Urinary System
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

The Anatomy of the Rectum and Anal Canal
BASIC SCIENCE identify the rectosigmoid junction with confidence at operation. The anatomy of the rectum The rectosigmoid junction usually lies approximately 6 cm below the level of the sacral promontory. Approached from the distal and anal canal end, however, as when performing a rigid or flexible sigmoid- oscopy, the rectosigmoid junction is seen to be 14e18 cm from Vishy Mahadevan the anal verge, and 18 cm is usually taken as the measurement for audit purposes. The rectum in the adult measures 10e14 cm in length. Abstract Diseases of the rectum and anal canal, both benign and malignant, Relationship of the peritoneum to the rectum account for a very large part of colorectal surgical practice in the UK. Unlike the transverse colon and sigmoid colon, the rectum lacks This article emphasizes the surgically-relevant aspects of the anatomy a mesentery (Figure 1). The posterior aspect of the rectum is thus of the rectum and anal canal. entirely free of a peritoneal covering. In this respect the rectum resembles the ascending and descending segments of the colon, Keywords Anal cushions; inferior hypogastric plexus; internal and and all of these segments may be therefore be spoken of as external anal sphincters; lymphatic drainage of rectum and anal canal; retroperitoneal. The precise relationship of the peritoneum to the mesorectum; perineum; rectal blood supply rectum is as follows: the upper third of the rectum is covered by peritoneum on its anterior and lateral surfaces; the middle third of the rectum is covered by peritoneum only on its anterior 1 The rectum is the direct continuation of the sigmoid colon and surface while the lower third of the rectum is below the level of commences in front of the body of the third sacral vertebra. -

Te2, Part Iii
TERMINOLOGIA EMBRYOLOGICA Second Edition International Embryological Terminology FIPAT The Federative International Programme for Anatomical Terminology A programme of the International Federation of Associations of Anatomists (IFAA) TE2, PART III Contents Caput V: Organogenesis Chapter 5: Organogenesis (continued) Systema respiratorium Respiratory system Systema urinarium Urinary system Systemata genitalia Genital systems Coeloma Coelom Glandulae endocrinae Endocrine glands Systema cardiovasculare Cardiovascular system Systema lymphoideum Lymphoid system Bibliographic Reference Citation: FIPAT. Terminologia Embryologica. 2nd ed. FIPAT.library.dal.ca. Federative International Programme for Anatomical Terminology, February 2017 Published pending approval by the General Assembly at the next Congress of IFAA (2019) Creative Commons License: The publication of Terminologia Embryologica is under a Creative Commons Attribution-NoDerivatives 4.0 International (CC BY-ND 4.0) license The individual terms in this terminology are within the public domain. Statements about terms being part of this international standard terminology should use the above bibliographic reference to cite this terminology. The unaltered PDF files of this terminology may be freely copied and distributed by users. IFAA member societies are authorized to publish translations of this terminology. Authors of other works that might be considered derivative should write to the Chair of FIPAT for permission to publish a derivative work. Caput V: ORGANOGENESIS Chapter 5: ORGANOGENESIS -

Kidney, Renal Tubule – Dilation
Kidney, Renal Tubule – Dilation Figure Legend: Figure 1 Kidney, Renal tubule - Dilation in a male B6C3F1 mouse from a chronic study. Dilated tubules are noted as tracts running through the cortex and outer medulla. Figure 2 Kidney, Renal tubule - Dilation in a male F344/N rat from a chronic study. Tubule dilation is present throughout the outer stripe of the outer medulla, extending into the cortex. Figure 3 Kidney, Renal tubule - Dilation in a male B6C3F1 mouse from a chronic study. Slight tubule dilation is associated with degeneration and necrosis. Figure 4 Kidney, Renal tubule - Dilation in a male F344/N rat from a chronic study. Tubule dilation is associated with chronic progressive nephropathy. Comment: Renal tubule dilation may occur anywhere along the nephron or collecting duct system. It may occur in focal areas or as tracts running along the entire length of kidney sections (Figure 1). 1 Kidney, Renal Tubule – Dilation Renal tubule dilation may occur from xenobiotic administration, secondary mechanisms, or an unknown pathogenesis (see Kidney – Nephropathy, Obstructive (Figure 2). Dilation may result from direct toxic injury to the tubule epithelium interfering with absorption and secretion (Figure 3). It may also occur secondary to renal ischemia or from prolonged diuresis related to drug administration. Secondary mechanisms of tubule dilation may result from lower urinary tract obstruction, the deposition of tubule crystals, interstitial inflammation and/or fibrosis, and chronic progressive nephropathy (Figure 4). A few dilated tubules may be regarded as normal histologic variation. Recommendation: Renal tubule dilation should be diagnosed and given a severity grade. The location of tubule dilation should be included in the diagnosis as a site modifier. -

Respiratory System
Respiratory system Department of Histology and Embryology of Jilin university ----Jiang Wenhua 1. General description z the nose, the pharynx, the larynx, the trachea, bronchus, lung zFunction: inspiring oxygen, expiring carbon dioxide The lung synthesises many materials 2.Trachea and bronchi General structure mucosa submucosa adventitia The trachea is a thin-walled tube about 11centimeters long and 2 centimeters in diameter, with a somewhat flattened posterior shape. The wall of the trachea is composed of three layers: mucosa, submucosa, and adventitia 2.1 mucosa 2.1.1 pseudostratified ciliated columnar epithelium 2.1.1.1 ciliated columnar cells These cells are columnar in shape with a centrally –located oval –shaped nucleus, on the free surface of the cells are microvilli and cilia, which regularly sweep toward the pharynx to remove inspired dust particles 2.1.1.2 brush cells These cells are columnar in shape with a round or oval –shaped nucleus located in the basal portion. on the free surface the microvilli are arranged into the shape of a brush. These cells are considered to be a type of under-developed ciliated columnar cell Schematic drawing of the trachea mucosa Scanning electron micrographs of the surface of mucosa Schematic drawing of the trachea mucosa 2.1.1.3 goblet cells secrete mucus to lubricate and protect the epithelium Schematic drawing of the trachea mucosa 2.1.1.4 basal cells These cells are cone –shaped and situated in the deep layer of the epithelium. Their apices are not exposed to the lumen, and their nuclei are round in shape, such cells constitute a variety of undifferentiated cells 2.1.1.5 small granular cells These cells are a kind of endocrine cells . -

The Oesophagus Lined with Gastric Mucous Membrane by P
Thorax: first published as 10.1136/thx.8.2.87 on 1 June 1953. Downloaded from Thorax (1953), 8, 87. THE OESOPHAGUS LINED WITH GASTRIC MUCOUS MEMBRANE BY P. R. ALLISON AND A. S. JOHNSTONE Leeds (RECEIVED FOR PUBLICATION FEBRUARY 26, 1953) Peptic oesophagitis and peptic ulceration of the likely to find its way into the museum. The result squamous epithelium of the oesophagus are second- has been that pathologists have been describing ary to regurgitation of digestive juices, are most one thing and clinicians another, and they have commonly found in those patients where the com- had the same name. The clarification of this point petence ofthecardia has been lost through herniation has been so important, and the description of a of the stomach into the mediastinum, and have gastric ulcer in the oesophagus so confusing, that been aptly named by Barrett (1950) " reflux oeso- it would seem to be justifiable to refer to the latter phagitis." In the past there has been some dis- as Barrett's ulcer. The use of the eponym does not cussion about gastric heterotopia as a cause of imply agreement with Barrett's description of an peptic ulcer of the oesophagus, but this point was oesophagus lined with gastric mucous membrane as very largely settled when the term reflux oesophagitis " stomach." Such a usage merely replaces one was coined. It describes accurately in two words confusion by another. All would agree that the the pathology and aetiology of a condition which muscular tube extending from the pharynx down- is a common cause of digestive disorder. -

Endocrine Block اللهم ال سهل اال ما جعلته سهل و أنت جتعل احلزن اذا شئت سهل
OSPE ENDOCRINE BLOCK اللهم ﻻ سهل اﻻ ما جعلته سهل و أنت جتعل احلزن اذا شئت سهل Important Points 1. Don’t forget to mention right and left. 2. Read the questions carefully. 3. Make sure your write the FULL name of the structures with the correct spelling. Example: IVC ✕ Inferior Vena Cava ✓ Aorta ✕ Abdominal aorta ✓ 4. There is NO guarantee whether or not the exam will go out of this file. ممكن يأشرون على أجزاء مو معلمه فراح نحط بيانات إضافية حاولوا تمرون عليها كلها Good luck! Pituitary gland Identify: 1. Anterior and posterior clinoidal process of sella turcica. 2. Hypophyseal fossa (sella turcica) Theory • The pituitary gland is located in middle cranial fossa and protected in sella turcica (hypophyseal fossa) of body of sphenoid. Relations Of Pituitary Gland hypothalamus Identify: 1. Mamillary body (posteriorly) 2. Optic chiasma (anteriorly) 3. Sphenoidal air sinuses (inferior) 4. Body of sphenoid 5. Pituitary gland Theory • If pituitary gland became enlarged (e.g adenoma) it will cause pressure on optic chiasma and lead to bilateral temporal eye field blindness (bilateral hemianopia) Relations Of Pituitary Gland Important! Identify: 1. Pituitary gland. 2. Diaphragma sellae (superior) 3. Sphenoidal air sinuses (inferior) 4. Cavernous sinuses (lateral) 5. Abducent nerve 6. Oculomotor nerve 7. Trochlear nerve 8. Ophthalmic nerve 9. Trigeminal (Maxillary) nerve Structures of lateral wall 10. Internal carotid artery Note: Ophthalmic and maxillary are both branches of the trigeminal nerve Divisions of Pituitary Gland Identify: 1. Anterior lobe (Adenohypophysis) 2. Optic chiasma 3. Infundibulum 4. Posterior lobe (Neurohypophysis) Theory Anterior Lobe Posterior Lobe • Adenohypophysis • Neurohypophysis • Secretes hormones • Stores hormones • Vascular connection to • Neural connection to hypothalamus by hypothalamus by Subdivisions hypophyseal portal hypothalamo-hypophyseal system (from superior tract from supraoptic and hypophyseal artery) paraventricular nuclei. -

Female Urethra
OBJECTIVES: • By the end of this lecture, student should understand the anatomical structure of urinary system. General Information Waste products of metabolism are toxic (CO2, ammonia, etc.) Removal from tissues by blood and lymph Removal from blood by Respiratory system And Urinary system Functions of the Urinary System Elimination of waste products Nitrogenous wastes Toxins Drugs Functions of the Urinary System Regulate homeostasis Water balance Acid-base balance in the blood Electrolytes Blood pressure Organs of the Urinary system Kidneys Ureters Urinary bladder Urethra Kidneys Primary organs of the urinary system Located between the 12th thoracic and 3rd lumbar vertebrae. Right is usually lower due to liver. Held in place by connective tissue [renal fascia] and surrounded by thick layer of adipose [perirenal fat] Each kidney is approx. 3 cm thick, 6 cm wide and 12 cm long Regions of the Kidney Renal cortex: outer region Renal medulla: pyramids and columns Renal pelvis: collecting system Kidneys protected by three connective tissue layers Renal fascia -Attaches to abdominal wall Renal capsule: -Surrounds each kidney -Fibrous sac -Protects from trauma and infection Adipose capsule -Fat cushioning kidney Nephrons Each kidney contains over a million nephrons [functional structure] • Blood enters the nephron from a network that begins with the renal artery. • This artery branches into smaller and smaller vessels and enters each nephron as an afferent arteriole. • The afferent arteriole ends in a specialized capillary called the Glomerulus. • Each kidney has a glomerulus contained in Bowman’s Capsule. • Any cells that are too large to pass into the nephron are returned to the venous blood supply via the efferent arteriole. -

Anatomical Study of the Coexistence of the Postaortic Left Brachiocephalic Vein with the Postaortic Left Renal Vein with a Review of the Literature
Okajimas Folia Anat.Coexistence Jpn., 91(3): of 73–81, postaortic November, veins 201473 Anatomical study of the coexistence of the postaortic left brachiocephalic vein with the postaortic left renal vein with a review of the literature By Akira IIMURA1, Takeshi OGUCHI1, Masato MATSUO1 Shogo HAYASHI2, Hiroshi MORIYAMA2 and Masahiro ITOH2 1Dental Anatomy Division, Department of Oral Science, Kanagawa Dental University, 82 Inaoka, Yokosuka, Kanagawa 238-8580, Japan 2Department of Anatomy, Tokyo Medical University, 6-1-1 Shinjuku-ku, Tokyo, 160, Japan –Received for Publication, December 11, 2014– Key Words: venous anomaly, postaortic vein, left brachiocephalic vein, left renal vein Summary: In a student course of gross anatomy dissection at Kanagawa Dental University in 2009, we found an extremely rare case of the coexistence of the postaortic left brachiocephalic vein with the postaortic left renal vein of a 73-year-old Japanese male cadaver. The left brachiocephalic vein passes behind the ascending aorta and connects with the right brachio- cephalic vein, and the left renal vein passes behind the abdominal aorta. These two anomalous cases mentioned above have been reported respectively. There have been few reports discussing coexistence of the postaortic left brachiocephalic vein with the postaortic left renal vein. We discuss the anatomical and embryological aspect of this anomaly with reference in the literature. Introduction phalic vein (PALBV) with the postaortic left renal vein (PALRV). These two anomalous cases mentioned above Normally, the left brachiocephalic vein passes in have been reported respectively. There have been few or front of the left common carotid artery and the brachio- no reports discussing coexistence of the PALBV with the cephalic artery and connects with the right brachioce- PALRV. -

Excretory Products and Their Elimination
290 BIOLOGY CHAPTER 19 EXCRETORY PRODUCTS AND THEIR ELIMINATION 19.1 Human Animals accumulate ammonia, urea, uric acid, carbon dioxide, water Excretory and ions like Na+, K+, Cl–, phosphate, sulphate, etc., either by metabolic System activities or by other means like excess ingestion. These substances have to be removed totally or partially. In this chapter, you will learn the 19.2 Urine Formation mechanisms of elimination of these substances with special emphasis on 19.3 Function of the common nitrogenous wastes. Ammonia, urea and uric acid are the major Tubules forms of nitrogenous wastes excreted by the animals. Ammonia is the most toxic form and requires large amount of water for its elimination, 19.4 Mechanism of whereas uric acid, being the least toxic, can be removed with a minimum Concentration of loss of water. the Filtrate The process of excreting ammonia is Ammonotelism. Many bony fishes, 19.5 Regulation of aquatic amphibians and aquatic insects are ammonotelic in nature. Kidney Function Ammonia, as it is readily soluble, is generally excreted by diffusion across 19.6 Micturition body surfaces or through gill surfaces (in fish) as ammonium ions. Kidneys do not play any significant role in its removal. Terrestrial adaptation 19.7 Role of other necessitated the production of lesser toxic nitrogenous wastes like urea Organs in and uric acid for conservation of water. Mammals, many terrestrial Excretion amphibians and marine fishes mainly excrete urea and are called ureotelic 19.8 Disorders of the animals. Ammonia produced by metabolism is converted into urea in the Excretory liver of these animals and released into the blood which is filtered and System excreted out by the kidneys. -
The Urinary Tract and How It Works
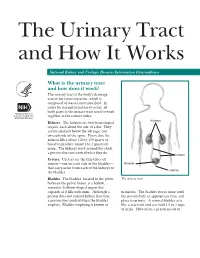
The Urinary Tract and How It Works National Kidney and Urologic Diseases Information Clearinghouse What is the urinary tract and how does it work? The urinary tract is the body’s drainage system for removing urine, which is composed of wastes and extra fluid. In order for normal urination to occur, all body parts in the urinary tract need to work together in the correct order. Kidneys Kidneys. The kidneys are two bean-shaped organs, each about the size of a fist. They are located just below the rib cage, one on each side of the spine. Every day, the kidneys filter about 120 to 150 quarts of blood to produce about 1 to 2 quarts of urine. The kidneys work around the clock; a person does not control what they do. Ureters Ureters. Ureters are the thin tubes of muscle—one on each side of the bladder— Bladder that carry urine from each of the kidneys to Urethra the bladder. Bladder. The bladder, located in the pelvis The urinary tract between the pelvic bones, is a hollow, muscular, balloon-shaped organ that expands as it fills with urine. Although a urination. The bladder stores urine until person does not control kidney function, the person finds an appropriate time and a person does control when the bladder place to urinate. A normal bladder acts empties. Bladder emptying is known as like a reservoir and can hold 1.5 to 2 cups of urine. How often a person needs to urinate depends on how quickly the kidneys Why is the urinary tract produce the urine that fills the bladder. -

Claudins in the Renal Collecting Duct
International Journal of Molecular Sciences Review Claudins in the Renal Collecting Duct Janna Leiz 1,2 and Kai M. Schmidt-Ott 1,2,3,* 1 Department of Nephrology and Intensive Care Medicine, Charité-Universitätsmedizin Berlin, 12203 Berlin, Germany; [email protected] 2 Molecular and Translational Kidney Research, Max-Delbrück-Center for Molecular Medicine in the Helmholtz Association (MDC), 13125 Berlin, Germany 3 Berlin Institute of Health (BIH), 10178 Berlin, Germany * Correspondence: [email protected]; Tel.: +49-(0)30-450614671 Received: 22 October 2019; Accepted: 20 December 2019; Published: 28 December 2019 Abstract: The renal collecting duct fine-tunes urinary composition, and thereby, coordinates key physiological processes, such as volume/blood pressure regulation, electrolyte-free water reabsorption, and acid-base homeostasis. The collecting duct epithelium is comprised of a tight epithelial barrier resulting in a strict separation of intraluminal urine and the interstitium. Tight junctions are key players in enforcing this barrier and in regulating paracellular transport of solutes across the epithelium. The features of tight junctions across different epithelia are strongly determined by their molecular composition. Claudins are particularly important structural components of tight junctions because they confer barrier and transport properties. In the collecting duct, a specific set of claudins (Cldn-3, Cldn-4, Cldn-7, Cldn-8) is expressed, and each of these claudins has been implicated in mediating aspects of the specific properties of its tight junction. The functional disruption of individual claudins or of the overall barrier function results in defects of blood pressure and water homeostasis. In this concise review, we provide an overview of the current knowledge on the role of the collecting duct epithelial barrier and of claudins in collecting duct function and pathophysiology. -

The Digestive System
69 chapter four THE DIGESTIVE SYSTEM THE DIGESTIVE SYSTEM The digestive system is structurally divided into two main parts: a long, winding tube that carries food through its length, and a series of supportive organs outside of the tube. The long tube is called the gastrointestinal (GI) tract. The GI tract extends from the mouth to the anus, and consists of the mouth, or oral cavity, the pharynx, the esophagus, the stomach, the small intestine, and the large intes- tine. It is here that the functions of mechanical digestion, chemical digestion, absorption of nutrients and water, and release of solid waste material take place. The supportive organs that lie outside the GI tract are known as accessory organs, and include the teeth, salivary glands, liver, gallbladder, and pancreas. Because most organs of the digestive system lie within body cavities, you will perform a dissection procedure that exposes the cavities before you begin identifying individual organs. You will also observe the cavities and their associated membranes before proceeding with your study of the digestive system. EXPOSING THE BODY CAVITIES should feel like the wall of a stretched balloon. With your skinned cat on its dorsal side, examine the cutting lines shown in Figure 4.1 and plan 2. Extend the cut laterally in both direc- out your dissection. Note that the numbers tions, roughly 4 inches, still working with indicate the sequence of the cutting procedure. your scissors. Cut in a curved pattern as Palpate the long, bony sternum and the softer, shown in Figure 4.1, which follows the cartilaginous xiphoid process to find the ventral contour of the diaphragm.