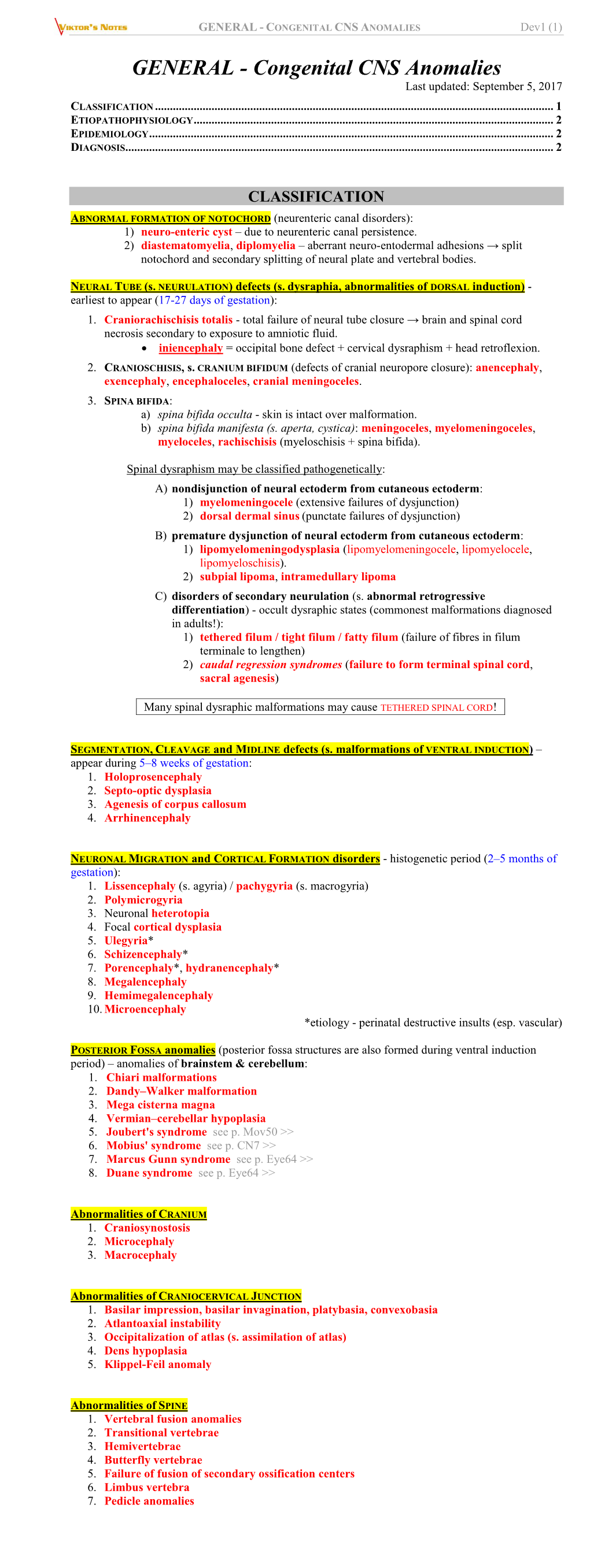
Congenital CNS Anomalies (General)
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Ultrasound Evaluation of the Central Nervous System
Ultrasound Evaluation of the Ultrasound Evaluation of the Central Nervous System Central Nervous System ••CNSCNS malformations are the second most Mani Montazemi, RDMS frequent category of congenital anomaly, Director of Ultrasound Education & Quality Assurancee after congenital heart disease Baylor College of Medicine Division of Maternal-Fetal Medicine ••PoorPoor timing of the examination, rather than Department of Obstetrics and Gynecology Texas Children’s Hospital, Pavilion for Women poor sensitivity, can be an important factor Houston Texas & in failing to detect a CNS abnormality Clinical Instructor Thomas Jefferson University Hospital Radiology Department Fetal Head Philadelphia, Pennsylvania Fetal Head Central Nervous System Brain Development 9 -13 weeks Rhombencephalon 5th Menstrual Week •Gives rise to hindbrain •4th ventricle Arises from the posterior surface of the embryonic ectoderm Mesencephalon •Gives rise to midbrain A small groove is found along •Aqueduct the midline of the embryo and the edges of this groove fold over to form a neuro tube that Prosencephalon gives rise to the fetal spinal •Gives rise to forebrain rd cord and brain •Lateral & 3 ventricles Fetal Head Fetal Head Ventricular view Neural Tube Defects ••LateralLateral ventricles ••ChoroidChoroid plexus Group of malformations: Thalamic view • Anencephaly ••MidlineMidline falx •Anencephaly ••CavumCavum septiseptipellucidi pellucidi ••CephalocelesCephaloceles ••ThalamiThalami ••SpinaSpina bifida Cerebellar view ••CerebellumCerebellum ••CisternaCisterna magna Fetal -

A Case Report Cem Yener Trakya University, Turkey
American Journal of Preventive Medicine and Public Health Open Access Iniencephaly: A Case Report Cem Yener Trakya University, Turkey ABSTRACT of head, spinal dysmorphism, and lordosis of cervicothoracic vertebrae. Iniencephaly is in the same family of neural tube defects as spina Iniencephaly is a rare neural tube defect characterized by the presence of occipital bone defects at foramen magnum, fixed retroflexion bifida, but it is more severe. The frequency varies between 0.1-10 / 10,000. Most of the fetuses are female. Etiopathogenesis is not known. According to some sources, it has been associated with trisomy 13, 18 and monosomy X. AFP(alfa-feto protein) as a biochemical marker is generally increased. Here we present a 30 years old 19 weeks pregnant women that was referred to our Perinatology Department. We detected polihydramnios, extreme retroflexion of the head, absent neck, low set ears and major cardiac anomaly on ultrasonography. We informed family and with family consent we terminated pregnancy (Image 1). In conclusion, iniencephaly is a neural tube defect with unknown etiopathogenesis. There is no standard treatment for iniencephaly since most infants rarely live longer than a few hours. Medicine is based more on prevention using supplementation with folic acid. Numerous studies have demonstrated that mothers can reduce the risk of neural tube birth defects such as iniencephaly by up to 70 percent with daily supplements of at least 4 mg of folic disordersacid. Pregnant so prenatal women care should is important avoid taking for these antiepileptic patients. drugs, diuretics, antihistamines, and sulfa drugs, which have been shown to be associated with an increased risk of neural tube defects. -

Split Notochord Syndrome
0021-7557/04/80-01/77 Jornal de Pediatria Copyright © 2004 by Sociedade Brasileira de Pediatria RELATO DE CASO Síndrome do notocórdio fendido, variante rara do cisto neuroentérico A rare variant of neuroenteric cyst: split notochord syndrome Lisieux E. Jesus1, Cristiano G. França2 Resumo Abstract Objetivo: Estudo de um caso de síndrome do notocórdio fendido, Objective: We present a case of split notochord syndrome, an forma extremamente rara de disrafismo medular. A literatura pertinen- extremely rare form of spinal dysraphism. te, pesquisada através das bases de dados MEDLINE e LILACS, é Description: We treated a 2 month-old boy presenting with an analisada e sumarizada. extensive lumbosacral deformity, hydrocephalus and apparent enteric Descrição: Foi atendido lactente masculino de 2 meses de idade segments in the dorsal midline, accompanied by an enteric fistula apresentando extensa deformidade de coluna lombo-sacra, hidrocefa- and imperforated anus. The malformation was diagnosed as split lia e exteriorização de alças intestinais pela linha média dorsal, notochord syndrome. The baby died as a result of sepsis before acompanhada de fístula entérica e imperfuração anal. A malformação surgical treatment could be attempted. foi diagnosticada como síndrome do notocórdio fendido. A criança Comments: Split notochord syndrome is the rarest form of evoluiu para óbito secundário a sepse antes de ser feito qualquer neuroenteric cyst described until this moment (<25 cases in the tratamento cirúrgico. literature). It is frequently associated with anorectal malformation, Comentários: A síndrome do notocórdio fendido é a forma mais intestinal fistulae and hydrocephalus. Prognosis is not necessarily rara de cisto neuroentérico já descrita (<25 casos descritos em poor and survival is possible if digestive malformations, hydrocephalus literatura) e está associada freqüentemente a fístulas digestivas, and the dysraphism itself are treated simultaneously. -

Pfeiffer Syndrome Type II Discovered Perinatally
Diagnostic and Interventional Imaging (2012) 93, 785—789 CORE Metadata, citation and similar papers at core.ac.uk Provided by Elsevier - Publisher Connector LETTER / Musculoskeletal imaging Pfeiffer syndrome type II discovered perinatally: Report of an observation and review of the literature a,∗ a a a H. Ben Hamouda , Y. Tlili , S. Ghanmi , H. Soua , b c b a S. Jerbi , M.M. Souissi , H. Hamza , M.T. Sfar a Unité de néonatologie, service de pédiatrie, CHU Tahar Sfar, 5111 Mahdia, Tunisia b Service de radiologie, CHU Tahar Sfar, 5111 Mahdia, Tunisia c Service de gynéco-obstétrique, CHU Tahar Sfar, 5111 Mahdia, Tunisia Pfeiffer syndrome, described for the first time by Pfeiffer in 1964, is a rare hereditary KEYWORDS condition combining osteochondrodysplasia with craniosynostosis [1]. This syndrome is Pfeiffer syndrome; also called acrocephalosyndactyly type 5, which is divided into three sub-types. Type I Cloverleaf skull; is the classic Pfeiffer syndrome, with autosomal dominant transmission, often associated Craniosynostosis; with normal intelligence. Types II and III occur as sporadic cases in individuals who have Syndactyly; craniosynostosis with broad thumbs, broad big toes, ankylosis of the elbows and visceral Prenatal diagnosis abnormalities [2]. We report a case of Pfeiffer syndrome type II, discovered perinatally, which is distinguished from type III by the skull appearing like a cloverleaf, and we shall discuss the clinical, radiological and evolutive features and the advantage of prenatal diagnosis of this syndrome with a review of the literature. Observation The case involved a male premature baby born at 36 weeks of amenorrhoea with multiple deformities at birth. The parents were not blood-related and in good health who had two other boys and a girl with normal morphology. -

Paternal Factors and Schizophrenia Risk: De Novo Mutations and Imprinting
Paternal Factors and Schizophrenia Risk: De Novo Mutations and Imprinting by Dolores Malaspina Downloaded from https://academic.oup.com/schizophreniabulletin/article/27/3/379/1835092 by guest on 23 September 2021 Abstract (Impagnatiello et al. 1998; Kao et al. 1998), but there is no consensus that any particular gene plays a meaning- There is a strong genetic component for schizophrenia ful role in the etiology of schizophrenia (Hyman 2000). risk, but it is unclear how the illness is maintained in Some of the obstacles in genetic research in schiz- the population given the significantly reduced fertility ophrenia are those of any complex disorder, and include of those with the disorder. One possibility is that new incomplete penetrance, polygenic interaction (epista- mutations occur in schizophrenia vulnerability genes. sis), diagnostic instability, and variable expressivity. If so, then those with schizophrenia may have older Schizophrenia also does not show a clear Mendelian fathers, because advancing paternal age is the major inheritance pattern, although segregation analyses have source of new mutations in humans. This review variably supported dominant, recessive, additive, sex- describes several neurodevelopmental disorders that linked, and oligogenic inheritance (Book 1953; Slater have been associated with de novo mutations in the 1958; Garrone 1962; Elston and Campbell 1970; Slater paternal germ line and reviews data linking increased and Cowie 1971; Karlsson 1972; Stewart et al. 1980; schizophrenia risk with older fathers. Several genetic Risch 1990a, 1990fc; reviewed by Kendler and Diehl mechanisms that could explain this association are 1993). Furthermore, both nonallelic (Kaufmann et al. proposed, including paternal germ line mutations, 1998) and etiologic heterogeneity (Malaspina et al. -

Bhagwan Moorjani, MD, FAAP, FAAN • Requires Knowledge of Normal CNS Developmental (I.E
1/16/2012 Neuroimaging in Childhood • Neuroimaging issues are distinct from Pediatric Neuroimaging in adults Neurometabolic-degenerative disorder • Sedation/anesthesia and Epilepsy • Motion artifacts Bhagwan Moorjani, MD, FAAP, FAAN • Requires knowledge of normal CNS developmental (i.e. myelin maturation) • Contrast media • Parental anxiety Diagnostic Approach Neuroimaging in Epilepsy • Age of onset • Peak incidence in childhood • Static vs Progressive • Occurs as a co-morbid condition in many – Look for treatable causes pediatric disorders (birth injury, – Do not overlook abuse, Manchausen if all is negative dysmorphism, chromosomal anomalies, • Phenotype presence (syndromic, HC, NCS, developmental delays/regression) systemic involvement) • Predominant symptom (epilepsy, DD, • Many neurologic disorders in children weakness/motor, psychomotor regression, have the same chief complaint cognitive/dementia) 1 1/16/2012 Congenital Malformation • Characterized by their anatomic features • Broad categories: based on embryogenesis – Stage 1: Dorsal Induction: Formation and closure of the neural tube. (Weeks 3-4) – Stage 2: Ventral Induction: Formation of the brain segments and face. (Weeks 5-10) – Stage 3: Migration and Histogenesis: (Months 2-5) – Stage 4: Myelination: (5-15 months; matures by 3 years) Dandy Walker Malformation Dandy walker • Criteria: – high position of tentorium – dysgenesis/agenesis of vermis – cystic dilatation of fourth ventricle • commonly associated features: – hypoplasia of cerebellum – scalloping of inner table of occipital bone • associated abnormalities: – hydrocephalus 75% – dysgenesis of corpus callosum 25% – heterotropia 10% 2 1/16/2012 Etiology of Epilepsy: Developmental and Genetic Classification of Gray Matter Heterotropia Cortical Dysplasia 1. Secondary to abnormal neuronal and • displaced masses of nerve cells • Subependymal glial proliferation/apoptosis (gray matter) heterotropia (most • most common: small nest common) 2. -
Split Spinal Cord Malformations in Children
Split spinal cord malformations in children Yusuf Ersahin, M.D., Saffet Mutluer, M.D., Sevgül Kocaman, R.N., and Eren Demirtas, M.D. Division of Pediatric Neurosurgery, Department of Neurosurgery, and Department of Pathology, Ege University Faculty of Medicine, Izmir, Turkey The authors reviewed and analyzed information on 74 patients with split spinal cord malformations (SSCMs) treated between January 1, 1980 and December 31, 1996 at their institution with the aim of defining and classifying the malformations according to the method of Pang, et al. Computerized tomography myelography was superior to other radiological tools in defining the type of SSCM. There were 46 girls (62%) and 28 boys (38%) ranging in age from less than 1 day to 12 years (mean 33.08 months). The mean age (43.2 months) of the patients who exhibited neurological deficits and orthopedic deformities was significantly older than those (8.2 months) without deficits (p = 0.003). Fifty-two patients had a single Type I and 18 patients a single Type II SSCM; four patients had composite SSCMs. Sixty-two patients had at least one associated spinal lesion that could lead to spinal cord tethering. After surgery, the majority of the patients remained stable and clinical improvement was observed in 18 patients. The classification of SSCMs proposed by Pang, et al., will eliminate the current chaos in terminology. In all SSCMs, either a rigid or a fibrous septum was found to transfix the spinal cord. There was at least one unrelated lesion that caused tethering of the spinal cord in 85% of the patients. -

Description Treatment
Description Megalencephaly, also called macrencephaly, is a condition in which an infant or child has an abnormally large, heavy, and usually malfunctioning brain. By definition, the brain weight is greater than average for the age and gender of the child. Head enlargement may be evident at birth or the head may become abnormally large in the early years of life. Megalencephaly is thought to be related to a disturbance in the regulation of cell production in the brain. In normal development, neuron proliferation - the process in which nerve cells divide to form new generations of cells - is regulated so that the correct number of cells is produced in the proper place at the appropriate time. In a megalencephalic brain, too many cells are produced either during development or progressively as part of another disorder, such as one of the neurofibromatoses or leukodystrophies. Symptoms of megalencephaly include delayed development, seizures, and corticospinal (brain cortex and spinal cord) dysfunction. Megalencephaly affects males more often than females. Unilateral megalencephaly or hemimegalencephaly is a rare condition that is characterized by the enlargement of one side of the brain. Children with this disorder may have a large, asymmetrical head accompanied by seizures, partial paralysis, and impaired cognitive development. Megalencephaly is different from macrocephaly (also called megacephaly or megalocephaly), which describes a big head, and which doesn’t necessarily indicate abnormality. Large head size is passed down through the generations in some families. Treatment There is no standard treatment for megalencephaly. Treatment will depend upon the disorder with which the megalencephaly is associated and will address individual symptoms and disabilities. -

A Anencephaly
Glossary of Birth Anomaly Terms: A Anencephaly: A deadly birth anomaly where most of the brain and skull did not form. Anomaly: Any part of the body or chromosomes that has an unusual or irregular structure. Aortic valve stenosis: The aortic valve controls the flow of blood from the left ventricle of the heart to the aorta, which takes the blood to the rest of the body. If there is stenosis of this valve, the valve has space for blood to flow through, but it is too narrow. Atresia: Lack of an opening where there should be one. Atrial septal defect: An opening in the wall (septum) that separates the left and right top chambers (atria) of the heart. A hole can vary in size and may close on its own or may require surgery. Atrioventricular septal defect (endocardial cushion defect): A defect in both the lower portion of the atrial septum and the upper portion of the ventricular septum. Together, these defects make a large opening (canal) in the middle part of the heart. Aniridia (an-i-rid-e-a): An eye anomaly where the colored part of the eye (called the iris) is partly or totally missing. It usually affects both eyes. Other parts of the eye can also be formed incorrectly. The effects on children’s ability to see can range from mild problems to blindness. To learn more about aniridia, go to the U.S. National Library of Medicine website. Anophthalmia/microphthalmia (an-oph-thal-mia/mi-croph-thal-mia): Birth anomalies of the eyes. In anophthalmia, a baby is born without one or both eyes. -

Iniencephaly: Radiological and Pathological Features of a Series of Three Cases Panduranga Chikkannaiah, V
Published online: 2019-09-25 Case Report Iniencephaly: Radiological and pathological features of a series of three cases Panduranga Chikkannaiah, V. Srinivasamurthy, B. S. Satish Prasad1, Pradeepkumar Lalyanayak, Divya N. Shivaram Department of Pathology, 1Radiology, ESIC Medical College and PGIMSR, Rajajinagar, Bangalore, Karnataka, India ABSTRACT Iniencephaly is a rare form of neural tube defect with an incidence of 0.1‑10 in 10,000 pregnancies. It is characterized by the presence of occipital bone defects at foramen magnum, fixed retroflexion of head, spinal dysmorphism, and lordosis of cervicothoracic vertebrae. It is usually associated with central nervous system, gastrointestinal, and cardiovascular anomalies. We present radiological and autopsy findings in a series of 3 cases of iniencephaly (gestational ages 29.3, 23, and 24 weeks) first fetus in addition showed omphalocele, pulmonary hypoplasia, two lobes in right lung, accessory spleen, atrial septal defect, bilateral clubfoot, ambiguous genitalia, and single umbilical artery. Second fetus was a classical case of iniencephaly apertus with spina bifida. Third fetus had colpocephaly and bifid spine. Key words: Colpocephaly, iniencephaly, omphalocele, pulmonary hypoplasia, spina bifida Introduction as her routine anomalous ultrasonogram (USG) done at a primary center revealed defective development of spine, Iniencephaly is a rare, fatal neural tube defect (NTD) atrial septal defect (ASD), aplasia of the right kidney, characterized by occipital bone defects at foramen magnum, and encephalocele. The mother’s routine blood and fixed retroflexion of head, spinal dysmorphism, and biochemical investigations were within normal limits. lordosis of cervicothoracic vertebrae.[1] Howkin and Lawrie She was not a known diabetic or hypertensive and had in 1939 classified iniencephaly into two types based on the a history of nonconsanguineous marriage. -
Basilar Invagination: Case Report and Literature Review
Accepted Manuscript Basilar Invagination: Case Report and Literature Review Nauman S. Chaudhry, MD, Alp Ozpinar, BS, Wenya Linda Bi, MD, PhD, Vamsidhar Chavakula, MD, John H. Chi, MD, MPH, Ian F. Dunn, MD PII: S1878-8750(15)00084-4 DOI: 10.1016/j.wneu.2015.02.007 Reference: WNEU 2716 To appear in: World Neurosurgery Please cite this article as: Chaudhry NS, Ozpinar A, Bi WL, Chavakula V, Chi JH, Dunn IF, Basilar Invagination: Case Report and Literature Review, World Neurosurgery (2015), doi: 10.1016/ j.wneu.2015.02.007. This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain. ACCEPTED MANUSCRIPT Basilar Invagination: Case Report and Literature Review Nauman S. Chaudhry, MD1*, Alp Ozpinar, BS2*, Wenya Linda Bi, MD, PhD1, Vamsidhar Chavakula, MD1, John H. Chi, MD, MPH1, Ian F. Dunn, MD1 1Department of Neurosurgery, Brigham and Women’s Hospital, Harvard Medical School, Boston, MA 2Department of Neurological Surgery, Oregon Health Sciences University, Portland, OR *These authors contributed equally Please address all correspondence to: Ian F. Dunn, M.D. Department of Neurosurgery Brigham and Women’s Hospital 15 Francis Street, PBB-3 Boston, MA 02115 Phone: 617-525-8371 Email: [email protected] Running Title: Anterior vs. -

Megalencephaly and Macrocephaly
277 Megalencephaly and Macrocephaly KellenD.Winden,MD,PhD1 Christopher J. Yuskaitis, MD, PhD1 Annapurna Poduri, MD, MPH2 1 Department of Neurology, Boston Children’s Hospital, Boston, Address for correspondence Annapurna Poduri, Epilepsy Genetics Massachusetts Program, Division of Epilepsy and Clinical Electrophysiology, 2 Epilepsy Genetics Program, Division of Epilepsy and Clinical Department of Neurology, Fegan 9, Boston Children’s Hospital, 300 Electrophysiology, Department of Neurology, Boston Children’s Longwood Avenue, Boston, MA 02115 Hospital, Boston, Massachusetts (e-mail: [email protected]). Semin Neurol 2015;35:277–287. Abstract Megalencephaly is a developmental disorder characterized by brain overgrowth secondary to increased size and/or numbers of neurons and glia. These disorders can be divided into metabolic and developmental categories based on their molecular etiologies. Metabolic megalencephalies are mostly caused by genetic defects in cellular metabolism, whereas developmental megalencephalies have recently been shown to be caused by alterations in signaling pathways that regulate neuronal replication, growth, and migration. These disorders often lead to epilepsy, developmental disabilities, and Keywords behavioral problems; specific disorders have associations with overgrowth or abnor- ► megalencephaly malities in other tissues. The molecular underpinnings of many of these disorders are ► hemimegalencephaly now understood, providing insight into how dysregulation of critical pathways leads to ►