Urinary Tract Eod Stage & Treatment
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Urinary System Dr
The urinary System Dr. Ali Ebneshahidi Functions of the Urinary System • Excretion – removal of waste material from the blood plasma and the disposal of this waste in the urine. • Elimination – removal of waste from other organ systems - from digestive system – undigested food, water, salt, ions, and drugs. + - from respiratory system – CO2,H , water, toxins. - from skin – water, NaCl, nitrogenous wastes (urea , uric acid, ammonia, creatinine). • Water balance -- kidney tubules regulate water reabsorption and urine concentration. • regulation of PH, volume, and composition of body fluids. • production of Erythropoietin for hematopoieseis, and renin for blood pressure regulation. Anatomy of the Urinary System Gross anatomy: • kidneys – a pair of bean – shaped organs located retroperitoneally, responsible for blood filtering and urine formation. • Renal capsule – a layer of fibrous connective tissue covering the kidneys. • Renal cortex – outer region of the kidneys where most nephrons is located. • Renal medulla – inner region of the kidneys where some nephrons is located, also where urine is collected to be excreted outward. • Renal calyx – duct – like sections of renal medulla for collecting urine from nephrons and direct urine into renal pelvis. • Renal pyramid – connective tissues in the renal medulla binding various structures together. • Renal pelvis – central urine collecting area of renal medulla. • Hilum (or hilus) – concave notch of kidneys where renal artery, renal vein, urethra, nerves, and lymphatic vessels converge. • Ureter – a tubule that transport urine (mainly by peristalsis) from the kidney to the urinary bladder. • Urinary bladder – a spherical storage organ that contains up to 400 ml of urine. • Urethra – a tubule that excretes urine out of the urinary bladder to the outside, through the urethral orifice. -

Laboratory 8 - Urinary and Reproductive Systems
Laboratory 8 - Urinary and Reproductive Systems Urinary System Please read before starting: It is easy to damage the structures of the reproductive system as you expose structures associated with excretion, so exercise caution as you do this. Please also note that we will have drawings available as well to help you find and identify the structures described below. The major blood vessels serving the kidneys are the Renal renal artery and the renal pyramid vein., which are located deep in the parietal peritoneum. The renal artery is a branch of the dorsal aorta that comes off Renal further caudal than the cranial pelvis mesenteric artery. Dissect the left kidney in situ, dividing it into dorsal and ventral portions by making a frontal section along the outer periphery. Observe the renal cortex renal medulla (next layer in) renal pyramids renal pelvis ureter (see above diagram) The kidneys include a variety of structures including an arterial supply, a venous return, extensive capillary networks around each nephron and then, of course, the filtration and reabsorption apparatus. These structures are primarily composed of nephrons (the basic functional unit of the kidney) and the ducts which carry urine away from the nephron (the collecting ducts and larger ducts eventually draining these into the ureters from each kidney. The renal pyramids contain the extensions of the nephrons into the renal medulla (the Loops of Henle) and the collecting ducts. Urine is eventually emptied into the renal pelvis before leaving the kidneys in the ureters. The ureters leaves the kidneys medially at approximately the midpoint of the organs and then run caudal to the urinary bladder. -

Urinary System: Summary Stage 2018 Coding Manual V2.0
URINARY SYSTEM BLADDER, RENAL PELVIS AND URETERS ANATOMIC STRUCTURES Table of Anatomic Structures MUCOSA MUSCULARIS PRIMARY SITE -Epithelium SEROSA PROPRIA -Lamina propria submucosa Yes, on superior Bladder (C67_) Yes Yes surface Renal pelvis (C659) Yes Yes No Ureter (C669) Yes Yes No The layers of the urinary tract include: 1. The EPITHELIAL LAYER contains no blood vessels or lymphatics 2. The BASEMENT MEMBRANE, a sheet of extracellular material, functions as a filtration barrier and a boundary involved in generating and maintaining tissue structure 3. The LAMINA PROPRIA, composed of areolar connective tissue, contains blood vessels, nerves, and, in some regions, glands. Once tumor has broken through the basement membrane into the lamina propria, it can spread by way of the lymphatics and blood vessels to other parts of the body 4. The urinary sites do NOT have a MUSCULARIS MUCOSAE, and, therefore, the lamina propria and the submucosa are difficult to separate. These terms are used interchangeably 5. The SUBMUCOSA is a thick layer of either dense or areolar connective tissue. It contains blood vessels, lymphatic vessels, nerves, and, in some regions, glands 6. The MUSCULARIS PROPRIA is composed of multiple layers of muscle tissue; it constitutes the wall of the organ 7. The SEROSA, the outermost layer covering, is a serous membrane, part of the visceral peritoneum. It covers only the superior surface of the bladder. There is no serosa on the renal pelvis or ureters. a. Where there is no serosa, the connective tissue of surrounding structures merges with the connective tissue of the urinary organs and is called ADVENTITIA. -

URINARY SYSTEM Components
Human Anatomy Unit 3 URINARY SYSTEM Components • Kidneys • Ureters • Urinary bladder • Urethra Funcons • Storage of urine – Bladder stores up to 1 L of urine • Excreon of urine – Transport of urine out of body • Regulaon: – Plasma pH – Blood volume/pressure – Plasma ion concentraons (Ca2+, Na+, K+, CL-) – Assist liver in detoxificaon, amino acid metabolism Kidney Gross Anatomy • Retroperitoneal – Anterior surface covered with peritoneum – Posterior surface directly against posterior abdominal wall • Superior surface at about T12 • Inferior surface at about L3 • Ureters enter urinary bladder posteriorly • LeT kidney 2cm superior to right – Size of liver Structure of the Kidney • Hilum = the depression along the medial border through which several structures pass – renal artery – renal vein – ureter – renal nerves Surrounding Tissue • Fibrous capsule – Innermost layer of dense irregular CT – Maintains shape, protec:on • Adipose capsule – Adipose ct of varying thickness – Cushioning and insulaon • Renal fascia – Dense irregular CT – Anchors kidney to peritoneum & abdominal wall • Paranephric fat – Outermost, adipose CT between renal fascia and peritoneum Frontal Sec:on of the Kidney • Cortex – Layer of renal :ssue in contact with capsule – Renal columns – parts of cortex that extend into the medulla between pyramids • Medulla – Striped due to renal tubules • Renal pyramids – 8-15 present in medulla of adult – Conical shape – Wide base at cor:comedullary juncon Flow of Filtrate/Urine • Collec:ng ducts – Collect from mul:ple nephrons • Minor calyx – Collect from each pyramid • Major calyx – Collect from minor calyx • Renal pelvis – Collects from calyces, passes onto • Ureter – Collects from pelvis • Urinary Bladder – Collects from ureters Histology Renal Cortex Renal Medulla Renal Tubules • Nephron – func:onal unit of the kidney. -
Introduction to the Urinary System
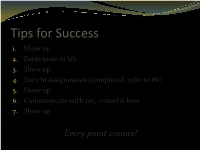
Tips for Success 1. Show up 2. Participate in lab 3. Show up 4. Turn in assignments (completed, refer to #6) 5. Show up 6. Communicate with me, e-mail is best 7. Show up Every point counts! Business Homework due in lab Label the handout provided today Front and back Use your book! There should be at least 18 items labeled Part 1 Urinary System Wastes Gases versus fluids Urinary system Dispose of water soluble wastes Electrolyte regulation Acid-base regulation Urinary System Other functions Kidneys Renin Erythropoietin Vitamin D activation Nitrogenous Wastes Urine is about 95% water Second largest component is urea Urea derived from breakdown of amino acids Nitrogenous Wastes TOXIC! + 1. Dietary amino acids → NH2 removed → NH2 + H → NH3 500 ml of urine removes only 1 gram of nitrogen as ammonia 2. Ammonia can be converted to urea Requires energy 50 ml of urine removes 1 gram of nitrogen as urea 3. Ammonia can be converted to uric acid Requires lots of energy 10 ml of urine removes 1 gram of nitrogen as uric acid Urinary System Organs Kidneys Major excretory organs Urinary bladder Temporary storage reservoir for urine Ureters Transport urine from the kidneys to the bladder Urethra Transports urine out of the body Hepatic veins (cut) Esophagus (cut) Inferior vena cava Renal artery Adrenal gland Renal hilum Aorta Renal vein Kidney Iliac crest Ureter Rectum (cut) Uterus (part of female reproductive Urinary system) bladder Urethra Figure 25.1 Kidney: Urinary System page 6 Anterior Inferior vena cava Peritoneal -

Renal Pelvis and Ureter Cases
RP/Ureter Case 1 SURGICAL PATHOLOGY REPORT Surgical Pathology Report October 20, 2007 Specimen: A. Left ureter biopsy B. Uterus and bladder C. Right ureter Final Diagnosis: A. Left ureter biopsy - invasive high grade urothelial carcinoma. B. Uterus and bladder (radical cystohysterectomy) - invasive high grade urothelial carcinoma involving the left ureter. Neoplasm penetrates into but not through muscularis propria of the ureter. Extensive urothelial carcinoma in situ involving the bladder. No involvement of the urethra. Staging AJCC pathologic stage: pT2; pNX; pMX; No involvement of soft tissue margins; invasive carcinoma is present at the transected left ureteral margin. Cystic atrophy of the endometrium. Cervix, right fallopian tube and right ovary with no significant diagnostic abnormality. C. Right ureter - chronic ureteritis with reactive urothelial atypia; no dysplastic or neoplastic changes in sections examined. END RP/Ureter Case 1 1SEER MPH Rules Web Casts http://seer.cancer.gov/tools/mphrules/ RP/Ureter Case 2 SURGICAL PATHOLOGY REPORT Surgical Pathology Report September 10, 2007 Clinical History: Left renal pelvis mass, gross hematuria Specimen: Left kidney with ureter and bladder cuff Gross Description: The specimen is received in one formalin filled container labeled with the patient's name, sublabeled "left kidney with ureter and bladder cuff", and consists of a previously opened radical nephrectomy specimen which measures 13 x 8 x 8 cm. The adipose tissue is peeled away from the kidney. No adrenal grand is present. A ureter is present measuring 17 x 1 cm. The kidney measures 12 x 7 x 7 cm. Upon sectioning a fungating, friable gray-white mass lesion is located in the hilum measuring 6 x 6 x 5 cm. -

The Kidneys by Jennifer Kenny
The Kidneys By Jennifer Kenny 1 You have two kidneys that are very important to your body's functioning. They are purplish brown in color because of the rich supply of blood vessels. They are about the size of a grownup's fist, but they weigh less than a pound together. They are located above your waist with one on each side of the spine. The right kidney is slightly lower than the left kidney so the liver can fit. 2 At the top of each kidney are adrenal glands. They are not directly connected to the kidneys, but by secreting hormones, they do help control some of the work of the kidneys. 3 The kidneys themselves are protected by about an inch of fat. There would be serious consequences if the kidneys were injured. In fact, kidney punches are illegal in the boxing ring because of the risk. 4 The hilus is the inward curve of the kidneys. The ureter comes out from this spot. Nerves and blood vessels enter or pass through here, too. Blood is brought to the kidney by a renal artery. The blood is carried away by the renal vein. The renal capsule, a thin but tough membrane surrounds the rest of the kidney. 5 There are three layers to the kidney. The cortex is the outer layer and contains the kidney's filtering structures. The medulla is the middle layer. It drains the urine into tubes and empties into the renal pelvis. The renal pelvis is the inner layer that leads to the ureter. -

The Urinary System Consists of Kidneys, Ureters, Urinary Bladder
Anatomy Lecture Notes Chapter 23 the urinary system consists of kidneys, ureters, urinary bladder, and urethra the function of the kidneys is NOT "to make urine" the kidneys: 1) regulate water balance 2) regular ECF electrolyte levels (Na, K, Ca) 3) eliminate some metabolic wastes urine is a by-product of these functions A. kidneys 1. located against posterior abdominal wall (retroperitoneal) T11 or T12 to L3 right kidney lower than left kidney 2. surrounded by a. pararenal fat (posterior only) b. renal fascia c. adipose capsule - perirenal fat d. renal capsule - dense c.t. covering surface of kidney e. parietal peritoneum Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 3. layers a. cortex - contains renal corpuscles and extends inwards as renal columns b. medulla - consists of renal pyramids which consist mostly of collecting ducts papilla - apex of renal pyramid; where collecting ducts drain into calyx 4. cavities and associated structures a. renal sinus - space in medial part of kidney; contains renal pelvis b. renal pelvis - expanded superior part of ureter minor calyx collects urine from one renal papilla major calyx formed by junction of 2 or more minor calyces renal pelvis formed by junction of all major calyces Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 5. renal hilum - medial indentation; where ureter leaves kidney 6. blood flow through the kidney - renal fraction = 20% of cardiac output aorta renal artery segmental arteries lobar arteries interlobar arteries arcuate arteries cortical radiate (interlobular) arteries afferent arterioles glomerular capillaries (glomerulus) efferent arteriole peritubular capillaries and vasa recta cortical radiate (interlobular) veins arcuate veins interlobar veins renal vein inferior vena cava Strong/Fall 2008 Anatomy Lecture Notes Chapter 23 7. -

Renal Pelvis Dilation
Renal Pelvis Dilation Important information for patients Fetal Medicine Unit If you have any questions or concerns, please contact the Fetal Medicine Unit on 01270 273775 (Monday to Friday, 9.00am - 5.00pm). This leaflet is available in audio, Braille, large print and other languages. To request a copy, please telephone 01270 273775. Revised and reprinted July 2021 Review July 2024 Ref: WC/MS/0340721 www.mchft.nhs.uk We care because you matter Your baby has been found to have more fluid in its kidneys than What does this mean for my pregnancy? normal. This leaflet will explain what this means for your baby. First of Due to renal pelvis dilation: all, it is important for you to understand how kidneys work. • Your baby will not have to be born early. How does the renal system work? The kidneys work to filter out water and waste products from the body • There is no increased rate of miscarriage or preterm delivery. and dispose of it as urine. This urine makes up the amniotic fluid that surrounds and protects baby, whilst baby is in the womb. • Your baby’s growth will not be affected. The outer part of the kidney (renal cortex) creates the urine, whilst What will happen once my baby is born? the inner part (renal pelvis) collects it and drains it into the ureter. Your baby will be examined by a Paediatrician who will arrange any Urine flows from the renal pelvis down the tube called the ureter into follow-up that is needed. the urinary bladder. The urine is stored in the bladder and then passes through the urethra. -
Signaling During Kidney Development
Cells 2015, 4, 112-132; doi:10.3390/cells4020112 OPEN ACCESS cells ISSN 2073-4409 www.mdpi.com/journal/cells Review Signaling during Kidney Development Mirja Krause 1, Aleksandra Rak-Raszewska 1, Ilkka Pietilä 1, Susan E. Quaggin 2 and Seppo Vainio 1,* 1 Faculty of Biochemistry and Molecular Medicine, Biocenter Oulu, Oulu University, 90014 Oulu, Finland; E-Mails: [email protected] (M.K.); [email protected] (A.R.R.); [email protected] (I.P.) 2 Northwestern University, Feinberg School of Medicine, Chicago, IL 60611, USA; E-Mail: [email protected] * Author to whom correspondence should be addressed; E-Mail: [email protected]; Tel.: +358-407-470939. Academic Editor: Christoph Englert Received: 28 February 2015 / Accepted: 30 March 2015 / Published: 10 April 2015 Abstract: The kidney plays an essential role during excretion of metabolic waste products, maintenance of key homeostasis components such as ion concentrations and hormone levels. It influences the blood pressure, composition and volume. The kidney tubule system is composed of two distinct cell populations: the nephrons forming the filtering units and the collecting duct system derived from the ureteric bud. Nephrons are composed of glomeruli that filter the blood to the Bowman’s capsule and tubular structures that reabsorb and concentrate primary urine. The collecting duct is a Wolffian duct-derived epithelial tube that concentrates and collects urine and transfers it via the renal pelvis into the bladder. The mammalian kidney function depends on the coordinated development of specific cell types within a precise architectural framework. Due to the availability of modern analysis techniques, the kidney has become a model organ defining the paradigm to study organogenesis. -
TUMOURS of RENAL PELVIS by I
Postgrad Med J: first published as 10.1136/pgmj.28.319.275 on 1 May 1952. Downloaded from 275 TUMOURS OF RENAL PELVIS By I. H. GRIFFITHS, F.R.C.S. From the Urological Department, Middlesex Hospital At the Annual Meeting of the British Association of Urological Surgeons in June 195I a survey was made of 2314 renal and ureteric tumours collected from 67 Centres in the British Isles (Riches, Griffiths and Thackray (I95I)). In this series 315 (12.5 per cent.) were tumours of the renal pelvis, an incidence of about i in I200 of malignant tumours admitted to General Hospitals. This long series of an interesting, though com- paratively rare, condition presented an opportunity to study the clinical and pathological behaviour by copyright. and to determine what factors influence the prog- nosis. Many of the conclusions of this series serve only to confirm those of J. B. Macalpine .0 (I947) to whom credit is given for much valuable and original work on this subject. j- Aetiology Like most other tumours of the urinary tract, very little is known of the aetiology. A most http://pmj.bmj.com/ interesting fact arising from the collective report Il was that no cases of bilateral papillary tumours of the pelvis were recorded. This does suggest *14 that the noxious agent responsible for tumour production is not excreted in the urine. In the case of papillary tumours of the pelvis it is un- common to find any local condition which may be presumed to be a cause. The urine is usually found on September 24, 2021 by guest. -

The Urinary System: Part A
10/20/2014 PowerPoint® Lecture Slides Kidney Functions prepared by Barbara Heard, Atlantic Cape Community • Regulating total water volume and total College solute concentration in water • Regulating ECF ion concentrations C H A P T E R 25 • Ensuring long-term acid-base balance • Removal of metabolic wastes, toxins, drugs The Urinary System: Part A © Annie Leibovitz/Contact Press Images © 2013 Pearson Education, Inc. © 2013 Pearson Education, Inc. Kidney Functions Urinary System Organs • Endocrine functions • Kidneys - major excretory organs – Renin - regulation of blood pressure • Ureters - transport urine from kidneys to – Erythropoietin - regulation of RBC urinary bladder production • Urinary bladder - temporary storage • Activation of vitamin D reservoir for urine • Gluconeogenesis during prolonged fasting • Urethra transports urine out of body © 2013 Pearson Education, Inc. © 2013 Pearson Education, Inc. Figure 25.1 The urinary system. Figure 25.2b Position of the kidneys against the posterior body wall. Hepatic veins (cut) Esophagus (cut) Inferior vena cava Renal artery Adrenal gland Renal hilum Aorta Renal vein Kidney Iliac crest Ureter Rectum (cut) Uterus (part of female reproductive system) 12th rib Urinary bladder Urethra © 2013 Pearson Education, Inc. © 2013 Pearson Education, Inc. 1 10/20/2014 Internal Anatomy Homeostatic Imbalance • Renal cortex • Pyelitis – Granular-appearing superficial region – Infection of renal pelvis and calyces • Renal medulla • Pyelonephritis – Composed of cone-shaped medullary (renal) – Infection/inflammation of entire kidney pyramids • Normally - successfully treated with – Pyramids separated by renal columns antibiotics • Inward extensions of cortical tissue © 2013 Pearson Education, Inc. © 2013 Pearson Education, Inc. Figure 25.2a Position of the kidneys against the posterior body wall. Figure 25.3 Internal anatomy of the kidney.