Antiseptics and Disinfectants: Activity, Action, and Resistance
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
Chemical Disinfectants for Biohazardous Materials (3/21)
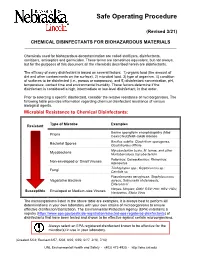
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

Decontamination of Rooms, Medical Equipment and Ambulances Using an Aerosol of Hydrogen Peroxide Disinfectant B.M
Journal of Hospital Infection (2006) 62, 149–155 www.elsevierhealth.com/journals/jhin Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant B.M. Andersena,*, M. Rascha, K. Hochlina, F.-H. Jensenb, P. Wismarc, J.-E. Fredriksend aDepartment of Hospital Infection, Ulleva˚l University Hospital, Oslo, Norway bDivision of Pre-hospital Care, Ulleva˚l University Hospital, Oslo, Norway cDepartment of Medical Equipment, Ulleva˚l University Hospital, Oslo, Norway dHealth and Environment AS, Oslo, Norway Received 17 November 2004; accepted 1 July 2005 KEYWORDS Summary A programmable device (Sterinis, Gloster Sante Europe) Room decontamina- providing a dry fume of 5% hydrogen peroxide (H2O2) disinfectant was tion; Ambulance tested for decontamination of rooms, ambulances and different types of decontamination; medical equipment. Pre-set concentrations were used according to the Medical equipment decontamination; volumes of the rooms and garages. Three cycles were performed with Hydrogen peroxide increasing contact times. Repetitive experiments were performed using fume decontamina- Bacillus atrophaeus (formerly Bacillus subtilis) Raven 1162282 spores to tion; Spore test control the effect of decontamination; after a sampling plan, spore strips were placed in various positions in rooms, ambulances, and inside and outside the items of medical equipment. Decontamination was effective in 87% of 146 spore tests in closed test rooms and in 100% of 48 tests in a surgical department when using three cycles. One or two cycles had no effect. The sporicidal effect on internal parts of the medical equipment was only 62.3% (220 tests). When the devices were run and ventilated during decontamination, 100% (57/57) of spore strips placed inside were decontaminated. -

National Center for Toxicological Research
National Center for Toxicological Research Annual Report Research Accomplishments and Plans FY 2015 – FY 2016 Page 0 of 193 Table of Contents Preface – William Slikker, Jr., Ph.D. ................................................................................... 3 NCTR Vision ......................................................................................................................... 7 NCTR Mission ...................................................................................................................... 7 NCTR Strategic Plan ............................................................................................................ 7 NCTR Organizational Structure .......................................................................................... 8 NCTR Location and Facilities .............................................................................................. 9 NCTR Advances Research Through Outreach and Collaboration ................................... 10 NCTR Global Outreach and Training Activities ............................................................... 12 Global Summit on Regulatory Science .................................................................................................12 Training Activities .................................................................................................................................14 NCTR Scientists – Leaders in the Research Community .................................................. 15 Science Advisory Board ................................................................................................... -

1 Brief Report: the Virucidal Efficacy of Oral Rinse Components Against SARS-Cov-2 in Vitro Evelina Statkute1†, Anzelika Rubin
bioRxiv preprint doi: https://doi.org/10.1101/2020.11.13.381079; this version posted November 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. Brief Report: The Virucidal Efficacy of Oral Rinse Components Against SARS-CoV-2 In Vitro Evelina Statkute1†, Anzelika Rubina1†, Valerie B O’Donnell1, David W. Thomas2† Richard J. Stanton1† 1Systems Immunity University Research Institute, Division of Infection & Immunity, School of Medicine, Heath Park, Cardiff, CF14 4XN 2Advanced Therapies Group, School of Dentistry, Cardiff University, Heath Park, Cardiff CF14 4XY, UK †These authors contributed equally * Correspondence: [email protected], [email protected] Running title: Virucidal Activity of Mouthwashes Keywords: SARS-CoV2, mouthwash, lipid, envelope Disclosure: Venture Life Group plc provided information on mouthwash formulations employed in the study, but had no role in funding, planning, execution, analysis or writing of this study. A separate study funded to Cardiff University by Venture Life Group is assessing in vivo efficacy of CPC in patients with COVID19. The investigators declare no direct conflicts exist. 1 bioRxiv preprint doi: https://doi.org/10.1101/2020.11.13.381079; this version posted November 13, 2020. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted bioRxiv a license to display the preprint in perpetuity. It is made available under aCC-BY-ND 4.0 International license. -

Antimicrobial Activity of Cationic
ANTIMICROBIAL ACTIVITY OF CATIONIC ANTISEPTICS IN LAYER-BY-LAYER THIN FILM ASSEMBLIES A Thesis by CHARLENE MYRIAH DVORACEK Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE May 2009 Major Subject: Mechanical Engineering ANTIMICROBIAL ACTIVITY OF CATIONIC ANTISEPTICS IN LAYER-BY-LAYER THIN FILM ASSEMBLIES A Thesis by CHARLENE MYRIAH DVORACEK Submitted to the Office of Graduate Studies of Texas A&M University in partial fulfillment of the requirements for the degree of MASTER OF SCIENCE Approved by: Chair of Committee, Jaime Grunlan Committee Members, Michael Benedik Xinghang Zhang Head of Department, Dennis O'Neal May 2009 Major Subject: Mechanical Engineering iii ABSTRACT Antimicrobial Activity of Cationic Antiseptics in Layer-by-Layer Thin Film Assemblies. (May 2009) Charlene Myriah Dvoracek, B.S., Rose-Hulman Institute of Technology Chair of Advisory Committee: Dr. Jaime Grunlan Layer-by-layer (LbL) assembly has proven to be a powerful technique for assembling thin films with a variety of properties including electrochromic, molecular sensing, oxygen barrier, and antimicrobial. LbL involves the deposition of alternating cationic and anionic ingredients from solution, utilizing the electrostatic charges to develop multilayer films. The present work incorporates cationic antimicrobial agents into the positively-charged layers of LbL assemblies. When these thin films are exposed to a humid environment, the antimicrobial molecules readily diffuse out and prevent bacterial growth. The influence of exposure time, testing temperature, secondary ingredients and number of bilayers on antimicrobial efficacy is evaluated here. Additionally, film growth and microstructure are analyzed to better understand the behavior of these films. -

)&F1y3x PHARMACEUTICAL APPENDIX to THE
)&f1y3X PHARMACEUTICAL APPENDIX TO THE HARMONIZED TARIFF SCHEDULE )&f1y3X PHARMACEUTICAL APPENDIX TO THE TARIFF SCHEDULE 3 Table 1. This table enumerates products described by International Non-proprietary Names (INN) which shall be entered free of duty under general note 13 to the tariff schedule. The Chemical Abstracts Service (CAS) registry numbers also set forth in this table are included to assist in the identification of the products concerned. For purposes of the tariff schedule, any references to a product enumerated in this table includes such product by whatever name known. Product CAS No. Product CAS No. ABAMECTIN 65195-55-3 ACTODIGIN 36983-69-4 ABANOQUIL 90402-40-7 ADAFENOXATE 82168-26-1 ABCIXIMAB 143653-53-6 ADAMEXINE 54785-02-3 ABECARNIL 111841-85-1 ADAPALENE 106685-40-9 ABITESARTAN 137882-98-5 ADAPROLOL 101479-70-3 ABLUKAST 96566-25-5 ADATANSERIN 127266-56-2 ABUNIDAZOLE 91017-58-2 ADEFOVIR 106941-25-7 ACADESINE 2627-69-2 ADELMIDROL 1675-66-7 ACAMPROSATE 77337-76-9 ADEMETIONINE 17176-17-9 ACAPRAZINE 55485-20-6 ADENOSINE PHOSPHATE 61-19-8 ACARBOSE 56180-94-0 ADIBENDAN 100510-33-6 ACEBROCHOL 514-50-1 ADICILLIN 525-94-0 ACEBURIC ACID 26976-72-7 ADIMOLOL 78459-19-5 ACEBUTOLOL 37517-30-9 ADINAZOLAM 37115-32-5 ACECAINIDE 32795-44-1 ADIPHENINE 64-95-9 ACECARBROMAL 77-66-7 ADIPIODONE 606-17-7 ACECLIDINE 827-61-2 ADITEREN 56066-19-4 ACECLOFENAC 89796-99-6 ADITOPRIM 56066-63-8 ACEDAPSONE 77-46-3 ADOSOPINE 88124-26-9 ACEDIASULFONE SODIUM 127-60-6 ADOZELESIN 110314-48-2 ACEDOBEN 556-08-1 ADRAFINIL 63547-13-7 ACEFLURANOL 80595-73-9 ADRENALONE -

Genetic Basis of Resistance to Quaternary Ammonium Compounds – the Qac Genes and Their Role: a Review
Veterinarni Medicina, 57, 2012 (6): 275–281 Review Article Genetic basis of resistance to quaternary ammonium compounds – the qac genes and their role: a review Z. Jaglic, D. Cervinkova Veterinary Research Institute, Brno, Czech Republic ABSTRACT: Although the qac genes are named after one of their main substrates (i.e., quaternary ammonium compounds), these genes also code for resistance to a broad spectrum of other cationic compounds such as inter- calating dyes, diamidines and biguanides. The various Qac proteins are involved in relatively low specific efflux- based multidrug pumps and belong to a family of small multidrug resistance proteins. Even though the practical significance of qac-mediated resistance lies mainly in resistance to antiseptics, contradictory findings on this issue are still reported. Therefore, the aim of this review is to summarise the current knowledge on qac-mediated resistance with special emphasis on resistance to antiseptics and its relevance for practice. Keywords: antimicrobial; disinfectant; biocide; benzalkonium; chlorhexidine; cation; susceptibility Contents 3.2. Substrates of qac-mediated resistance 1. Introduction 3.3. Adaptive response to antiseptics 2. The qac genes and their distribution 4. The qac genes and resistance to antibiotics 3. Qac-mediated resistance 5. Conclusions 3.1. Mechanisms of qac-mediated resistance 6. References 1. Introduction first described genetic determinant of resistance to antiseptics was the qacA gene found on pSK1 Resistance to intercalating dyes (i.e. acriflavine and β-lactamase/heavy metal resistance plasmids and ethidium) was associated with particular ge- (Gillespie et al. 1986; Lyon and Skurray 1987). A netic elements, namely staphylococcal β-lactamase range of other qac genes linked with particular plas- plasmids, already more than 40 years ago (Ericson mids (Littlejohn et al. -

Reseptregisteret 2013–2017 the Norwegian Prescription Database
LEGEMIDDELSTATISTIKK 2018:2 Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Reseptregisteret 2013–2017 Tema: Legemidler og eldre The Norwegian Prescription Database 2013–2017 Topic: Drug use in the elderly Christian Berg Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Utgitt av Folkehelseinstituttet/Published by Norwegian Institute of Public Health Område for Helsedata og digitalisering Avdeling for Legemiddelstatistikk Juni 2018 Tittel/Title: Legemiddelstatistikk 2018:2 Reseptregisteret 2013–2017 / The Norwegian Prescription Database 2013–2017 Forfattere/Authors: Christian Berg, redaktør/editor Hege Salvesen Blix Olaug Fenne Kari Furu Vidar Hjellvik Kari Jansdotter Husabø Irene Litleskare Marit Rønning Solveig Sakshaug Randi Selmer Anne-Johanne Søgaard Sissel Torheim Acknowledgement: Julie D. W. Johansen (English text) Bestilling/Order: Rapporten kan lastes ned som pdf på Folkehelseinstituttets nettsider: www.fhi.no The report can be downloaded from www.fhi.no Grafisk design omslag: Fete Typer Ombrekking: Houston911 Kontaktinformasjon/Contact information: Folkehelseinstituttet/Norwegian Institute of Public Health Postboks 222 Skøyen N-0213 Oslo Tel: +47 21 07 70 00 ISSN: 1890-9647 ISBN: 978-82-8082-926-9 Sitering/Citation: Berg, C (red), Reseptregisteret 2013–2017 [The Norwegian Prescription Database 2013–2017] Legemiddelstatistikk 2018:2, Oslo, Norge: Folkehelseinstituttet, 2018. Tidligere utgaver / Previous editions: 2008: Reseptregisteret 2004–2007 / The Norwegian Prescription Database 2004–2007 2009: Legemiddelstatistikk 2009:2: Reseptregisteret 2004–2008 / The Norwegian Prescription Database 2004–2008 2010: Legemiddelstatistikk 2010:2: Reseptregisteret 2005–2009. Tema: Vanedannende legemidler / The Norwegian Prescription Database 2005–2009. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -

Being Aware of Chlorhexidine Allergy
Being aware of chlorhexidine allergy If you have an immediate allergic reaction to chlorhexidine you may experience symptoms such as: x itching x skin rash (hives) x swelling x anaphylaxis. People who develop anaphylaxis to chlorhexidine may have experienced mild reactions, such as skin rash, to chlorhexidine before. Irritant contact dermatitis or allergic contact dermatitis Chlorhexidine can also cause irritant dermatitis. This is not a true allergic reaction. It is caused by chlorhexidine directly irritating skin and results in rough, dry and scaly Chlorhexidine is an antiseptic. Allergic reactions to skin, sometimes with weeping sores. chlorhexidine are rare but are becoming more common. Chlorhexidine is used in many products both in Chlorhexidine can also cause allergic contact hospitals and in the community. dermatitis. Symptoms look like irritant dermatitis, but the cause of the symptoms is delayed by 12-48 hours Why have I been given this factsheet? after contact with chlorhexidine. You have been given this brochure because you have had a reaction to a medication, a medical dressing Both irritant dermatitis and allergic contact dermatitis or antiseptic. This may or may not be caused by a caused by chlorhexidine are annoying but not chlorhexidine allergy. dangerous. It is important that you are aware of the possibility of an It is recommended that you avoid chlorhexidine if you allergy. experience these responses as some people have gone on to develop immediate allergic reaction to chlorhexidine. Allergic reactions to chlorhexidine Severe allergic reactions to chlorhexidine are rare, but How do I know which products contain they can be serious. Immediate allergic reactions can chlorhexidine? cause anaphlaxis (a very severe allergic reaction which can be life-threatening). -

In Vivo Evaluation of the Virucidal Efficacy of Chlorhexidine and Povidone-Iodine Mouthwashes Against Salivary SARS-Cov-2
medRxiv preprint doi: https://doi.org/10.1101/2021.03.07.21252302; this version posted March 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity. It is made available under a CC-BY-NC-ND 4.0 International license . Title: In vivo evaluation of the virucidal efficacy of Chlorhexidine and Povidone-iodine mouthwashes against salivary SARS-CoV-2. Rola Elzein1*, Fadi Abdel-Sater2*, Soha Fakhreddine3, Pierre Abi Hanna3, Rita Feghali4, Hassan Hamad5, Fouad Ayoub6 ¹Department of Pediatric Dentistry and Public Dental Health, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon 2Laboratory of Cancer Biology and Cellular Immunology, Department of Biological Sciences, Faculty of Sciences, Lebanese University, Beirut, Lebanon 3Infectious Diseases division, Rafik Hariri University Hospital, Beirut, Lebanon 4Department of Laboratory Medicine, Rafik Hariri University Hospital, Beirut, Lebanon 5Medical care Laboratory, Faculty of Public Health IV, Lebanese University, Zahle, Lebanon 6Department of Forensic Odontology, Human Identification and Anthropology, Faculty of Dental Medicine, Lebanese University, Beirut, Lebanon *CORRESPONDING AUTHORS: Rola ELZEIN; Mobile number: 009613252480; Email address: [email protected] Fadi Abdelsater; Mobile number: 009613781176; Email address: [email protected] NOTE: This preprint reports new research that has not been certified by peer review and should not be used to guide clinical practice. medRxiv preprint doi: https://doi.org/10.1101/2021.03.07.21252302; this version posted March 17, 2021. The copyright holder for this preprint (which was not certified by peer review) is the author/funder, who has granted medRxiv a license to display the preprint in perpetuity.