U N I T 3 Records Management
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

(June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION and WHY
DRAFT EVALUATION & MANAGEMENT DOCUMENTATION GUIDELINES (June 2000) I. INTRODUCTION WHAT IS DOCUMENTATION AND WHY IS IT IMPORTANT? Medical record documentation is required to record pertinent facts, findings, and observations about an individual's health history including past and present illnesses, examinations, tests, treatments, and outcomes. The medical record chronologically documents the care of the patient and is an important element contributing to high quality care. The medical record facilitates: · the ability of the physician and other health care professionals to evaluate and plan the patient's immediate treatment, and to monitor his/her health care over time. · communication and continuity of care among physicians and other health care professionals involved in the patient's care; · accurate and timely claims review and payment; · appropriate utilization review and quality of care evaluations; and · collection of data that may be useful for research and education. An appropriately documented medical record can reduce many of the "hassles" associated with claims processing and may serve as a legal document to verify the care provided, if necessary. WHAT DO PAYERS WANT AND WHY? Because payers have a contractual obligation to enrollees, they may require reasonable documentation that services are consistent with the insurance coverage provided. They may request information to validate: · the site of service; · the medical necessity and appropriateness of the diagnostic and/or therapeutic services provided; and/or · that services provided have been accurately reported. II. GENERAL PRINCIPLES OF MEDICAL RECORD DOCUMENTATION The principles of documentation listed below are applicable to all types of medical and surgical Pg. 1 services in all settings. For Evaluation and Management (E/M) services, the nature and amount of physician work and documentation varies by type of service, place of service and the patient's status. -

Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019
Outcome and Assessment Information Set OASIS-D Guidance Manual Effective January 1, 2019 Centers for Medicare & Medicaid Services PRA Disclosure Statement According to the Paperwork Reduction Act of 1995, no persons are required to respond to a collection of information unless it displays a valid OMB control number. The valid OMB control number for this information collection is x. The time required to complete this information collection is estimated to average 0.3 minutes per response, including the time to review instructions, search existing data resources, gather the data needed, and complete and review the information collection. This estimate does not include time for training. If you have comments concerning the accuracy of the time estimate(s) or suggestions for improving this form, please write to: CMS, 7500 Security Boulevard, Attn: PRA Reports Clearance Officer, Mail Stop C4-26-05, Baltimore, Maryland 21244-1850. *****CMS Disclaimer*****Please do not send applications, claims, payments, medical records or any documents containing sensitive information to the PRA Reports Clearance Office. Please note that any correspondence not pertaining to the information collection burden approved under the associated OMB control number listed on this form will not be reviewed, forwarded, or retained. If you have questions or concerns regarding where to submit your documents, please contact Joan Proctor National Coordinator, Home Health Quality Reporting Program Centers for Medicare & Medicaid. OASIS-D Guidance Manual Table of Contents Page -

The Oral Presentation Nersi Nikakhtar, M.D
Guidelines for the Oral Presentation Nersi Nikakhtar, M.D. University of Minnesota Medical School !1 Table of Contents The Oral Presentation: An Introduction ..................................3 Why Worry About the Oral Presentation? ...............................4 Presenting the New Patient .....................................................5 The Opening Statement ......................................................5 History of Present Illness ....................................................5 Past Medical History ...........................................................6 Medications/Allergies ..........................................................7 Social and Family History ...................................................7 Review of Systems ..............................................................7 Vitals .....................................................................................8 Physical Exam .....................................................................8 Labs and Studies .................................................................8 Summary Statement ............................................................8 Assessment and Plan ..........................................................9 The Follow Up (or Daily) Presentation: What's Different? ...................................................................11 The Outpatient (Known Patient) Presentation: What's Different? ...................................................................12 !2 The Oral Presentation: An Introduction The -

Brain Pulsatility and Pulsatile Tinnitus: Clinical Types
EDITORIAL International Tinnitus Journal. 2012;17(1):2-3. Brain pulsatility and pulsatile tinnitus: clinical types The purpose of this commentary is to share our supported in the literature by animal and human studies evolving clinical experience with the tympanic membrane ongoing since 1980. The raw data analysis of the IPPA displacement (TMD) analyzer which has focused on wave in patients with nonpulsatile, predominantly central- brain pulsatility in nonpulsatile, predominantly central- type severe disabling SIT resistant to attempts for tinnitus type severe disabling subjective idiopathic tinnitus relief with instrumentation or medication are published (SIT) patients resistant to attempts for tinnitus relief with in this issue of the International Tinnitus Journal (see the instrumentation or medication. article “The Tympanic Membrane Displacement Test and One outcome of this evolving TMD experience Tinnitus”). has been the establishment of a classification system for In our experience, the extensive otologic, pulsatile tinnitus and its clinical translation for diagnosis neurotologic, and neuroradiolgical workup for pulsatile and treatment. tinnitus is frequently negative, and the etiology of the A new discipline, brain pulsatility, has been pulsation is a vascular hypothesis based predominantly emerging in the last 50-60 years, the principles of which on the clinical history and or physical examination. The are based on physical principles of matter, volume, and establishment of an accurate diagnosis and treatment pressure relationships in a confined area (i.e., brain) of pulsatile tinnitus has a satisfactory outcome to the and find clinical translation to the ear and the discipline patient and physician when a pathological process is of tinnitology - in particular, pulsatile tinnitus. -

Coding Tips For: PROGRESS NOTE CONTENTS
Coding tips for: PROGRESS NOTE CONTENTS PREFERRED FORMAT, PER CMS, IS THE S.O.A.P. FORMAT: SUBJECTIVE: This section should be utilized to report subjective information of clinical significance. The chief complaint of the patient belongs in this section. OBJECTIVE: This section is where you will report the measurable and observable information that you obtain during the visit. Review of systems, physical examination, any test results, outside communications with specialists should be noted in this section. ASSESSMENT: List all diagnoses and conditions assessed during the visit. Include any conditions for which prescriptions were given/renewed, tests were ordered, referrals were given. Also include any conditions in which affected decision-making for treatment. PLAN: The final section of your SOAP notes is where you outline the course of treatment, after considering the information you gathered during the visit. e text box anywhere in the document. Use the Text Box Tools tab to change the formatting of the pull quote text box.] Coding tips for: ASSURE PROGRESS NOTE COMPLIANCE The physician’s signature must be on all progress notes If the physician does not include his/her credentials as part of their signature, the full name and credentials must be printed clearly on the note The patient’s name, date of birth and DOS must be on each page of the patient’s progress note/chart Electronic Medical Records must clearly be “authenticated", “digitally signed”, “electronically signed by” the provider The medical record must be legible/complete Only standard medical abbreviations should be used Late entries can be made to clarify confirmed diagnoses. -

The Patient Interview
CHAPTER 1 The Patient Interview Sneha Baxi Srivastava, PharmD, BCACP LEARNING OBJECTIVES • Explain the basic communication skills needed when performing a patient interview. • Describe the components of the patient interview. • Conduct a thorough medication history. • Compare and contrast the different patient interview approaches in various clinical settings. • Adapt the interview technique based on the needs of the patient. KEY TERMS • Active Listening • Pertinent Positive • Rapport • Pertinent Negative • Empathy • Past History • Open-Ended Questions • Medication History • Leading Questions • Family History • Probing Questions • Personal and Social History • Nonverbal Communication • Review of Systems • Chief Complaint • Physical Exam • History of Present Illness • QuEST/SCHOLAR-MAC INTRODUCTION The patient interview is the primary way of obtaining comprehensive information about the patient in order to provide effective patient-centered care, and the medica- tion history component is the pharmacist’s expertise. A methodological approach is used to obtain information from the patient, usually starting with determining the patient’s chief complaint, also known as the reason for the healthcare visit, and then 2 CHAPTER 1 / The Patient Interview delving further into an exploration of the patient’s specific complaint and problem. A comprehensive patient interview includes inquiring about the patient’s medical, medication, social, personal, and family history, as well as a thorough review of systems and possibly a physical examination. The medication history is the part of the patient interview that provides the pharmacist the opportunity to utilize his or her expertise by precisely collecting each component of the medication history (however, a medication history may also be collected independent of a comprehensive patient interview). -

Medical Terminology Information Sheet
Medical Terminology Information Sheet: Medical Chart Organization: • Demographics and insurance • Flow sheets • Physician Orders Medical History Terms: • Visit notes • CC Chief Complaint of Patient • Laboratory results • HPI History of Present Illness • Radiology results • ROS Review of Systems • Consultant notes • PMHx Past Medical History • Other communications • PSHx Past Surgical History • SHx & FHx Social & Family History Types of Patient Encounter Notes: • Medications and medication allergies • History and Physical • NKDA = no known drug allergies o PE Physical Exam o Lab Laboratory Studies Physical Examination Terms: o Radiology • PE= Physical Exam y x-rays • (+) = present y CT and MRI scans • (-) = Ф = negative or absent y ultrasounds • nl = normal o Assessment- Dx (diagnosis) or • wnl = within normal limits DDx (differential diagnosis) if diagnosis is unclear o R/O = rule out (if diagnosis is Laboratory Terminology: unclear) • CBC = complete blood count o Plan- Further tests, • Chem 7 (or Chem 8, 14, 20) = consultations, treatment, chemistry panels of 7,8,14,or 20 recommendations chemistry tests • The “SOAP” Note • BMP = basic Metabolic Panel o S = Subjective (what the • CMP = complete Metabolic Panel patient tells you) • LFTs = liver function tests o O = Objective (info from PE, • ABG = arterial blood gas labs, radiology) • UA = urine analysis o A = Assessment (Dx and DDx) • HbA1C= diabetes blood test o P = Plan (treatment, further tests, etc.) • Discharge Summary o Narrative in format o Summarizes the events of a hospital stay -
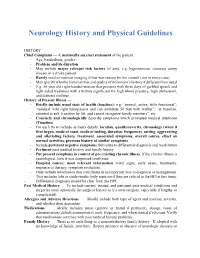
Neurology History and Physical Guidelines
Neurology History and Physical Guidelines HISTORY Chief Complaint — A maximally succinct statement of the patient: - Age, handedness, gender - Problem and its duration - May include major relevant risk factors (if any), e.g. hypertension, coronary artery disease in a stroke patient. - Rarely need to mention imaging if that was reason for the consult (not in every case) - May specify who the historian was and quality of informant’s history if different from usual - E.g: 56 year old right-handed woman that presents with three days of garbled speech and right sided weakness with a history significant for high blood pressure, high cholesterol, and diabetes mellitus History of Present Illness — - Briefly include usual state of health (baseline): e.g: “normal, active, fully functional”; “residual mild right hemiparesis and can ambulate 50 feet with walker”; “at baseline, oriented to self, transfers by lift, and cannot recognize family members”, etc. - Concisely and chronologically describe symptoms which prompted medical attentions (Timeline) - For each try to include as many details: location, quality/severity, chronology (when it first began, mode of onset, mode of ending, duration, frequency), setting, aggravating and alleviating factors, treatment, associated symptoms, overall course, effect on normal activities, previous history of similar symptoms - Include pertinent negative symptoms that relate to differential diagnosis and localization - Pertinent past medical history and family history - Put present symptoms in context of pre-existing chronic illness. If the chronic illness is neurological, how it was diagnosed/confirmed - Hospital course: most relevant information (vital signs, early exam, treatments, response to therapy, symptom evolution) - Only include information that contributes in an important way to diagnosis or management. -
The AOA Guide
The AOA Guide: How to Succeed in the Third-Year Clerkships Example Notes for the MSIII 2014 Preface This guide was created as a way of assisting you as you start your clinical training. For the rest of your professional life you will write various notes, and although they eventually become second nature to you, it is often challenging at first to figure out what information is pertinent to a particular specialty/rotation.This book is designed to help you through that process. In this book you will find samples of SOAP notes for each specialty and a complete History and Physical. Each of these notes represents very typical patients you will see on the rotation. Look at the way the notes are phrased and the information they contain. We have included an abbreviations page at the end of this book so that you can refer to it for the short-forms with which you are not yet familiar. Pretty soon you will be using these abbreviations without a problem! These notes can be used as a template from which you can adjust the information to apply to your patient. It is important to remember that these notes are not all inclusive, of course, and other physicians will give suggestions that you should heed. If you are having trouble, remember there is usually a fourth year medical student on the rotation somewhere, too. We are always willing to help! Table of Contents Internal Medicine Progress Note (SOAP) ............................................................3 Neurology Progress Note (SOAP) ....................................................................... 5 Surgery ................................................................................................................. 7 Progress Note (SOAP) .................................................................................... 7 Pre-Operative Note ........................................................................................ -
The AOA Guide
The AOA Guide: How to Succeed in the Third-Year Clerkships Example Notes for the MSIII 2017 Preface This guide was created as a way of assisting you as you start your clinical training. For the rest of your professional life, you will write various notes. Although they will eventually become second nature to you, it is often challenging at first to figure out what information is pertinent to a particular specialty/rotation.This book is designed to help you through that process. In this book you will find samples of SOAP notes for each specialty and a complete History and Physical. Each of these notes represents very typical patients you will see on the rotation. Look at the way the notes are phrased and the information they contain. We have included an abbre- viations page at the end of this book so that you can refer to it for the short-forms with which you are not yet familiar. Pretty soon you will be using these abbrevia- tions without a problem! These notes can be used as a template from which you can adjust the information to apply to your patient. It is important to remember that these notes are not all inclusive, of course, and other physicians will give sugges- tions that you should heed. If you are ever having trouble, us fourth year medical students are always willing to help! ***NOTE: Many note-writing practices at Jefferson may change as the hospital transitions from paper notes to EMR.*** Table of Contents Internal Medicine Progress Note (SOAP) ............................................................3 Neurology Progress Note (SOAP) ...................................................................... -

EHR Go Guide: the Notes Tab
EHR Go Guide: The Notes Tab Introduction The Notes tab in the EHR contains narrative information about a patient’s current and past medical history. It is where all members of the health care team communicate about the patient during a hospital visit or while receiving outpatient care. Notes are documented on regular intervals about clinical events related to the diagnoses and treatment of the patient. There are many types of notes in the EHR including: admission notes, assessments, SOAP notes, exams, reports, screening tools, progress notes, evaluations, and more. Notes are sometimes referred to as “Flow Sheets.” Most note options are templated, meaning specific fields or questions are built in to the note for the clinician to answer, while other notes allow for free-text narrative entry. Case patients in EHR Go have existing notes in their chart. You may review these notes to gather detailed information about the patient’s condition. It is often helpful to review the patient’s notes first, to learn about the patient, before reviewing the information in the other EHR tabs. In some activities, you’ll need to write a new note. This guide explains how to access and review existing notes, edit notes, and create new notes. Additional resources Please refer to the Student Guide to EHR Go for information on logging in to Go and launching the EHR for an activity. FAQs about notes 1. Can I edit a note after I have finished it? a. Yes. In EHR Go, you may edit any existing note as often as needed. See Editing a Note section. -

Progress Notes and Psychotherapy Notes
Progress Notes and Psychotherapy Notes This Appendix covers two kinds of notes written about psychotherapy—progress notes and psychotherapy notes—and highlights the practical value of this important distinction. Progress notes are part of the client record or file, as noted below. Psychotherapy notes are not part of the file. After an overview of the client file or record, the difference between these two kinds of notes is discussed along with guides for writing progress notes. The Client File or Record The record or file of a client’s treatment at the Clinic consists of: Contact information Informed consent for treatment (including notification of rights) An intake report and/or, A written treatment plan or case formulation based on an initial assessment (i.e. interview information, formal assessment if used, and any other information collected from other sources) Progress notes documenting treatment, filed in reverse chronological order on the Clinic form Progress Note A termination note when work is concluded Other materials such as releases of information, test protocols, information obtained from other sources and so forth. The file or record does not contain psychotherapy notes (see below). Another way of saying this is that if it’s in the file, it’s not a psychotherapy note. As context for progress notes versus psychotherapy notes, please also refer to the form in Appendix D Brief Summary of Client Rights to Privacy and Access to Records and Consent to Behavioral Health Treatment and to the document in that appendix entitled Protecting the Privacy of Your Behavioral Health Information. A general intake outline is contained in Appendix C-4 Intake Outline and Report which can serve to organize information and begin treatment planning.