The Treatment of Acute Neerotizing Ulcerative Gingivitis Anne C
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent 19 11 Patent Number: 5,648,064 Gaffar Et Al
US005648064A United States Patent 19 11 Patent Number: 5,648,064 Gaffar et al. 45 Date of Patent: Jul. 15, 1997 (54) ORAL COMPOSITIONS HAVING 5,279,816 1/1994 Church et al. ............................ 424/53 ACCELERATED TOOTH WHTENING 5,302,374 4/1994 Wagner ..................................... 424/52 EFFECT 5,302,375 4/1994 Viscio ....................................... 424/53 5,356,554 10/1994 Delwel et al. ........................... 252/94 I76) Inventors: Abdul Gaffar, 89 Carter Rd., Princeton, 5,536,441 7/1996 Chapple et al. ................... 252A186.33 N.J. 08902; Sahar Fakhry-Smith. 7 FOREIGN PATENT DOCUMENTS Ryans Ct. Bordentown, N.J. 08505 0237111 9/1987 European Pat. Off. ......... C11D 3/39 (21) Appl. No.: 499,532 Primary Examiner-Shep K. Rose Attorney, Agent, or Firm-Paul Shapiro (22 Filed: Jul. 7, 1995 57 ABSTRACT (51] Int. Cl. .................. A61K 7/16; A61K7/20 52 U.S. Cl. ............................................... 424/53; 424/49 A two component whitening dentifrice composition is dis 58) Field of Search ................................... 424/53. 49-58 closed which comprises a first component containing a peroxygen compound such as hydrogen peroxide and a (56) References Cited second dentifrice component containing a manganese coor dination complex compound such as manganese gluconate, U.S. PATENT DOCUMENTS which activates the peroxygen compound and accelerates 4,728,455 3/1988 Rerek ........................................ 25299 the release of active oxygen for rapid whitening action, the 4,759,956 7/1988 Amer et al. ... 427/213 first and second components being maintained separate from 5,032,178 7/1991 Cornell ..................................... 106/35 the other until dispensed for application to teeth. 5, 194416 3/1993 Jureller et al. -

Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report Abstract Hereditary gingival fibromatosis (HGF) is a rare condition characterized by varying degrees of gingival hyperplasia. Gingival fibromatosis usually occurs as an isolated disorder or can be associated with a variety of other syndromes. A 33-year-old male patient who had a generalized severe gingival overgrowth covering two thirds of almost all maxillary and mandibular teeth is reported. A mucoperiosteal flap was performed using interdental and crevicular incisions to remove excess gingival tissues and an internal bevel incision to reflect flaps. The patient was treated 15 years ago in the same clinical facility using the same treatment strategy. There was no recurrence one year following the most recent surgery. Keywords: Gingival hyperplasia, hereditary gingival hyperplasia, HGF, hereditary disease, therapy, mucoperiostal flap Citation: S¸engün D, Hatipog˘lu H, Hatipog˘lu MG. Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report. J Contemp Dent Pract 2007 January;(8)1:090-096. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 8, No. 1, January 1, 2007 Introduction Hereditary gingival fibromatosis (HGF), also Ankara, Turkey with a complaint of recurrent known as elephantiasis gingiva, hereditary generalized gingival overgrowth. The patient gingival hyperplasia, idiopathic fibromatosis, had presented himself for examination at the and hypertrophied gingival, is a rare condition same clinic with the same complaint 15 years (1:750000)1 which can present as an isolated ago. At that time, he was treated with full-mouth disorder or more rarely as a syndrome periodontal surgery after the diagnosis of HGF component.2,3 This condition is characterized by had been made following clinical and histological a slow and progressive enlargement of both the examination (Figures 1 A-B). -
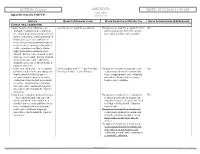
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Essential Dental (Pdf)
Dental Essential Plans 2 Plans1 for Individuals & Families with Optional Vision Benefits2 Table of Contents Optional Vision Benefits 5 Why Dental Essential? 2 Exclusions & Limitations 6 Dental Essential & Notice of Privacy Practices 10 Dental Essential Preferred 3 Wisconsin Outline of Coverage 14 Hearing Discounts 4 California Notices 18 Golden Rule Insurance Company is the underwriter of these plans. This product is administered by Dental Benefit Providers, Inc. Policy Forms GRI-DEN3-JR, -01 (AL), -02 (AZ), -03 (AR), -04 (CA), -05 (CO), -06 (CT), (DE), -08 (DC), -09 (FL), -10 (GA), -51 (HI), -12 (IL), -13 (IN), -14 (IA), -15 (KS), -16 (KY), -17 (LA), -19 (MD), -21 (MI), -22 (MN), -23 (MS), -24 (MO), -26 (NE), -28 (NH), -30 (NM), -32 (NC), -33 (ND), -35 (OK), -36 (OR), -37 (PA), -38 (RI), -39 (SC), -40 (SD), -41 (TN), -42 (TX), -43 (UT), -44 (VT), -45 (VA), -47 (WV), and -48 (WI); GRI-DEN3-JR-PB, -11 (ID), -34 (OH), -46 (WA); GRI-DEN3-JR-PBM, -11 (ID), -34 (OH), -46 (WA) 1 Essential Preferred is the only plan available in CO and MN. 2 The optional vision benefit is not available in MN, RI or WA. The ratio of incurred claims to earned premiums (loss-ratio) for total accident and health for Golden Rule Insurance Company in all states in 2019 was 62.4%. This is an outline only and is not intended to serve as a legal interpretation of benefits. Reasonable effort has been made to have this outline represent the intent of contract language. However, the contract language stands alone and the complete terms of the coverage will be determined by the policy. -

Hereditary Gingival Fibromatosis CASE REPORT
Richa et al.: Management of Hereditary Gingival Fibromatosis CASE REPORT Hereditary Gingival Fibromatosis and its management: A Rare Case of Homozygous Twins Richa1, Neeraj Kumar2, Krishan Gauba3, Debojyoti Chatterjee4 1-Tutor, Unit of Pedodontics and preventive dentistry, ESIC Dental College and Hospital, Rohini, Delhi. 2-Senior Resident, Unit of Pedodontics and preventive dentistry, Oral Health Sciences Centre, Post Correspondence to: Graduate Institute of Medical Education and Research , Chandigarh, India. 3-Professor and Head, Dr. Richa, Tutor, Unit of Pedodontics and Department of Oral Health Sciences Centre, Post Graduate Institute of Medical Education and preventive dentistry, ESIC Dental College and Research, Chandigarh, India. 4-Senior Resident, Department of Histopathology, Oral Health Sciences Hospital, Rohini, Delhi Centre, Post Graduate Institute of Medical Education and Research, Chandigarh, India. Contact Us: www.ijohmr.com ABSTRACT Hereditary gingival fibromatosis (HGF) is a rare condition which manifests itself by gingival overgrowth covering teeth to variable degree i.e. either isolated or as part of a syndrome. This paper presented two cases of generalized and severe HGF in siblings without any systemic illness. HGF was confirmed based on family history, clinical and histological examination. Management of both the cases was done conservatively. Quadrant wise gingivectomy using ledge and wedge method was adopted and followed for 12 months. The surgical procedure yielded functionally and esthetically satisfying results with no recurrence. KEYWORDS: Gingival enlargement, Hereditary, homozygous, Gingivectomy AA swollen gums. The patient gave a history of swelling of upper gums that started 2 years back which gradually aaaasasasss INTRODUCTION increased in size. The child’s mother denied prenatal Hereditary Gingival Enlargement, being a rare entity, is exposure to tobacco, alcohol, and drug. -

Gingivectomy Approaches: a Review
ISSN: 2469-5734 Peres et al. Int J Oral Dent Health 2019, 5:099 DOI: 10.23937/2469-5734/1510099 Volume 5 | Issue 3 International Journal of Open Access Oral and Dental Health REVIEW ARTICLE Gingivectomy Approaches: A Review Millena Mathias Peres1, Tais da Silva Lima¹, Idiberto José Zotarelli Filho1,2*, Igor Mariotto Beneti1,2, Marcelo Augusto Rudnik Gomes1,2 and Patrícia Garani Fernandes1,2 1University Center North Paulista (Unorp) Dental School, Brazil 2Department of Scientific Production, Post Graduate and Continuing Education (Unipos), Brazil Check for *Corresponding author: Prof. Idiberto José Zotarelli Filho, Department of Scientific Production, Post updates Graduate and Continuing Education (Unipos), Street Ipiranga, 3460, São José do Rio Preto SP, 15020-040, Brazil, Tel: +55-(17)-98166-6537 gingival tissue, and can be corrected with surgical tech- Abstract niques such as gingivectomy. Many patients seek dental offices for a beautiful, harmoni- ous smile to boost their self-esteem. At present, there is a Gingivectomy is a technique that is easy to carry great search for oral aesthetics, where the harmony of the out and is usually well accepted by patients, who, ac- smile is determined not only by the shape, position, and col- cording to the correct indications, can obtain satisfac- or of teeth but also by the gingival tissue. The present study aimed to establish the etiology and diagnosis of the gingi- tory results in dentogingival aesthetics and harmony val smile, with the alternative of correcting it with very safe [3]. surgical techniques such as gingivectomy. The procedure consists in the elimination of gingival deformities resulting The procedure consists in the removal of gingival de- in a better gingival contour. -

Surface Morphology Alterations in Bovine Dentin Exposed to Different Bleaching Agents
Braz J Oral Sci. Original Article January/March 2009 - Volume 8, Number 1 Surface morphology alterations in bovine dentin exposed to different bleaching agents Juliana Nascimento Santos1, Daniel Pinto de Oliveira1, Fábio Roberto Dametto1, Brenda Paula Figueiredo de Almeida Gomes2, Alexandre Augusto Zaia2, José Flávio Affonso de Almeida2, Caio Cezar Randi Ferraz2 1 DDS, MSc, PhD, Department of Restorative Dentistry and Endodontics, Faculdade de Odontologia de Piracicaba, Universidade Estadual de Campinas (Unicamp), Piracicaba (SP), Brazil 2 DDS, MSc, PhD, Professor, Department of Restorative Dentistry, Endodontics, Faculdade de Odontologia de Piracicaba, Unicamp, Piracicaba (SP), Brazil Abstract Aim: This study evaluated the morphological changes caused by internal bleaching agents on dentin surface. Methods: Twenty crowns of bovine incisors were cut into slabs that were randomly distributed in six experimental groups (n = 5), according to the bleaching agent used: G1 – sodium perborate + water, G2 – sodium perborate + 2% chlorhexidine gel, G3 – sodium perborate + 30% hydrogen peroxide, G4 – 30% hydrogen peroxide, G5 – 37% carbamide peroxide and G6 – gel base without carbamide. Two Control Groups were used: C1 with distilled water and C2 with 2% chlorhexidine gel. The specimens were immersed in the respective test bleaching agent and incubated at 37 °C for seven days. Following, they were prepared for scanning electron microscopy and five images from each tooth segment were recorded and analyzed for surface morphological alterations, by three previously calibrated examiners. Inter-examiner agreement was verified using the Kappa test. The rank averages obtained for the groups were subjected to Kruskal-Wallis analysis of variance at 5% significance level. Results: The analysis of the scores obtained indicated that all tested materials caused some morphological alteration on dentin, except for sodium perborate + water (G1) and Control Groups 1 and 2. -

Ammonium-Persulphate.Pdf
ADVANCE An Exclusive Chemical Range CHEMICAL SALES CORPORATION CHEMICAL SUPPLIES SIMPLIFIED ABOUT US ADVANCE CHEMICAL SALES CORPORATION Advance Chemical Sales Corporation is an industrial distributor of Fine & Speciality Chemicals. It boasts of its technology-driven innovative ways in suppling products to its customers. ADVANCE CHEMICAL SALES CORPORATION (ACSC) has been a trusted supplier of chemicals since 1968. We like to work alongside customers and solve their challenges with efficiency, progressive solutions and quality products. Whether the order is for chemical commodities or speciality chemicals, no matter if the volume is large or small, we can handle it. We are committed to bring the best quality products at competitive prices from reputed manufacturers to our customers. Our goal is to make sure that our customers find their needs of chemicals in one place. We work to develop the customers' trust An Exclusive Chemical Range EXEMPLAR DELHI is in Trade and Import of ACIDS, INORGANIC CHEMICALS, METAL ORGANIC COMPOUNDS, ORGANIC CHEMICALS & SOLVENTS. EXEMPLAR NOIDA produces chemicals like ACETATES, CHELATED EDTA, CITRATES, EDTA SALTS, GLUCONATES, HEDP SALTS, OXALATES, PHOSPHATES, TARTRATES, FINE & PERFORMANCE CHEMICALS INDUSTRIES SERVED AGRO CHEMICALS DAIRY PAINTS & INKS CERAMIC & GLASS DETERGENTS PESTICIDES CHEMICAL INDUSTRIES FOOD PROCESSING PHARMACEUTICALS CONSTRUCTION LUBRICANTS POULTRY FEED COSMETICS METAL TREATMENT WATER TREATMENT CHEMICAL SUPPLIES SIMPLIFIED ACETATES AGRO CHEMICALS Ammonium acetate Amino acid (Protein hydrolysate) Calcium acetate Boron-20 Potassium acetate Disodium octaborate tetrahydrate Sodium acetate 3 hyd. Fulvic acid Sodium acetate anhy. Potassium humate Sodium diacetate Potassium humate fulvate Zinc acetate 2 hy. Seaweed extract ACIDS ALKALIES Acetic acid glacial Alumina trihydrate Adipic acid Aluminium oxide (Calcined) Ascorbic acid Ammonia solution Benzoic acid Ammonium carbonate Boric acid Calcium carbonate Citric acid mono/ anhy. -

Entodinternational.Com ENTOD HOUSE, W-50(B), M.I.D.C, T.T.C
Since 1977... Ocular Care & Wellness Since 1977 OUR OPHTHALMIC • Over 40 Years of Pharmaceutical & Nutraceutical Expertise RANGE AT A GLANCE • International Formulation R&D Centres • Technology-Driven Ophthalmics • WHO GMP & US FDA Accredited Manufacturing • Global Exports CONTACT US Head Office: Entod Pharmaceuticals Ltd., OPHTHALMIC FORMULATIONS R & D OPHTHALMIC SPECIALTY EXCIPIENTS Ashirwad Building, S.V. Road, Opp. Badi Masjid, Bandra(W), Mumbai-400050, INDIA Email: [email protected] Additional Office: 15 Tottenham Lane, London N8 9DJ, UK. E-mail: [email protected] A Global Research-Based Speciality Website: ophthalmicsuk.com Formulation R&D: Pharmaceutical Enterprise Medisearch Laboratory entodinternational.com ENTOD HOUSE, W-50(B), M.I.D.C, T.T.C. Indl. Estate, Rabale, Thane-Belapur Road, Follow us on: Navi Mumbai-400701, INDIA Email: [email protected] @entodinternational @entodpharma Entod Pharmaceuticals Medisearch Laboratories Entod Research 2018073 Ltd. (India) (Bombay) Pvt. Ltd. (India) Cell Ltd. (UK) entodinternational.com entodinternational.com Complete Ophthalmic Finished Products Range PRESS-DT TABLET OMEFLOX-BM EYE DROPS EYETAMIN CAPSULES MYOPIA CONTROL Acetazolamide IP 250mg Ofloxacin IP 0.3% w/w Lycopene, Lutein Zeaxanthin, Betamethasone Sodium Phosphate 0.1% w/w Vitamins & Minerals MYATRO EYE DROPS ENDOR EYE DROPS FLUCOCID EYE DROPS Fluconazole USP 0.3% w/v Atropine Sulphate USP 0.01% w/v Dorzolamide HCl USP 2% w/v TOBRACID-F EYE DROPS I-DEW MEGA CAPSULES Stabilized Oxychloro Complex 0.005% w/v Benzalkonium Chloride Solution IP 0.0075%w/v NATACIN EYE DROPS Tobramycin Sulphate USP Omega 3 fatty acid (deodourised) eqv. To ENDOR PLUS EYE DROPS Natamycin USP 5.0%w/v equi. -

Literature Review
LITERATURE REVIEW PERIODONTAL ANATOMY The tissues which surround the teeth, and provide the support necessary for normal function form the periodontium (Greek peri- “around”; odont-, “tooth”). The periodontium is comprised of the gingiva, periodontal ligament, alveolar bone, and cementum. The gingiva is anatomically divided into the marginal (unattached), attached and interdental gingiva. The marginal gingiva forms the coronal border of the gingiva which surrounds the tooth, but is not adherent to it. The cemento-enamel junction (CEJ) is where the crown enamel and the root cementum meet. The Marginal gingiva in normal periodontal tissues extends approximately 2mm coronal tothe CEJ. Microscopically the gingiva is comprised of a central core of dense connective tissue and an outer surface of stratified squamous epithelium. The space between the marginal gingiva and the external tooth surface is termed the gingival sulcus. The normal depth of the gingival sulcus, and corresponding width of the marginal gingival, is variable. In general, sulcular depths less than 2mm to 3mm in humans and animals are considered normal1. Ranges from 0.0mm to 6.0mm 2 have been reported.. The depth of a sulcus histologically is not necessarily the same as the depth which could be measured with a periodontal probe. The probing depth of a clinically normal human or canine gingival sulcus is 2 to 3 mm2 1. Attached gingiva is bordered coronally by the apical extent of the unattached gingiva, which is, in turn, defined by the depth of the gingival sulcus. The apical extent of the attached 1 gingiva is the mucogingival junction on the facial aspect of the mandible and maxilla, and the lingual aspect of the mandibular attached gingiva. -

Food and Drugs
21 Part 170 to 199 Revised as of April 1, 2001 Food and Drugs Containing a codification of documents of general applicability and future effect As of April 1, 2001 With Ancillaries Published by Office of the Federal Register National Archives and Records Administration A Special Edition of the Federal Register VerDate 11<MAY>2000 11:38 Apr 16, 2001 Jkt 194064 PO 00000 Frm 00001 Fmt 8091 Sfmt 8091 Y:\SGML\194064F.XXX pfrm02 PsN: 194064F U.S. GOVERNMENT PRINTING OFFICE WASHINGTON : 2001 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: (202) 512-1800 Tax: (202) 512-2250 Mail Stop: SSOP, Washington, DC 20402–0001 VerDate 11<MAY>2000 11:38 Apr 16, 2001 Jkt 194064 PO 00000 Frm 00002 Fmt 8092 Sfmt 8092 Y:\SGML\194064F.XXX pfrm02 PsN: 194064F Table of Contents Page Explanation ................................................................................................ v Title 21: Chapter I—Food and Drug Administration, Department of Health and Human Services (Continued) ................................................. 3 Finding Aids: Material Approved for Incorporation by Reference ............................ 573 Table of CFR Titles and Chapters ....................................................... 587 Alphabetical List of Agencies Appearing in the CFR ......................... 605 Redesignation Table ............................................................................ 615 List of CFR Sections Affected ............................................................. 617 -

Scholars Journal of Medical Case Reports
DOI: 10.21276/sjmcr.2016.4.6.16 Scholars Journal of Medical Case Reports ISSN 2347-6559 (Online) Sch J Med Case Rep 2016; 4(6):416-419 ISSN 2347-9507 (Print) ©Scholars Academic and Scientific Publishers (SAS Publishers) (An International Publisher for Academic and Scientific Resources) Hereditary Gingival Fibromatosis: A Case Report with Review of Literature Jesudass Govada1, Sridhar Reddy Erugula2, Narendra Kumar Narahari3, Vijay Kumar R4,Rajajee KTSS5, Sudhir Kumar Vujhini6 1Associate Professor, Department of Pedodontics and Preventive Dentistry, Government Dental College and Hospital, RIMS, Kadapa, Andhra Pradesh, India 2Senior lecturer, Department of Oral Pathology, MNR Dental College and Hospital, Sangareddy, Telangana, India 3Assistant Professor, Department of Respiratory Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, India. 4Assistant Professor, Dept. of Dentistry, Govt. Dental College, Ananthapur,, Andhra Pradesh, India 5Reader, Dept of Pedodontics, Anil Neerukonda Institute of Dental Sciences, Visakhapatnam, Andhra Pradesh, India. 6Assistant Professor, Transfusion Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, India *Corresponding author Sudhir Kumar Vujhini Email: [email protected] Abstract: Gingival fibromatosis is characterized by localized or generalized fibrous enlargement of the gingivae, mainly around permanent teeth. Gingival fibromatosis affects only the masticatory mucosa and does not extend beyond the muco-gingival junction. This article describes an unusual case of hereditary gingival fibromatosis with delayed eruption of permanent teeth in an 11 year-old girl and her younger sibling. The patient presented with severely enlarged gingival tissues affecting both arches and multiple retained deciduous. Most of the permanent teeth were not erupted. She had no associated symptoms to suggest any syndrome but there was family history of similar disorder with father and paternal aunt.