NORTH – NANSON CLINICAL MANUAL “The Red Book”
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

International Journal of Medical and Health Sciences
International Journal of Medical and Health Sciences Journal Home Page: http://www.ijmhs.net ISSN:2277-4505 Review article Examining the liver – Revisiting an old friend Cyriac Abby Philips1*, Apurva Pande2 1Department of Hepatology and Transplant Medicine, PVS Institute of Digestive Diseases, PVS Memorial Hospital, Kaloor, Kochi, Kerala, India, 2Department of Hepatology, Institute of Liver and Biliary Sciences, D-1, Vasant Kunj, New Delhi, India. ABSTRACT In the current era of medical practice, super saturated with investigations of choice and development of diagnostic tools, clinical examination is a lost art. In this review we briefly discuss important aspects of examination of the liver, which is much needed in decision making on investigational approach. We urge the new medical student or the newly practicing physician to develop skills in clinical examination for resourceful management of the patient. KEYWORDS: Liver, examination, clinical skills, hepatomegaly, chronic liver disease, portal hypertension, liver span INTRODUCTION respiration, the excursion of liver movement is around 2 to 3 The liver attains its adult size by the age of 15 years. The cm. Castell and Frank has elegantly described normal liver liver weighs 1.2 to 1.4 kg in women and 1.4 to 1.5 kg in span in men and women utilizing the percussion method men. The liver seldom extends more than 5 cm beyond the (Table 1). Accordingly, the mean liver span is 10.5 cm for midline towards the left costal margin. During inspiration, men and 7 cm in women. During examination, a span 2 to 3 the diaphragmatic exertion moves the liver downward with cm larger or smaller than these values is considered anterior surface rotating to the right. -
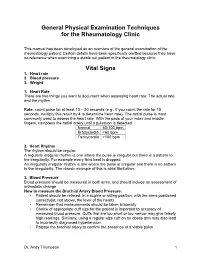
General Physical Examination Skills for Ahps
General Physical Examination Techniques for the Rheumatology Clinic This manual has been developed as an overview of the general examination of the rheumatology patient. Certain details have been specifically omitted because they have no relevance when examining a stable out patient in the rheumatology clinic. Vital Signs 1. Heart rate 2. Blood pressure 3. Weight 1. Heart Rate There are two things you want to document when assessing heart rate: The actual rate and the rhythm. Rate: count pulse for at least 15 – 30 seconds (e.g., if you count the rate for 15 seconds, multiply this result by 4 to determine heart rate). The radial pulse is most commonly used to assess the heart rate. With the pads of your index and middle fingers, compress the radial artery until a pulsation is detected. Normal 60-100 bpm Bradycardia <60 bpm Tachycardia >100 bpm 2. Heart Rhythm The rhythm should be regular. A regularly irregular rhythm is one where the pulse is irregular but there is a pattern to the irregularity. For example every third beat is dropped. An irregularly irregular rhythm is one where the pulse is irregular and there is no pattern to the irregularity. The classic example of this is atrial fibrillation. 3. Blood Pressure Blood pressure should be measured in both arms, and should include an assessment of orthostatic change How to measure the Brachial Artery Blood Pressure: • Patient should be relaxed, in a supine or sitting position, with the arms positioned correctly(at, not above, the level of the heart) • Remember that measurements should be taken bilaterally • Choice of appropriate cuff size for the patient is important to accuracy of measured blood pressure. -

HEENT EXAMINIATION ______HEENT Exam Exam Overview
HEENT EXAMINIATION ____________________________________________________________ HEENT Exam Exam Overview I. Head A. Visual inspection B. Palpation of scalp II. Eyes A. Visual Acuity B. Visual Fields C. Extraocular Movements/Near Response D. Inspection of sclera & conjunctiva E. Pupils F. Ophthalmoscopy III. Ears A. External Inspection B. Otoscopy C. Hearing Acuity D. Weber/Rinne IV. Nose A. External Inspection B. Speculum/otoscope C. Sinus areas V. Throat/Mouth A. Mouth Examination B. Pharynx Examination C. Bimanual Palpation VI. Neck A. Lymph nodes B. Thyroid gland 29 HEENT EXAMINIATION ____________________________________________________________ HEENT Terms Acuity – (ehk-yu-eh-tee) sharpness, clearness, and distinctness of perception or vision. Accommodation - adjustment, especially of the eye for seeing objects at various distances. Miosis – (mi-o-siss) constriction of the pupil of the eye, resulting from a normal response to an increase in light or caused by certain drugs or pathological conditions. Conjunctiva – (kon-junk-ti-veh) the mucous membrane lining the inner surfaces of the eyelids and anterior part of the sclera. Sclera – (sklehr-eh) the tough fibrous tunic forming the outer envelope of the eye and covering all of the eyeball except the cornea. Cornea – (kor-nee-eh) clear, bowl-shaped structure at the front of the eye. It is located in front of the colored part of the eye (iris). The cornea lets light into the eye and partially focuses it. Glaucoma – (glaw-ko-ma) any of a group of eye diseases characterized by abnormally high intraocular fluid pressure, damaged optic disk, hardening of the eyeball, and partial to complete loss of vision. Conductive hearing loss - a hearing impairment of the outer or middle ear, which is due to abnormalities or damage within the conductive pathways leading to the inner ear. -

Utility of the Digital Rectal Examination in the Emergency Department: a Review
The Journal of Emergency Medicine, Vol. 43, No. 6, pp. 1196–1204, 2012 Published by Elsevier Inc. Printed in the USA 0736-4679/$ - see front matter http://dx.doi.org/10.1016/j.jemermed.2012.06.015 Clinical Reviews UTILITY OF THE DIGITAL RECTAL EXAMINATION IN THE EMERGENCY DEPARTMENT: A REVIEW Chad Kessler, MD, MHPE*† and Stephen J. Bauer, MD† *Department of Emergency Medicine, Jesse Brown VA Medical Center and †University of Illinois-Chicago College of Medicine, Chicago, Illinois Reprint Address: Chad Kessler, MD, MHPE, Department of Emergency Medicine, Jesse Brown Veterans Hospital, 820 S Damen Ave., M/C 111, Chicago, IL 60612 , Abstract—Background: The digital rectal examination abdominal pain and acute appendicitis. Stool obtained by (DRE) has been reflexively performed to evaluate common DRE doesn’t seem to increase the false-positive rate of chief complaints in the Emergency Department without FOBTs, and the DRE correlated moderately well with anal knowing its true utility in diagnosis. Objective: Medical lit- manometric measurements in determining anal sphincter erature databases were searched for the most relevant arti- tone. Published by Elsevier Inc. cles pertaining to: the utility of the DRE in evaluating abdominal pain and acute appendicitis, the false-positive , Keywords—digital rectal; utility; review; Emergency rate of fecal occult blood tests (FOBT) from stool obtained Department; evidence-based medicine by DRE or spontaneous passage, and the correlation be- tween DRE and anal manometry in determining anal tone. Discussion: Sixteen articles met our inclusion criteria; there INTRODUCTION were two for abdominal pain, five for appendicitis, six for anal tone, and three for fecal occult blood. -

A Neurological Examination
THE 3 MINUTE NEUROLOGICAL EXAMINATION DEMYSTIFIED Faculty: W.J. Oczkowski MD, FRCPC Professor and Academic Head, Division of Neurology, Department of Medicine, McMaster University Stroke Neurologist, Hamilton Health Sciences Relationships with commercial interests: ► Not Applicable Potential for conflict(s) of interest: ► Not Applicable Mitigating Potential Bias ► All the recommendations involving clinical medicine are based on evidence that is accepted within the profession. ► All scientific research referred to, reported, or used is in the support or justification of patient care. ► Recommendations conform to the generally accepted standards. ► Independent content validation. ► The presentation will mitigate potential bias by ensuring that data and recommendations are presented in a fair and balanced way. ► Potential bias will be mitigated by presenting a full range of products that can be used in this therapeutic area. ► Information of the history, development, funding, and the sponsoring organizations of the disclosure presented will be discussed. Objectives ► Overview of neurological assessment . It’s all about stroke! . It’s all about the chief complaint and history. ► Overview: . 3 types of clinical exams . Neurological signs . Neurological localization o Pathognomonic signs o Upper versus lower motor neuron signs ► Cases and practice Bill ► 72 year old male . Hypertension . Smoker ► Stroke call: dizzy, facial droop, slurred speech ► Neurological Exam: . Ptosis and miosis on left . Numb left face . Left palatal weakness . Dysarthria . Ataxic left arm and left leg . Numb right arm and leg NIH Stroke Scale Score ► LOC: a,b,c_________________ 0 ► Best gaze__________________ 0 0 ► Visual fields________________ 0 ► Facial palsy________________ 0 ► Motor arm and leg__________ -Left Ptosis 2 -Left miosis ► Limb ataxia________________ -Weakness of 1 ► Sensory_______________________ left palate ► Best Language______________ 0 1 ► Dysarthria_________________ 0 ► Extinction and inattention____ - . -

CASE REPORT 48-Year-Old Man
THE PATIENT CASE REPORT 48-year-old man SIGNS & SYMPTOMS – Acute hearing loss, tinnitus, and fullness in the left ear Dennerd Ovando, MD; J. Walter Kutz, MD; Weber test lateralized to the – Sergio Huerta, MD right ear Department of Surgery (Drs. Ovando and Huerta) – Positive Rinne test and and Department of normal tympanometry Otolaryngology (Dr. Kutz), UT Southwestern Medical Center, Dallas; VA North Texas Health Care System, Dallas (Dr. Huerta) Sergio.Huerta@ THE CASE UTSouthwestern.edu The authors reported no A healthy 48-year-old man presented to our otolaryngology clinic with a 2-hour history of potential conflict of interest hearing loss, tinnitus, and fullness in the left ear. He denied any vertigo, nausea, vomiting, relevant to this article. otalgia, or otorrhea. He had noticed signs of a possible upper respiratory infection, including a sore throat and headache, the day before his symptoms started. His medical history was unremarkable. He denied any history of otologic surgery, trauma, or vision problems, and he was not taking any medications. The patient was afebrile on physical examination with a heart rate of 48 beats/min and blood pressure of 117/68 mm Hg. A Weber test performed using a 512-Hz tuning fork lateral- ized to the right ear. A Rinne test showed air conduction was louder than bone conduction in the affected left ear—a normal finding. Tympanometry and otoscopic examination showed the bilateral tympanic membranes were normal. THE DIAGNOSIS Pure tone audiometry showed severe sensorineural hearing loss in the left ear and a poor speech discrimination score. The Weber test confirmed the hearing loss was sensorineu- ral and not conductive, ruling out a middle ear effusion. -

The Older Adult 20
CHAPTER The Older Adult 20 Older adults now number more than 25 million people in the United States and are expected to reach 80 million by 2050.1 These seniors will live longer than previous generations: life span at birth is currently 79 years for women and 74 years for men. Those older than 85 years are projected to increase to 5% of the U.S. population within 40 years. Hence, the “demographic im- perative” is to maximize not only the life span but also the “health span” of our older population, so that seniors maintain full function for as long as possible, enjoying rich and active lives in their homes and communities. Clinicians now recognize frailty as one of society’s common myths about aging—more than 95% of Americans older than 65 years live in the commu- nity, and only 5% reside in long-term care facilities.1,2 Over the past 20 years, seniors actually have become more active and less disabled. These changes call for new goals for clinical care—“an informed activated patient inter- acting with a prepared proactive team, resulting in high quality satisfying en- counters and improved outcomes”3—and a distinct set of clinical attitudes and skills. CHAPTER 20 I THE OLDER ADULT 839 ANATOMY AND PHYSIOLOGY Assessing the older adult presents special opportunities and special challenges. Many of these are quite different from the disease-oriented approach of his- tory taking and physical examination for younger patients: the focus on healthy or “successful” aging; the need to understand and mobilize family, social, and community supports; the importance of skills directed to func- tional assessment, “the sixth vital sign”; and the opportunities for promoting the older adult’s long-term health and safety. -
Bates' Pocket Guide to Physical Examination and History Taking
Lynn S. Bickley, MD, FACP Clinical Professor of Internal Medicine School of Medicine University of New Mexico Albuquerque, New Mexico Peter G. Szilagyi, MD, MPH Professor of Pediatrics Chief, Division of General Pediatrics University of Rochester School of Medicine and Dentistry Rochester, New York Acquisitions Editor: Elizabeth Nieginski/Susan Rhyner Product Manager: Annette Ferran Editorial Assistant: Ashley Fischer Design Coordinator: Joan Wendt Art Director, Illustration: Brett MacNaughton Manufacturing Coordinator: Karin Duffield Indexer: Angie Allen Prepress Vendor: Aptara, Inc. 7th Edition Copyright © 2013 Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2009 by Wolters Kluwer Health | Lippincott Williams & Wilkins. Copyright © 2007, 2004, 2000 by Lippincott Williams & Wilkins. Copyright © 1995, 1991 by J. B. Lippincott Company. All rights reserved. This book is protected by copyright. No part of this book may be reproduced or transmitted in any form or by any means, including as photocopies or scanned-in or other electronic copies, or utilized by any information storage and retrieval system without written permission from the copyright owner, except for brief quotations embodied in critical articles and reviews. Materials appear- ing in this book prepared by individuals as part of their official duties as U.S. government employees are not covered by the above-mentioned copyright. To request permission, please contact Lippincott Williams & Wilkins at Two Commerce Square, 2001 Market Street, Philadelphia PA 19103, via email at [email protected] or via website at lww.com (products and services). 9 8 7 6 5 4 3 2 1 Printed in China Library of Congress Cataloging-in-Publication Data Bickley, Lynn S. Bates’ pocket guide to physical examination and history taking / Lynn S. -
Bitemedicine.Com/Watch
Aims and Objectives • Requires some basic knowledge of clinical examinations • Clinical examination station (OSCE) • Abdominal examination: 4 cases • Duration: 70 mins • Slides and recordings: www.bitemedicine.com/watch • Other common OSCE cases available in previous and upcoming webinars • Aim of the week is to cover most of the common scenarios 2 Abdominal examination: OSCE Cases list What cases could come up? 1. Renal transplantation (+ AV fistula) 2. Stoma 3. Chronic liver disease 4. Hepatosplenomegaly 5. Cushing’s syndrome This is not an exhaustive list • But by preparing for these you will be better at: • Your exam routine • Looking out for important signs • Formulating your findings systematically • Tackling the VIVA 3 How to present your findings? I performed an abdominal examination on this patient If you have an idea, then • Who has signs suggestive of XXX back yourself from the start. It gets the examiner listening My main positive findings are: 1. XXX 2. YYY My relevant negative findings are: RELEVANT negatives 1. XXX (Risk factors) 2. YYY (Signs of decompensation) 3. ZZZ (POSSIBLE associated features) Overall, this points towards a diagnosis of XXX with no signs of decompensation 4 Abdominal examination: Case 1 Background 65M Central (1) (2) • Palpable mass in the left iliac fossa Bedside/peripheral Tacrolimus 5 Question 1 Q1 Q2 What is the most likely diagnosis? Chronic kidney disease Diabetic nephropathy resulting in renal transplantation Tacrolimus-induced nephropathy resulting in renal transplantation Hypertensive nephropathy -

Breast Carcinoma in Axillary Tail of Spence: a Rare Case Report
International Journal of Current Research and Review Case Report DOI: http://dx.doi.org/10.31782/IJCRR.2020.9295 Breast Carcinoma in Axillary Tail of Spence: A Rare Case Report IJCRR 1 2 3 4 Section: Healthcare Rajesh Domkunti , Yashwant R. Lamture , Avinash Rinait , Dilip Gode Sci. Journal Impact Factor: 6.1 (2018) 1 2 ICV: 90.90 (2018) Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Wardha-442001; Professor and HOD Dept. of Surgery, Datta Meghe Medical College Nagpur, Shalinitai Meghe Hospital and Research Centre, Nagpur-441110; 3Assistant Professor Dept. of Surgery, Datta Meghe Medical College Nagpur, Shalinitai Meghe Hospital and Research Centre, Nagpur-441110; 4Dean & Professor Dept. of Surgery, Datta Meghe Medical College Nagpur, Shalinitai Meghe Hospital and Research Centre, Nagpur-441110 ABSTRACT . Breast carcinoma is known to be one of the commonest malignant tumours among which Axillary breast cancer is a special individual that accounts for 0.1% to 2% of all cases of breast cancer. This is usually composed of poorly differentiated IDC with squamous or mesenchymal carcinoma areas sometimes. Axillary malignancy is difficult as there are many differential diagnoses that may require careful evaluation. This is a case report on Breast carcinoma of tail of Spence in axilla with skin involvement near nipple-areola complex whose histopathology was suggestive of infiltrating ductal carcinoma of axillary tail of Spence with mild dysplastic changes over right nipple-areola complex and high lymph node positivity (96.7%). Standard investigations like Ultrasonography of B/L Breast with Axilla and Tru-cut biopsy were done to reach the diagnosis of Intraductal Carcinoma (IDC) of the axillary tail. -

GYNECOLOGY Helen B. Albano, MD, FPOGS Medical History • The
GYNECOLOGY Only one Helen B. Albano, MD, FPOGS Reason for admission Common gynecological complaints Medical History o Bleeding (vaginal) The quality of the medical care provided by the o Pain (specify: use 9 regions of abdomen) physician o Mass (abdominal or pelvic) Type of relationship between physician and the o Vaginal discharge patient o Urinary or GI symptoms Can be determined largely the depth of o o Protrusion out of the vagina gynecological history o Infertility Patient-Doctor Relationship o Complete history HPI (History of Present Illness) o Complete PE Refers to the chief complaint o Labs o Duration New Patient o Severity o Take Time o Precipitating factors . Obtain comprehensive history o Occurrence in relation to other events . Perform comprehensive PE . Menstrual cycle o Establish data base, along with DPR basd on . Voiding a good communication . Bowel movements Old Patient or the established patient History of similar symptoms Updates o Outcome of previous therapies . Gynecological changes Impact on the patient’s: . Pregnancy history o Quality of life . Additional surgery, accidents or new o Self-image medications o Relationship with the family (sexual history to husband) History Taking o Daily activities Overview o Most important part of gynecological Menstrual History evaluation Age of menarche o Provides tentative diagnosis (impression) Date of onset of menstrual periods before PE Duration and quantity (i.e. number of pads used per o LEGAL document . Subject to subpoena, may be day) of flow defended in court Degree of Discomfort Premenstrual symptoms General Data Cycle Name o Counted from the first day of menstrual flow Age of one cycle to the first day of menstrual Gravidity (G) flow of the next o State of being pregnant Range of normal is wide Normal range of ovulatory cycles Parity (P) o . -

The Newborn Physical Examination Joan Richardson's Assessment of A
The Newborn Physical Examination Assessment of a Newborn with Joan Richardson Joan Richardson's Assessment of a Newborn What follows is a demonstration of the physical examination of a newborn baby as well as the determination of the gestational age of the baby using the Dubowitz examination. Dubowitz examination From L.M. Dubowitz et al, Clinical assessment of gestational age in the newborn infant. Journal of Pediatrics 77-1, 1970, with permission Skin Color When examining a newborn baby, start by closely observing the baby. Observe the color. Is the baby pink or cyanotic? The best place to observe is the lips or tongue. If those are nice and pink then baby does not have cyanosis. The most unreliable places to observe for cyanosis are the fingers and toes because babies frequently have poor blood circulation to the extremities and this results in acrocyanosis.(See video below of baby with cyanotic feet) Also observe the baby for any obvious congenital malformations or any obvious congenital anomalies. Be sure to count the number of fingers and toes. Cyanotic Feet The most unreliable places to observe for cyanosis are the fingers and toes because babies frequently have poor blood circulation to the extremities and this results in a condition called acrocyanosis. Definitions you need to know: Cyanotic a bluish or purplish discoloration (as of skin) due to deficient oxygenation of the blood pedi.edtech - a faculty development program with support from US Dept. Health & Human Services, Health Resources and Services Administration, Bureau of Health Professions create 6/24/2015; last modified date 11/23/2015 Page 1 of 12 acrocyanosis Blueness or pallor of extremities, normal sign of vasomotor instability characterized by color change limited to the peripheral circulation.