COVID-19 pandemic has caused an increase in the number of disinfection products used throughout UW departments. This document provides general information about EPA-registered disinfectants, such as potential health hazards and personal protective equipment recommendations, for the commonly used disinfectants at the UW. Chemical Disinfectant Base / Category Products Potential Hazards Controls ● Ethyl alcohol Highly flammable and could form explosive Disposable nitrile gloves Alcohols ● ● vapor/air mixtures. ● Use in well-ventilated areas away from o Clorox 4 in One Disinfecting Spray Ready-to-Use ● May react violently with strong oxidants. ignition sources ● Alcohols may de-fat the skin and cause ● Wear long sleeve shirt and pants ● Isopropyl alcohol dermatitis. ● Closed toe shoes o Isopropyl Alcohol Antiseptic ● Inhalation of concentrated alcohol vapor 75% Topical Solution, MM may cause irritation of the respiratory tract (Ready to Use) and effects on the central nervous system. o Opti-Cide Surface Wipes o Powell PII Disinfectant Wipes o Super Sani Cloth Germicidal Wipe 201 Hall Health Center, Box 354400, Seattle, WA 98195-4400 206.543.7262 ᅵ fax 206.543.3351ᅵ www.ehs.washington.edu ● Formaldehyde Formaldehyde in gas form is extremely Disposable nitrile gloves for Aldehydes ● ● flammable. It forms explosive mixtures with concentrations 10% or less ● Paraformaldehyde air. ● Medium or heavyweight nitrile, neoprene, ● Glutaraldehyde ● It should only be used in well-ventilated natural rubber, or PVC gloves for ● Ortho-phthalaldehyde (OPA) areas. concentrated solutions ● The chemicals are irritating, toxic to humans ● Protective clothing to minimize skin upon contact or inhalation of high contact concentrations. -

Mechanisms and Strategies to Overcome Multiple Drug Resistance in Cancer
View metadata, citation and similar papers at core.ac.uk brought to you by CORE provided by Elsevier - Publisher Connector FEBS Letters 580 (2006) 2903–2909 Minireview Mechanisms and strategies to overcome multiple drug resistance in cancer Tomris Ozben* Akdeniz University, Faculty of Medicine, Department of Biochemistry, 07070 Antalya, Turkey Received 30 January 2006; accepted 9 February 2006 Available online 17 February 2006 Edited by Horst Feldmann The cytotoxic drugs that are most frequently associated with Abstract One of the major problems in chemotherapy is multi- drug resistance (MDR) against anticancer drugs. ATP-binding MDR are hydrophobic, amphipathic natural products, such as cassette (ABC) transporters are a family of proteins that medi- the taxanes (paclitaxel and docetaxel), vinca alkaloids (vinorel- ate MDR via ATP-dependent drug efflux pumps. Many MDR bine, vincristine, and vinblastine), anthracyclines (doxorubicin, inhibitors have been identified, but none of them have been pro- daunorubicin, and epirubicin), epipodophyllotoxins (etoposide ven clinically useful without side effects. Efforts continue to dis- and teniposide), antimetabolites (methorexate, fluorouracil, cover not toxic MDR inhibitors which lack pharmacokinetic cytosar, 5-azacytosine, 6-mercaptopurine, and gemcitabine) interactions with anticancer drugs. Novel approaches have also topotecan, dactinomycin, and mitomycin C [4,6–8]. been designed to inhibit or circumvent MDR. In this review, Overexpression of ATP-binding cassette (ABC) transporters the structure and function of ABC transporters and development has been shown to be responsible for MDR [5]. Therefore eluci- of MDR inhibitors are described briefly including various ap- dation of the structure and function for each ABC transporter is proaches to suppress MDR mechanisms. -

A Review on Antimicrobial Resistance in Developing Countries
mac har olo P gy : & O y r p t e s i n Biochemistry & Pharmacology: Open A m c e c h e c Ravalli, et al. Biochem Pharmacol 2015, 4:2 s o i s B Access DOI: 10.4172/2167-0501.1000r001 ISSN: 2167-0501 Review Open Access A Review on Antimicrobial Resistance in Developing Countries Ravalli R1*, NavaJyothi CH2, Sushma B3 and Amala Reddy J4 1Deparment of Pharmaceutical Sciences, Andhra University, Vishakapatnam, India 2University College of Technology, Osmania University, Hyderabad, India 3Deparment of Medicinal Chemistry, National Institute of Pharmaceutical Education and Research (NIPER) Hyderabad, India 4Deparment of Pharmaceutical Sciences, Osmania University, Hyderabad, India *Corresponding author: Ravalli R, Deparment of Pharmaceutical Sciences, Andhra University, Vishakapatnam, India, Tel: + 0437-869-033; E-mail: [email protected] Received date: April 13, 2015; Accepted date: April 14, 2015; Published date: April 21, 2015 Copyright: © 2015 Ravalli Remella. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestri cted use, distribution, and reproduction in any medium, provided the original author and source are credited. Availability of Antimicrobial Drugs isolates were proof against Principen, Co-trimoxazole, and bactericide, and 14-40% were given with Mecillinam [6]. This was associate degree Although foremost potent and recently developed antimicrobial outsized increase over the half resistant isolates notable in 1991, before medicine are offered throughout the globe, in developing countries the drug was wide on the market. Throughout infectious disease their use is confined to people who are flush enough to afford them. In epidemics the organism has the flexibleness to develop increasing tertiary referral hospitals like the Kenyatta National Hospital in resistance, typically by acquisition of plasmids. -

Expression of Cytokeratin Confers Multiple Drug Resistance (Multidrug Resance/Cytoskeleton) PATRICIA A
Proc. Nati. Acad. Sci. USA Vol. 91, pp. 5311-5314, June 1994 Pharmacology Expression of cytokeratin confers multiple drug resistance (multidrug resance/cytoskeleton) PATRICIA A. BAUMAN*, WILLIAM S. DALTON*t, JOHN M. ANDERSONt, AND ANNE E. CRESSO§ Departments of *Pharmacology and Toxicology, tMedicine, and *Radiation Oncology, The University of Arizona, The Arizona Cancer Center, Tucson, AZ 85724 Communicated by Gertrude B. Elion, February 23, 1994 (received for review October 21, 1993) ABSTRACT The cytokeratin network is an extensive fda- We utilized a mouse fibroblast cell line and a transfected mentous structure in the cytoplasm whose biological function(s) variant expressing cytokeratins 8 and 18 (9) to test whether is unknown. Based upon previous data showing the modifica- cytokeratin expression could alter the cell survival response tion ofcytokeratin by mitoxantrone, we investigated the ability to six different chemotherapeutic drugs. of cytokeratin networks to influence the survival response of cells to chemotherapeutic agents. We have compared the MATERIALS AND METHODS survival of mouse L fibroblasts lacking cytokeratins with that of L cells transfected with cytokeratins 8 and 18 in the presence Tumor Cell Lines, Growth Curves, and Cell Cycle Distri- of chemotherapeutic drugs. The expression of cytokeratins 8 butions. Parental L cells and transfected LK8+18 cells were and 18 conferred a multiple drug resistance phenotype on cells obtained from Robert Oshima (La Jolla Cancer Research exposed to mitoxantrone, doxorubicin, methotrexate, melpha- Foundation, La Jolla, CA) and maintained as described (9). Ian, Colcemid, and vincristine. The degree of drug resistance Mock transfectants (LPBMOC) were created by simultane- was 5-454 times that of parental cells, depending upon the ous calcium phosphate transfection of pGEM-3 (Promega) agent used. -

Chapter 12 Antimicrobial Therapy Antibiotics
Chapter 12 Antimicrobial Therapy Topics: • Ideal drug - Antimicrobial Therapy - Selective Toxicity • Terminology - Survey of Antimicrobial Drug • Antibiotics - Microbial Drug Resistance - Drug and Host Interaction An ideal antimicrobic: Chemotherapy is the use of any chemical - soluble in body fluids, agent in the treatment of disease. - selectively toxic , - nonallergenic, A chemotherapeutic agent or drug is any - reasonable half life (maintained at a chemical agent used in medical practice. constant therapeutic concentration) An antibiotic agent is usually considered to - unlikely to elicit resistance, be a chemical substance made by a - has a long shelf life, microorganism that can inhibit the growth or - reasonably priced. kill microorganisms. There is no ideal antimicrobic An antimicrobic or antimicrobial agent is Selective Toxicity - Drugs that specifically target a chemical substance similar to an microbial processes, and not the human host’s. antibiotic, but may be synthetic. Antibiotics Spectrum of antibiotics and targets • Naturally occurring antimicrobials – Metabolic products of bacteria and fungi – Reduce competition for nutrients and space • Bacteria – Streptomyces, Bacillus, • Molds – Penicillium, Cephalosporium * * 1 The mechanism of action for different 5 General Mechanisms of Action for antimicrobial drug targets in bacterial cells Antibiotics - Inhibition of Cell Wall Synthesis - Disruption of Cell Membrane Function - Inhibition of Protein Synthesis - Inhibition of Nucleic Acid Synthesis - Anti-metabolic activity Antibiotics -
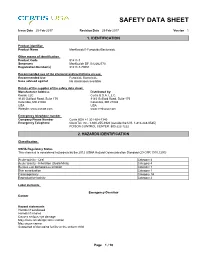
Mankocide® Fungicide/Bactericide
SAFETY DATA SHEET Issue Date 25-Feb-2017 Revision Date 25-Feb-2017 Version 1 1. IDENTIFICATION Product identifier Product Name ManKocide® Fungicide/Bactericide Other means of identification Product Code 91411-7 Synonyms ManKocide DF, B12262770 Registration Number(s) 91411-7-70051 Recommended use of the chemical and restrictions on use Recommended Use Fungicide Bactericide Uses advised against No information available Details of the supplier of the safety data sheet Manufacturer Address Distributed by: Kocide LLC Certis U.S.A. L.L.C. 9145 Guilford Road, Suite 175 9145 Guilford Road, Suite 175 Columbia, MD 21046 Columbia, MD 21046 USA USA Website: www.kocide.com www.certisusa.com Emergency telephone number Company Phone Number Certis USA +1 301-604-7340 Emergency Telephone ChemTel, Inc.: 1-800-255-3924 (outside the U.S. 1-813-248-0585) POISON CONTROL CENTER: 800-222-1222 2. HAZARDS IDENTIFICATION Classification OSHA Regulatory Status This chemical is considered hazardous by the 2012 OSHA Hazard Communication Standard (29 CFR 1910.1200) Acute toxicity - Oral Category 4 Acute toxicity - Inhalation (Dusts/Mists) Category 4 Serious eye damage/eye irritation Category 1 Skin sensitization Category 1 Carcinogenicity Category 1A Reproductive toxicity Category 2 Label elements Emergency Overview Danger Hazard statements Harmful if swallowed Harmful if inhaled Causes serious eye damage May cause an allergic skin reaction May cause cancer Suspected of damaging fertility or the unborn child _____________________________________________________________________________________________ -

National Center for Toxicological Research
National Center for Toxicological Research Annual Report Research Accomplishments and Plans FY 2015 – FY 2016 Page 0 of 193 Table of Contents Preface – William Slikker, Jr., Ph.D. ................................................................................... 3 NCTR Vision ......................................................................................................................... 7 NCTR Mission ...................................................................................................................... 7 NCTR Strategic Plan ............................................................................................................ 7 NCTR Organizational Structure .......................................................................................... 8 NCTR Location and Facilities .............................................................................................. 9 NCTR Advances Research Through Outreach and Collaboration ................................... 10 NCTR Global Outreach and Training Activities ............................................................... 12 Global Summit on Regulatory Science .................................................................................................12 Training Activities .................................................................................................................................14 NCTR Scientists – Leaders in the Research Community .................................................. 15 Science Advisory Board ................................................................................................... -

Antibiotic Resistance: from the Bench to Patients
antibiotics Editorial Antibiotic Resistance: From the Bench to Patients Márió Gajdács 1,* and Fernando Albericio 2,3 1 Department of Pharmacodynamics and Biopharmacy, Faculty of Pharmacy, University of Szeged, Dóm tér 10., 6720 Szeged, Hungary 2 School of Chemistry, University of KwaZulu-Natal, Durban 4001, South Africa 3 Department of Organic Chemistry, University of Barcelona, CIBER-BBN, 08028 Barcelona, Spain * Correspondence: [email protected]; Tel.: +36-62-341-330 Received: 20 August 2019; Accepted: 26 August 2019; Published: 27 August 2019 The discovery and subsequent clinical introduction of antibiotics is one of the most important game-changers in the history of medicine [1]. These drugs have saved millions of lives from infections that would previously have been fatal, and later, they allowed for the introduction of surgical interventions, organ transplantation, care of premature infants, and cancer chemotherapy [2]. Nevertheless, the therapy of bacterial infections is becoming less and less straightforward due to the emergence of multidrug resistance (MDR) in these pathogens [3]. Direct consequences of antibiotic resistance include delays in the onset of the appropriate (effective) antimicrobial therapy, the need to use older, more toxic antibiotics (e.g., colistin) with a disadvantageous side-effect profile, longer hospital stays, and an increasing burden on the healthcare infrastructure; overall, a decrease in the quality-of-life (QoL) and an increase in the mortality rate of the affected patients [4,5]. To highlight the severity of the issue, several international declarations have been published to call governments around the globe to take action on antimicrobial resistance [6–9]. Since the 1980s, pharmaceutical companies have slowly turned away from antimicrobial research and towards the drug therapy of chronic non-communicable diseases [10,11]. -

Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020
First independent framework for assessing pharmaceutical company action Antimicrobial Resistance Benchmark 2020 Antimicrobial Resistance Benchmark 2020 ACKNOWLEDGEMENTS The Access to Medicine Foundation would like to thank the following people and organisations for their contributions to this report.1 FUNDERS The Antimicrobial Resistance Benchmark research programme is made possible with financial support from UK AID and the Dutch Ministry of Health, Welfare and Sport. Expert Review Committee Research Team Reviewers Hans Hogerzeil - Chair Gabrielle Breugelmans Christine Årdal Gregory Frank Fatema Rafiqi Karen Gallant Nina Grundmann Adrián Alonso Ruiz Hans Hogerzeil Magdalena Kettis Ruth Baron Hitesh Hurkchand Joakim Larsson Dulce Calçada Joakim Larsson Marc Mendelson Moska Hellamand Marc Mendelson Margareth Ndomondo-Sigonda Kevin Outterson Katarina Nedog Sarah Paulin (Observer) Editorial Team Andrew Singer Anna Massey Deirdre Cogan ACCESS TO MEDICINE FOUNDATION Rachel Jones The Access to Medicine Foundation is an independent Emma Ross non-profit organisation based in the Netherlands. It aims to advance access to medicine in low- and middle-income Additional contributors countries by stimulating and guiding the pharmaceutical Thomas Collin-Lefebvre industry to play a greater role in improving access to Alex Kong medicine. Nestor Papanikolaou Address Contact Naritaweg 227-A For more information about this publication, please contact 1043 CB, Amsterdam Jayasree K. Iyer, Executive Director The Netherlands [email protected] +31 (0) 20 215 35 35 www.amrbenchmark.org 1 This acknowledgement is not intended to imply that the individuals and institutions referred to above endorse About the cover: Young woman from the Antimicrobial Resistance Benchmark methodology, Brazil, where 40%-60% of infections are analyses or results. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Selling Mercury Cosmetics and Pharmaceuticals (W-Hw4-22)
www.pca.state.mn.us Selling mercury cosmetics and pharmaceuticals Mercury-containing skin lightening creams, lotions, soaps, ointments, lozenges, pharmaceuticals and antiseptics Mercury is a toxic element that was historically used in some cosmetic, pharmaceutical, and antiseptic products due to its unique properties and is now being phased out of most uses. The offer, sale, or distribution of mercury-containing products is regulated in Minnesota by the Minnesota Pollution Control Agency (MPCA). Anyone offering a mercury-containing product for sale or donation in Minnesota is subject to these requirements, whether a private citizen, collector, non-profit organization, or business. Offers and sales through any method are regulated, whether in a store or shop, classified advertisement, flea market, or online. If a mercury-containing product is located in Minnesota, it is regulated, regardless of where a purchaser is located. Note: This fact sheet discusses the requirements and restrictions of the MPCA. Cosmetics and pharmaceuticals may also be regulated for sale whether they contain mercury or not by other state or federal agencies, including the Minnesota Board of Pharmacy and the U.S. Food & Drug Administration. See More information on page 2. What are the risks of using mercury-containing products? Use of mercury-containing products can damage the brain, kidneys, and liver. Children and pregnant women are at increased risk. For more information about the risks of mercury exposure, visit the Minnesota Department of Health. See More information on the page 2. If you believe you have been exposed to a mercury-containing product, contact your health care provider or the Minnesota Poison Control Center at 1-800-222-1222. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard.