Disinfectant and Antiseptics Pdf
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-
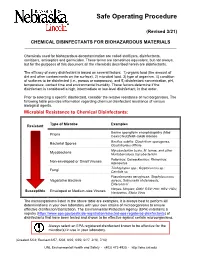
Chemical Disinfectants for Biohazardous Materials (3/21)
Safe Operating Procedure (Revised 3/21) CHEMICAL DISINFECTANTS FOR BIOHAZARDOUS MATERIALS ____________________________________________________________________________ Chemicals used for biohazardous decontamination are called sterilizers, disinfectants, sanitizers, antiseptics and germicides. These terms are sometimes equivalent, but not always, but for the purposes of this document all the chemicals described herein are disinfectants. The efficacy of every disinfectant is based on several factors: 1) organic load (the amount of dirt and other contaminants on the surface), 2) microbial load, 3) type of organism, 4) condition of surfaces to be disinfected (i.e., porous or nonporous), and 5) disinfectant concentration, pH, temperature, contact time and environmental humidity. These factors determine if the disinfectant is considered a high, intermediate or low-level disinfectant, in that order. Prior to selecting a specific disinfectant, consider the relative resistance of microorganisms. The following table provides information regarding chemical disinfectant resistance of various biological agents. Microbial Resistance to Chemical Disinfectants: Type of Microbe Examples Resistant Bovine spongiform encephalopathy (Mad Prions Cow) Creutzfeldt-Jakob disease Bacillus subtilis; Clostridium sporogenes, Bacterial Spores Clostridioides difficile Mycobacterium bovis, M. terrae, and other Mycobacteria Nontuberculous mycobacterium Poliovirus; Coxsackievirus; Rhinovirus; Non-enveloped or Small Viruses Adenovirus Trichophyton spp.; Cryptococcus sp.; -

Antiseptics and Disinfectants for the Treatment Of
Verstraelen et al. BMC Infectious Diseases 2012, 12:148 http://www.biomedcentral.com/1471-2334/12/148 RESEARCH ARTICLE Open Access Antiseptics and disinfectants for the treatment of bacterial vaginosis: A systematic review Hans Verstraelen1*, Rita Verhelst2, Kristien Roelens1 and Marleen Temmerman1,2 Abstract Background: The study objective was to assess the available data on efficacy and tolerability of antiseptics and disinfectants in treating bacterial vaginosis (BV). Methods: A systematic search was conducted by consulting PubMed (1966-2010), CINAHL (1982-2010), IPA (1970- 2010), and the Cochrane CENTRAL databases. Clinical trials were searched for by the generic names of all antiseptics and disinfectants listed in the Anatomical Therapeutic Chemical (ATC) Classification System under the code D08A. Clinical trials were considered eligible if the efficacy of antiseptics and disinfectants in the treatment of BV was assessed in comparison to placebo or standard antibiotic treatment with metronidazole or clindamycin and if diagnosis of BV relied on standard criteria such as Amsel’s and Nugent’s criteria. Results: A total of 262 articles were found, of which 15 reports on clinical trials were assessed. Of these, four randomised controlled trials (RCTs) were withheld from analysis. Reasons for exclusion were primarily the lack of standard criteria to diagnose BV or to assess cure, and control treatment not involving placebo or standard antibiotic treatment. Risk of bias for the included studies was assessed with the Cochrane Collaboration’s tool for assessing risk of bias. Three studies showed non-inferiority of chlorhexidine and polyhexamethylene biguanide compared to metronidazole or clindamycin. One RCT found that a single vaginal douche with hydrogen peroxide was slightly, though significantly less effective than a single oral dose of metronidazole. -

Decontamination of Rooms, Medical Equipment and Ambulances Using an Aerosol of Hydrogen Peroxide Disinfectant B.M
Journal of Hospital Infection (2006) 62, 149–155 www.elsevierhealth.com/journals/jhin Decontamination of rooms, medical equipment and ambulances using an aerosol of hydrogen peroxide disinfectant B.M. Andersena,*, M. Rascha, K. Hochlina, F.-H. Jensenb, P. Wismarc, J.-E. Fredriksend aDepartment of Hospital Infection, Ulleva˚l University Hospital, Oslo, Norway bDivision of Pre-hospital Care, Ulleva˚l University Hospital, Oslo, Norway cDepartment of Medical Equipment, Ulleva˚l University Hospital, Oslo, Norway dHealth and Environment AS, Oslo, Norway Received 17 November 2004; accepted 1 July 2005 KEYWORDS Summary A programmable device (Sterinis, Gloster Sante Europe) Room decontamina- providing a dry fume of 5% hydrogen peroxide (H2O2) disinfectant was tion; Ambulance tested for decontamination of rooms, ambulances and different types of decontamination; medical equipment. Pre-set concentrations were used according to the Medical equipment decontamination; volumes of the rooms and garages. Three cycles were performed with Hydrogen peroxide increasing contact times. Repetitive experiments were performed using fume decontamina- Bacillus atrophaeus (formerly Bacillus subtilis) Raven 1162282 spores to tion; Spore test control the effect of decontamination; after a sampling plan, spore strips were placed in various positions in rooms, ambulances, and inside and outside the items of medical equipment. Decontamination was effective in 87% of 146 spore tests in closed test rooms and in 100% of 48 tests in a surgical department when using three cycles. One or two cycles had no effect. The sporicidal effect on internal parts of the medical equipment was only 62.3% (220 tests). When the devices were run and ventilated during decontamination, 100% (57/57) of spore strips placed inside were decontaminated. -
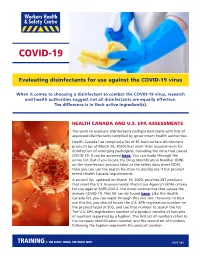
Evaluating Disinfectants for Use Against the COVID-19 Virus
When it comes to choosing a disinfectant to combat the COVID-19 virus, research and health authorities suggest not all disinfectants are equally effective. The difference is in their active ingredient(s). HEALTH CANADA AND U.S. EPA ASSESSMENTS The work to evaluate disinfectants perhaps best starts with lists of approved disinfectants compiled by government health authorities. Health Canada has compiled a list of 85 hard surface disinfectant products (as of March 20, 2020) that meet their requirements for disinfection of emerging pathogens, including the virus that causes COVID-19. It can be accessed here. You can wade through the entire list. But if you locate the Drug Identification Number (DIN) on the disinfectant product label or the safety data sheet (SDS), then you can use the search function to quickly see if the product meets Health Canada requirements. A second list, updated on March 19, 2020, provides 287 products that meet the U.S. Environmental Protection Agency’s (EPA) criteria for use against SARS-CoV-2, the novel coronavirus that causes the disease COVID-19. This list can be found here. Like the Health Canada list, you can wade through this one too. However, to best use this list, you should locate the U.S. EPA registration number on the product label or SDS, and use that number to search the list. The U.S. EPA registration number of a product consists of two sets of numbers separated by a hyphen. The first set of numbers refers to the company identification number, and the second set of numbers following the hyphen represents the product number. -

Effect of Polyhexamethylene Biguanide in Combination with Undecylenamidopropyl Betaine Or Pslg on Biofilm Clearance
International Journal of Molecular Sciences Article Effect of Polyhexamethylene Biguanide in Combination with Undecylenamidopropyl Betaine or PslG on Biofilm Clearance Yaqian Zheng 1,2,†, Di Wang 1,† and Luyan Z. Ma 1,3,* 1 State Key Laboratory of Microbial Resources, Institute of Microbiology, Chinese Academy of Sciences, Beijing 100101, China; [email protected] (Y.Z.); [email protected] (D.W.) 2 College of Life Sciences, University of Chinese Academy of Sciences, Beijing 100049, China 3 Savaid Medical School, University of Chinese Academy of Sciences, Beijing 100049, China * Correspondence: [email protected]; Tel.: +86-10-64807437 † These authors have contributed equally to this work. Abstract: Hospital-acquired infection is a great challenge for clinical treatment due to pathogens’ biofilm formation and their antibiotic resistance. Here, we investigate the effect of antiseptic agent polyhexamethylene biguanide (PHMB) and undecylenamidopropyl betaine (UB) against biofilms of four pathogens that are often found in hospitals, including Gram-negative bacteria Pseudomonas aeruginosa and Escherichia coli, Gram-positive bacteria Staphylococcus aureus, and pathogenic fungus, Candida albicans. We show that 0.02% PHMB, which is 10-fold lower than the concentration of commercial products, has a strong inhibitory effect on the growth, initial attachment, and biofilm formation of all tested pathogens. PHMB can also disrupt the preformed biofilms of these pathogens. In contrast, 0.1% UB exhibits a mild inhibitory effect on biofilm formation of the four pathogens. This concentration inhibits the growth of S. aureus and C. albicans yet has no growth effect on P. aeruginosa or E. coli. UB only slightly enhances the anti-biofilm efficacy of PHMB on P. -

Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic
Safer Disinfectant Use in Child Care and Schools During the COVID-19 Pandemic Vickie Leonard, PhD Environmental Health in Early Care and Educaon Project, Western States Pediatric Environmental Health Specialty Unit (WSPEHSU) 1 Why Should We Be Concerned about Environmental Health in ECE? 2 Why Should We Be Concerned about Environmental Health in ECE? • There are 8 million children in child care centers in the U.S. A child may spend up to 12,500 hours in an ECE facility. A million child care providers work in these centers in the U.S. Half are child-bearing age. • Many toxicants found in child care facilities are not addressed in state child care health and safety regulations. • No agency at the state or federal level is charged with ensuring children’s health and safety in and around schools and ECE facilities. • No systematic means exists for collecting data on environmental exposures in these buildings. • Teachers have more protection in these buildings (unions, OSHA) than children do 3 Why Should We Be Concerned about Environmental Health in ECE? • Many people think that adults and children are exposed to, and affected by, toxic chemicals in the same way. • This is not the case. • Children • have higher exposures to toxicants in the environment, • are more vulnerable to the effects of those toxicants than adults. 4 Cleaning and Disinfec?ng Products: A Major Source of Exposure in Child Care and Schools • Products used to clean, sanitize and disinfect child care facilities and schools are a good example of the pervasive and unregulated use of toxic chemicals that put the health of our children at risk. -

Comparison of Effectiveness Disinfection of 2%
ORIGINAL RESEARCH Journal of Dentomaxillofacial Science (J Dentomaxillofac Sci ) December 2018, Volume 3, Number 3: 169-171 P-ISSN.2503-0817, E-ISSN.2503-0825 Comparison of effectiveness disinfection of 2% Original Research glutaraldehyde and 4.8% chloroxylenol on tooth extraction instruments in the Department of Oral CrossMark http://dx.doi.org/10.15562/jdmfs.v3i2.794 Maxillofacial Surgery, Faculty of Dentistry, University of North Sumatera Month: December Ahyar Riza,* Isnandar, Indra B. Siregar, Bernard Volume No.: 3 Abstract Objective: To compare disinfecting effectiveness of 2% glutaraldehyde while the control group was treated with 4.8% chloroxylenol. Each Issue: 2 and 4.8% chloroxylenol on tooth extraction instruments at the instrument was pre-cleaned using a brush, water and soap for both Department of Oral Surgery, Faculty of Dentistry, University of North groups underwent the disinfection process. Sumatera. Results: The results were statistically analyzed using Mann-Whitney Material and Methods: This was an experimental study with post- Test. The comparison between glutaraldehyde and chloroxylenol First page No.: 147 test only control group design approach. Purposive technique is showed a significant difference to the total bacteria count on applied to collect samples which are lower molar extraction forceps. In instrument after disinfection (p=0.014 < 0.05). this study, sample were divided into 2 groups and each consisting of 18 Conclusion: 2% glutaraldehyde was more effective than 4.8% P-ISSN.2503-0817 instruments. The treatment group was treated with 2% glutaraldehyde chloroxylenol at disinfecting lower molar extraction forceps. Keyword: Disinfection, Glutaraldehyde, Chloroxylenol, Forceps E-ISSN.2503-0825 Cite this Article: Riza A, Siregar IB, Isnandar, Bernard. -

Comparative Analysis of Chlorhexidine Gluconate, Povidone Iodine and Chloroxylenol As Scrubbing Solution
British Journal of Pharmacology and Toxicology 1(2): 93-95, 2010 ISSN: 2044-2467 © Maxwell Scientific Organization, 2010 Submitted date: May 20, 2010 Accepted date: August 21, 2010 Published date: November 15, 2010 Comparative Analysis of Chlorhexidine Gluconate, Povidone Iodine and Chloroxylenol as Scrubbing Solution 1A.S. Yakubu, 1A.A. Abubakar, 2M.D. Salihu, 1A. Jibril and 1I. Isah 1Department of Veterinary Medicine, Surgery and Theriogenology 2Department of Veterinary Public Health and Preventive Medicine, Usmanu Danfodiyo University, Sokoto Abstract: The study was carried out to determine the efficacy of stock concentration of the commonly used disinfectant as scrub solution for surgical site in goats. The evaluation of efficacy and safety of commercially available disinfectant and antiseptic (0.3% Chlorhexidine gluconate, 0.4% Chloroxylenol and 4% Povidone iodine) as scrub solution for surgical site, using stock concentration was assessed in thirty (30) Red Sokoto goats undergoing non elective surgical procedures at Usmanu Danfodiyo University, Veterinary Teaching Hospital and Zonal Veterinary Clinic, Sokoto. Colony counting was used to quantify skin bacteria Colony Forming Unit (CFU) at surgical site before and after skin preparation. Reduction of CFU before and after preparation was significant with all the three disinfectants compared (p<0.05) and the result shows that Povidone iodine and Chloroxylenol to be less effecacious than Chlorhexidine gluconate when mean colony forming unit after two minute of preparing the surgical sites. -

Silver As a Drinking-Water Disinfectant
Silver as a drinking-water disinfectant Silver as a drinking-water disinfectant Alternative drinking-water disinfectants: silver ISBN 978-92-4-151369-2 © World Health Organization 2018 Some rights reserved. This work is available under the Creative Commons Attribution- NonCommercial-ShareAlike 3.0 IGO licence (CC BY-NC-SA 3.0 IGO; https://creativecommons.org/licenses/by-nc-sa/3.0/igo). Under the terms of this licence, you may copy, redistribute and adapt the work for non-commercial purposes, provided the work is appropriately cited, as indicated below. In any use of this work, there should be no suggestion that WHO endorses any specific organization, products or services. The use of the WHO logo is not permitted. If you adapt the work, then you must license your work under the same or equivalent Creative Commons licence. If you create a translation of this work, you should add the following disclaimer along with the suggested citation: “This translation was not created by the World Health Organization (WHO). WHO is not responsible for the content or accuracy of this translation. The original English edition shall be the binding and authentic edition”. Any mediation relating to disputes arising under the licence shall be conducted in accordance with the mediation rules of the World Intellectual Property Organization. Suggested citation. Alternative drinking-water disinfectants: bromine, iodine and silver. Geneva: World Health Organization; 2018. Licence: CC BY-NC-SA 3.0 IGO. Cataloguing-in-Publication (CIP) data. CIP data are available at http://apps.who.int/iris. Sales, rights and licensing. To purchase WHO publications, see http://apps.who.int/bookorders. -

Infection Prevention & Control Chlorhexidine
Winnipeg Regional Health Authority Acute Care Infection Prevention & Control Manual INFECTION PREVENTION & CONTROL CHLORHEXIDINE GLUCONATE CONCENTRATION FOR HAND HYGIENE COMMUNICATION FORM PART 1: ISSUE & RECOMMENDATIONS Issue: The WRHA Infection Prevention and Control program (IP&C) was requested to research and recommend acceptable concentrations of chlorhexidine gluconate (CHG) (2% versus 4%) for hand hygiene in all programs within WRHA sites, to ensure appropriate products are being used, and facilitate standardization. Recommendations: Use 2% CHG hand cleansers for hand hygiene when antimicrobial hand soap is indicated. Do NOT use 4% CHG for hand hygiene as the minimal improvement in efficacy (from 2%), does not warrant the increased frequency of skin irritation and breakdown, which ultimately impedes effective hand hygiene practices. PART 2: BACKGROUND: DISCUSSION OF ISSUE, OPTIONS AND ANALYSIS & REFERENCES Discussion of Issue: There are several different hand hygiene products used within and between WRHA sites. All areas should adhere to recommended hand hygiene products, as determined by available evidence. There are differences in when specific hand hygiene products are indicated. It is important to identify the appropriate product to use for the appropriate reason, as supported by evidence. Options and Analysis: 1. CHG has a cumulative effect when applied to the skin. In hand hygiene, this effect remains and is sustained, especially when hand hygiene is repeated. 2% CHG is appropriate for hand antisepsis because of the cumulative effect.1 2. Literature regarding differences between 2% and 4% CHG identifies there is minimal difference in efficacy between 2% and 4% CHG for hand antisepsis and cleansing.2 3. The frequency of skin irritation is concentration dependent, with products containing 4% most likely to cause dermatitis when used frequently for hand antisepsis. -

Disinfection of Tonometers a Report by the American Academy of Ophthalmology
Ophthalmic Technology Assessment Disinfection of Tonometers A Report by the American Academy of Ophthalmology Anna K. Junk, MD,1 Philip P. Chen, MD,2 Shan C. Lin, MD,3 Kouros Nouri-Mahdavi, MD,4 Sunita Radhakrishnan, MD,5 Kuldev Singh, MD, MPH,6 Teresa C. Chen, MD7 Objective: To examine the efficacy of various disinfection methods for reusable tonometer prisms in eye care and to highlight how disinfectants can damage tonometer tips and cause subsequent patient harm. Methods: Literature searches were conducted last in October 2016 in the PubMed and the Cochrane Library databases for original research investigations. Reviews, non-English language articles, nonophthalmology articles, surveys, and case reports were excluded. Results: The searches initially yielded 64 unique citations. After exclusion criteria were applied, 10 labo- ratory studies remained for this review. Nine of the 10 studies used tonometer prisms and 1 used steel discs. The infectious agents covered in this assessment include adenovirus 8 and 19, herpes simplex virus (HSV) 1 and 2, human immunodeficiency virus 1, hepatitis C virus, enterovirus 70, and variant Creutzfeldt-Jakob disease. All 4 studies of adenovirus 8 concluded that after sodium hypochlorite (dilute bleach) disinfection, the virus was undetectable, but only 2 of the 4 studies found that 70% isopropyl alcohol (e.g., alcohol wipes or soaks) eradicated all viable virus. All 3 HSV studies concluded that both sodium hypochlorite and 70% isopropyl alcohol eliminated HSV. Ethanol, 70% isopropyl alcohol, dilute bleach, and mechanical cleaning all lack the ability to remove cellular debris completely, which is necessary to prevent prion transmission. Therefore, single-use tonometer tips or disposable tonometer covers should be considered when treating patients with suspected prion disease. -

U.S. EPA, Pesticide Product Label, 776 DISINFECTANT VIRUCIDE
, 1-ls-lf9 UNITED ST ATES ENVIRONMENTAL PROTECTION AGENCY Carroll Company 2900 West Kingsley Road Garland, TX 75041 Subject: 776 Disinfectant, Virucide and Cleaner EPA Registration No. 4313-22 Amendment Dated November 9, 1998 Attn: Linda Kirk Kirby Director, Regulatory Compliance The amendment referred to above, submitted in connection with registration under the Federal Insecticide, Fungicide and Rodenticide Act, as amended, is acceptable. A stamped copy of the label is enclosed for your records. Submit one (I) copy ofthe finished printed label before this product is released for shipment. If you have any questions concerning the comments in this letter, you should contact Zenobia Jones at (703) 308-6198. Sincerely, ) JJ~lvJHdL Velma Noble Product Manager 31 Regulatory Management Branch I Antimicrobial Division (751 OW) COHCURRI!HCI!S ::::} ·m·I~ .Q........ ................ - ....................................... -................................ _............................. DATE ) . \-1i.-9l1... ....... ................... ................. .................................................................................... OFFICIAL FILE COpy Primed Oft R~cye/~d Paper ~' '....,-. " DISINFECTANT, UIRUCIDE* AND CLEANER FOR HOSPITAL INSTITUTIONAL ACTIVE INGREDIENT: AND iNDUSTRIAL USE Alkyl (C14 50%, C12 40%, C16 10%) dimelhyl • benzyl ammonium chloride........... 3.3 Yo ·Hum8n immunodeficiency virus, Type 1 (HIV-l) INERT INGR~DIENTS .................. 96.7% KEEP OUT OF REACH OF CHILDREN DANGER See back panel for additional precautionary