Managing Discoloured Non-Vital Teeth: the Inside/Outside Bleaching Technique
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

United States Patent 19 11 Patent Number: 5,648,064 Gaffar Et Al
US005648064A United States Patent 19 11 Patent Number: 5,648,064 Gaffar et al. 45 Date of Patent: Jul. 15, 1997 (54) ORAL COMPOSITIONS HAVING 5,279,816 1/1994 Church et al. ............................ 424/53 ACCELERATED TOOTH WHTENING 5,302,374 4/1994 Wagner ..................................... 424/52 EFFECT 5,302,375 4/1994 Viscio ....................................... 424/53 5,356,554 10/1994 Delwel et al. ........................... 252/94 I76) Inventors: Abdul Gaffar, 89 Carter Rd., Princeton, 5,536,441 7/1996 Chapple et al. ................... 252A186.33 N.J. 08902; Sahar Fakhry-Smith. 7 FOREIGN PATENT DOCUMENTS Ryans Ct. Bordentown, N.J. 08505 0237111 9/1987 European Pat. Off. ......... C11D 3/39 (21) Appl. No.: 499,532 Primary Examiner-Shep K. Rose Attorney, Agent, or Firm-Paul Shapiro (22 Filed: Jul. 7, 1995 57 ABSTRACT (51] Int. Cl. .................. A61K 7/16; A61K7/20 52 U.S. Cl. ............................................... 424/53; 424/49 A two component whitening dentifrice composition is dis 58) Field of Search ................................... 424/53. 49-58 closed which comprises a first component containing a peroxygen compound such as hydrogen peroxide and a (56) References Cited second dentifrice component containing a manganese coor dination complex compound such as manganese gluconate, U.S. PATENT DOCUMENTS which activates the peroxygen compound and accelerates 4,728,455 3/1988 Rerek ........................................ 25299 the release of active oxygen for rapid whitening action, the 4,759,956 7/1988 Amer et al. ... 427/213 first and second components being maintained separate from 5,032,178 7/1991 Cornell ..................................... 106/35 the other until dispensed for application to teeth. 5, 194416 3/1993 Jureller et al. -

Surface Morphology Alterations in Bovine Dentin Exposed to Different Bleaching Agents
Braz J Oral Sci. Original Article January/March 2009 - Volume 8, Number 1 Surface morphology alterations in bovine dentin exposed to different bleaching agents Juliana Nascimento Santos1, Daniel Pinto de Oliveira1, Fábio Roberto Dametto1, Brenda Paula Figueiredo de Almeida Gomes2, Alexandre Augusto Zaia2, José Flávio Affonso de Almeida2, Caio Cezar Randi Ferraz2 1 DDS, MSc, PhD, Department of Restorative Dentistry and Endodontics, Faculdade de Odontologia de Piracicaba, Universidade Estadual de Campinas (Unicamp), Piracicaba (SP), Brazil 2 DDS, MSc, PhD, Professor, Department of Restorative Dentistry, Endodontics, Faculdade de Odontologia de Piracicaba, Unicamp, Piracicaba (SP), Brazil Abstract Aim: This study evaluated the morphological changes caused by internal bleaching agents on dentin surface. Methods: Twenty crowns of bovine incisors were cut into slabs that were randomly distributed in six experimental groups (n = 5), according to the bleaching agent used: G1 – sodium perborate + water, G2 – sodium perborate + 2% chlorhexidine gel, G3 – sodium perborate + 30% hydrogen peroxide, G4 – 30% hydrogen peroxide, G5 – 37% carbamide peroxide and G6 – gel base without carbamide. Two Control Groups were used: C1 with distilled water and C2 with 2% chlorhexidine gel. The specimens were immersed in the respective test bleaching agent and incubated at 37 °C for seven days. Following, they were prepared for scanning electron microscopy and five images from each tooth segment were recorded and analyzed for surface morphological alterations, by three previously calibrated examiners. Inter-examiner agreement was verified using the Kappa test. The rank averages obtained for the groups were subjected to Kruskal-Wallis analysis of variance at 5% significance level. Results: The analysis of the scores obtained indicated that all tested materials caused some morphological alteration on dentin, except for sodium perborate + water (G1) and Control Groups 1 and 2. -

Ammonium-Persulphate.Pdf
ADVANCE An Exclusive Chemical Range CHEMICAL SALES CORPORATION CHEMICAL SUPPLIES SIMPLIFIED ABOUT US ADVANCE CHEMICAL SALES CORPORATION Advance Chemical Sales Corporation is an industrial distributor of Fine & Speciality Chemicals. It boasts of its technology-driven innovative ways in suppling products to its customers. ADVANCE CHEMICAL SALES CORPORATION (ACSC) has been a trusted supplier of chemicals since 1968. We like to work alongside customers and solve their challenges with efficiency, progressive solutions and quality products. Whether the order is for chemical commodities or speciality chemicals, no matter if the volume is large or small, we can handle it. We are committed to bring the best quality products at competitive prices from reputed manufacturers to our customers. Our goal is to make sure that our customers find their needs of chemicals in one place. We work to develop the customers' trust An Exclusive Chemical Range EXEMPLAR DELHI is in Trade and Import of ACIDS, INORGANIC CHEMICALS, METAL ORGANIC COMPOUNDS, ORGANIC CHEMICALS & SOLVENTS. EXEMPLAR NOIDA produces chemicals like ACETATES, CHELATED EDTA, CITRATES, EDTA SALTS, GLUCONATES, HEDP SALTS, OXALATES, PHOSPHATES, TARTRATES, FINE & PERFORMANCE CHEMICALS INDUSTRIES SERVED AGRO CHEMICALS DAIRY PAINTS & INKS CERAMIC & GLASS DETERGENTS PESTICIDES CHEMICAL INDUSTRIES FOOD PROCESSING PHARMACEUTICALS CONSTRUCTION LUBRICANTS POULTRY FEED COSMETICS METAL TREATMENT WATER TREATMENT CHEMICAL SUPPLIES SIMPLIFIED ACETATES AGRO CHEMICALS Ammonium acetate Amino acid (Protein hydrolysate) Calcium acetate Boron-20 Potassium acetate Disodium octaborate tetrahydrate Sodium acetate 3 hyd. Fulvic acid Sodium acetate anhy. Potassium humate Sodium diacetate Potassium humate fulvate Zinc acetate 2 hy. Seaweed extract ACIDS ALKALIES Acetic acid glacial Alumina trihydrate Adipic acid Aluminium oxide (Calcined) Ascorbic acid Ammonia solution Benzoic acid Ammonium carbonate Boric acid Calcium carbonate Citric acid mono/ anhy. -

The Treatment of Acute Neerotizing Ulcerative Gingivitis Anne C
Penodontics The treatment of acute neerotizing ulcerative gingivitis Anne C. Hartnett* / Jacob Shiloah** The destruction of tbe interdental papillae and formation of permanent gingiva! craierx are common sequelae of acute neerotizing uleerative gingivitis. These craters ean be disfiguring, especially in the anterior gingiva, and ean act as a nidus for recurrent epi- sodes. Traditional therapy has emphasized a stirgieal approach for elimination of Ihese defects, often increasing the esthelie problems. The pwpose of this paper is to review the treatment modalities of acitte neerotizing itlcerative gingivitis and ¡Ilústrate an al- ternative treatment approach of periodic sealing, root planing, and antimicrohiai rinses with 0.12% chlorhexidine. With this therapeutic regimen, the disease proeess ean be reversed and damaged papillae may regenérale. (Quintessence Int 1991:22:95-100.) Introduction chetes, fusifonn bacteria, and species of Bacteroides are the organisms most frequently cultivated from Acute neerotizing ulcerative gingivitis (ANUG) is a these lesions,' a definitive periodontal pathogen has rapidly destructive, noncommunicable, gingival infec- yet to be tmplicated in the onset or progression of tion of complex etiology. It is characterized by necrosis ANUG. A susceptible animal model in which to study of the crest of the gingival papillae, spontaneous ANUG has not been found. bleeding, pain, and halitosis. If left untreated, it may Previous studies have speculated on the importance spread laterally and apically to involve the entire -

Entodinternational.Com ENTOD HOUSE, W-50(B), M.I.D.C, T.T.C
Since 1977... Ocular Care & Wellness Since 1977 OUR OPHTHALMIC • Over 40 Years of Pharmaceutical & Nutraceutical Expertise RANGE AT A GLANCE • International Formulation R&D Centres • Technology-Driven Ophthalmics • WHO GMP & US FDA Accredited Manufacturing • Global Exports CONTACT US Head Office: Entod Pharmaceuticals Ltd., OPHTHALMIC FORMULATIONS R & D OPHTHALMIC SPECIALTY EXCIPIENTS Ashirwad Building, S.V. Road, Opp. Badi Masjid, Bandra(W), Mumbai-400050, INDIA Email: [email protected] Additional Office: 15 Tottenham Lane, London N8 9DJ, UK. E-mail: [email protected] A Global Research-Based Speciality Website: ophthalmicsuk.com Formulation R&D: Pharmaceutical Enterprise Medisearch Laboratory entodinternational.com ENTOD HOUSE, W-50(B), M.I.D.C, T.T.C. Indl. Estate, Rabale, Thane-Belapur Road, Follow us on: Navi Mumbai-400701, INDIA Email: [email protected] @entodinternational @entodpharma Entod Pharmaceuticals Medisearch Laboratories Entod Research 2018073 Ltd. (India) (Bombay) Pvt. Ltd. (India) Cell Ltd. (UK) entodinternational.com entodinternational.com Complete Ophthalmic Finished Products Range PRESS-DT TABLET OMEFLOX-BM EYE DROPS EYETAMIN CAPSULES MYOPIA CONTROL Acetazolamide IP 250mg Ofloxacin IP 0.3% w/w Lycopene, Lutein Zeaxanthin, Betamethasone Sodium Phosphate 0.1% w/w Vitamins & Minerals MYATRO EYE DROPS ENDOR EYE DROPS FLUCOCID EYE DROPS Fluconazole USP 0.3% w/v Atropine Sulphate USP 0.01% w/v Dorzolamide HCl USP 2% w/v TOBRACID-F EYE DROPS I-DEW MEGA CAPSULES Stabilized Oxychloro Complex 0.005% w/v Benzalkonium Chloride Solution IP 0.0075%w/v NATACIN EYE DROPS Tobramycin Sulphate USP Omega 3 fatty acid (deodourised) eqv. To ENDOR PLUS EYE DROPS Natamycin USP 5.0%w/v equi. -

Food and Drugs
21 Part 170 to 199 Revised as of April 1, 2001 Food and Drugs Containing a codification of documents of general applicability and future effect As of April 1, 2001 With Ancillaries Published by Office of the Federal Register National Archives and Records Administration A Special Edition of the Federal Register VerDate 11<MAY>2000 11:38 Apr 16, 2001 Jkt 194064 PO 00000 Frm 00001 Fmt 8091 Sfmt 8091 Y:\SGML\194064F.XXX pfrm02 PsN: 194064F U.S. GOVERNMENT PRINTING OFFICE WASHINGTON : 2001 For sale by the Superintendent of Documents, U.S. Government Printing Office Internet: bookstore.gpo.gov Phone: (202) 512-1800 Tax: (202) 512-2250 Mail Stop: SSOP, Washington, DC 20402–0001 VerDate 11<MAY>2000 11:38 Apr 16, 2001 Jkt 194064 PO 00000 Frm 00002 Fmt 8092 Sfmt 8092 Y:\SGML\194064F.XXX pfrm02 PsN: 194064F Table of Contents Page Explanation ................................................................................................ v Title 21: Chapter I—Food and Drug Administration, Department of Health and Human Services (Continued) ................................................. 3 Finding Aids: Material Approved for Incorporation by Reference ............................ 573 Table of CFR Titles and Chapters ....................................................... 587 Alphabetical List of Agencies Appearing in the CFR ......................... 605 Redesignation Table ............................................................................ 615 List of CFR Sections Affected ............................................................. 617 -

European Patent Office
Europäisches Patentamt *EP001047406B1* (19) European Patent Office Office européen des brevets (11) EP 1 047 406 B1 (12) EUROPEAN PATENT SPECIFICATION (45) Date of publication and mention (51) Int Cl.7: A61K 9/00, A61K 47/18 of the grant of the patent: 23.04.2003 Bulletin 2003/17 (86) International application number: PCT/EP99/00160 (21) Application number: 99906123.7 (87) International publication number: (22) Date of filing: 13.01.1999 WO 99/036055 (22.07.1999 Gazette 1999/29) (54) AUTOCLAVABLE PHARMACEUTICAL COMPOSITIONS CONTAINING A CHELATING AGENT AUTOKLAVIERBARE PHARMAZEUTISCHE ZUSAMMENSETZUNGEN MIT KOMPLEXBILDNER COMPOSITIONS PHARMACEUTIQUES AUTOCLAVABLES, CONTENANT UN CHELATEUR (84) Designated Contracting States: (72) Inventor: KIS, György, Lajos AT BE CH CY DE DK ES FI FR GB GR IE IT LI LU CH-8273 Triboltingen (CH) MC NL PT SE (74) Representative: Becker, Konrad et al (30) Priority: 15.01.1998 EP 98810016 Novartis AG Corporate Intellectual Property (43) Date of publication of application: Patent- und Markenabteilung 02.11.2000 Bulletin 2000/44 4002 Basel (CH) (60) Divisional application: (56) References cited: 01124282.3 / 1 172 098 EP-A- 0 258 865 EP-A- 0 719 545 WO-A-97/00669 GB-A- 1 399 834 (73) Proprietors: GB-A- 2 001 529 US-A- 5 165 918 • Novartis AG 4056 Basel (CH) Designated Contracting States: BE CH DE DK ES FI FR GB GR IE IT LU MC NL PT SE CY LI • Novartis Pharma GmbH 1230 Wien (AT) Designated Contracting States: AT Note: Within nine months from the publication of the mention of the grant of the European patent, any person may give notice to the European Patent Office of opposition to the European patent granted. -

Usage Ingredients Literature
Usage Brush at least 2 times a day for at least 2 minutes with Implaclean®. Suitable for adults and children 6 years and over. Ingredients The toothpaste for people with dental implants Glycerin, Aqua, Hydrated Silica, Silica, PEG-32, Aroma, Cocamidopropyl Betaine, Sodium Gluconate, Cellulose Gum, Sodium Citrate, Lactoferrin, Sodium Saccharin, Magnesium Sulfate, Sodium Methylparaben, Sodium Perborate, Citric Acid, Sodium Chloride, Sodium Fluoride (200 ppm F-), CI 42090. Patented formula. Developed and recommended by dental surgeons, implantologists, dentists and oral hygienists. Literature 1. Berendsen JLM, el Allati I, Sylva LH, Blijdorp PA, Van Damme PhA, Meijer GJ. Ardox- X® adjunctive topical active oxygen application in periodontitis and peri-implantitis – a non published pilot study 2. Boere G Academic Centre for Dentistry Amsterdam (ACTA), Department of Dental Materials Science, The Netherlands, Influence of fluoride on titanium in an acidic environment measured by polarization resistance technique. J Appl Biomater. 1995 Winter;6(4):283-8 3. Nakagawa M, Matsuya S, Shiraishi T, Ohta M., Department of Dental Materials Engineering, Faculty of Dentistry, Kyushu University, Fukuoka, Japan. Effect of fluo- ride concentration and pH on corrosion behavior of titanium for dental use. J Dent Res. 1999 Sep;78(9):1568-72 4. Toumelin-Chemla F, Rouelle F, Burdairon G, Laboratoire de Biomatériaux, Faculté de Chirurgie Dentaire, l’Université Paris V, France Corrosive properties of fluoride- containing odontologic gels against titanium. J Dent. 1996 Jan-Mar;24(1-2):109-15. 5. Ide K, Hattori M, Yoshinari M, Kawada E, Oda Y. , Department of Dental Materials Science, Tokyo Dental College, 1-2-2 Masago, Mihama-ku, Chiba, Japan 261-8502. -
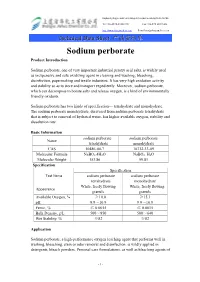
Sodium Perborate Product Introduction
Hangzhou Bay Shangyu economic and Technological Development Area,Zhejiang Province P.R.China Tel:+86-0575-81222198 Fax:+86-575 82211434 http://www.shangyuchem.com E-mail:[email protected] Technical Data Sheet 产品资料单 Sodium perborate Product Introduction Sodium perborate, one of very important industrial peroxy acid salts, is widely used as inexpensive and safe oxidizing agent in cleaning and washing, bleaching, disinfection, papermaking and textile industries. It has very high oxidation activity and stability so as to store and transport expediently. Moreover, sodium perborate, which can decompose to borate salts and release oxygen, is a kind of environmentally friendly oxidants. Sodium perborate has two kinds of specification--- tetrahydrate and monohydrate. The sodium perborate monohydrate, derivered from sodium perborate tetrahydrate that is subject to removal of hydrated water, has higher available oxygen, stability and dissolution rate. Basic Information sodium perborate sodium perborate Name tetrahydrate monohydrate CAS 10486-00-7 10332-33-09 Molecular Formula NaBO3.4H2O NaBO3. H2O Molecular Weight 153.86 99.81 Specification Specification Test Items sodium perborate sodium perborate tetrahydrate monohydrate White, freely flowing White, freely flowing Appearance granule granule Available Oxygen, % ≥10.0 ≥15.1 pH 9.9~10.9 9.9~10.9 Ferric, % ≤ 0.0015 ≤ 0.0015 Bulk Density, g/L 500~850 500~640 Wet Stability, % ≥82 ≥82 Application Sodium perborate, a high-performance oxygen leaching agent that performs well in washing, bleaching, stain or odor removal and disinfection, is wildly applied in detergents, bleach powders, Personal care formulations, as well as bleaching agents of - 1 - Hangzhou Bay Shangyu economic and Technological Development Area,Zhejiang Province P.R.China Tel:+86-0575-81222198 Fax:+86-575 82211434 http://www.shangyuchem.com E-mail:[email protected] Technical Data Sheet 产品资料单 Textile and paper pulp. -

Esthetic Dentistry
ESTHETIC DENTISTRY A modified inside/outside bleaching technique for nonvital discolored teeth: a case report François Reitzer*, DMD/Claire Ehlinger*, DMD/Maryline Minoux, DMD, PhD Over the past decades, the walking bleach technique using so- that the access cavity is left open. To overcome this disadvan- dium perborate was considered a safe and effective method to tage, the present authors propose to seal the bleaching agent bleach nonvital discolored teeth. However, sodium perbor ate in the access cavity instead of leaving the latter open. Through has been classified as carcinogenic, mutagenic, and toxic for a clinical case, this paper presents and discusses several aspects reproduction by European Union legislation. Its use is therefore of this protocol, including the clinical steps, the design of the prohibited since April 2015. The initially described inside/out- bleaching tray, and the treatment of potential recurrences. The side bleaching technique, combining internal and external ap- present authors believe that the protocol proposed in this arti- plication of 10% carbamide peroxide, is an alternative to the cle is easier to use for the patient. Moreover, it prevents the walking bleach technique using sodium perborate. While good accumulation of food debris in the access cavity and avoids the esthetic results and low risks of external cervical resorptions colonization of coronary dentin by bacteria. (Quintessence Int have been associated with this technique, its main drawback is 2019;50: 802–807; doi: 10.3290/j.qi.a43248) Key words: carbamide peroxide, case report, inside/outside bleaching technique, sodium perborate, walking bleach technique Discoloration of anterior teeth is an esthetic concern for many study on 95 teeth, good or acceptable results were observed in patients.1 On pulpless teeth, intrinsic dyschromia often results 89% of the cases. -

In Re Hydrogen Peroxide Antitrust Litigation
PRECEDENTIAL UNITED STATES COURT OF APPEALS FOR THE THIRD CIRCUIT No. 07-1689 IN RE: HYDROGEN PEROXIDE ANTITRUST LITIGATION Arkema Inc., Arkema France S.A., FMC Corp., Kemira Chemicals Canada, Inc., Kemira OYJ, Appellants On Appeal from the United States District Court for the Eastern District of Pennsylvania D.C. Civil Action No. 05-cv-0666 and MDL No. 1682 (Honorable Stewart Dalzell) Argued April 17, 2008 Before: SCIRICA, Chief Judge, AMBRO and FISHER, Circuit Judges. (Filed December 30, 2008) STEVEN E. BIZAR, ESQUIRE (ARGUED) LANDON Y. JONES III, ESQUIRE THOMAS P. MANNING, ESQUIRE HOWARD D. SCHER, ESQUIRE Buchanan Ingersoll & Rooney 1835 Market Street, 14th Floor Philadelphia, Pennsylvania 19103 Attorneys for Appellants, Arkema Inc. and Arkema France SA MICHAEL I. FRANKEL, ESQUIRE Dechert LLP Cira Centre, 18th Floor 2929 Arch Street Philadelphia, Pennsylvania 19104 Attorney for Appellant, FMC Corporation JEFFREY S. CASHDAN, ESQUIRE STEPHEN P. CUMMINGS, ESQUIRE CHRISTINE A. HOPKINSON, ESQUIRE CATHERINE M. O’NEIL, ESQUIRE King & Spalding 1180 Peachtree Street Atlanta, Georgia 30309 2 JOANNA J. CLINE, ESQUIRE BARBARA W. MATHER, ESQUIRE Pepper Hamilton 3000 Two Logan Square 18th & Arch Streets Philadelphia, Pennsylvania 19103 Attorneys for Appellants, Kemira OYJ and Kemira Chemicals Canada, Inc. GREGORY K. ARENSON, ESQUIRE (ARGUED) ROBERT N. KAPLAN, ESQUIRE Kaplan Fox & Kilsheimer 805 Third Avenue, 22nd Floor New York, New York 10022 ANTHONY J. BOLOGNESE, ESQUIRE Bolognese & Associates Suite 320, Two Penn Center Plaza 1500 John F. Kennedy Boulevard Philadelphia, Pennsylvania 19102 WILLIAM P. BUTTERFIELD, ESQUIRE Cohen Milstein Hausfeld & Toll West Tower, Suite 500 1100 New York Avenue, N.W. Washington, D.C. 20005 Attorneys for Appellees, Artco Chemical, Inc., Astro Chemicals, Inc., 3 Borden & Remington Corporation, Chem/Ser, Inc., EMCO Chemical Distributors, Inc., Finch Pruyn and Company, Inc., Interstate Chemical Company, Lensco Products, Inc., Lincoln Paper & Tissue, LLC, Ohio Chemical Services, Inc., James R. -

Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act
Updated June 07, 2021 Bulk Drug Substances Nominated for Use in Compounding Under Section 503B of the Federal Food, Drug, and Cosmetic Act Three categories of bulk drug substances: • Category 1: Bulk Drug Substances Under Evaluation • Category 2: Bulk Drug Substances that Raise Significant Safety Risks • Category 3: Bulk Drug Substances Nominated Without Adequate Support Updates to Categories of Substances Nominated for the 503B Bulk Drug Substances List1 • Add the following entry to category 2 due to serious safety concerns of mutagenicity, cytotoxicity, and possible carcinogenicity when quinacrine hydrochloride is used for intrauterine administration for non- surgical female sterilization: 2,3 o Quinacrine Hydrochloride for intrauterine administration • Revision to category 1 for clarity: o Modify the entry for “Quinacrine Hydrochloride” to “Quinacrine Hydrochloride (except for intrauterine administration).” • Revision to category 1 to correct a substance name error: o Correct the error in the substance name “DHEA (dehydroepiandosterone)” to “DHEA (dehydroepiandrosterone).” 1 For the purposes of the substance names in the categories, hydrated forms of the substance are included in the scope of the substance name. 2 Quinacrine HCl was previously reviewed in 2016 as part of FDA’s consideration of this bulk drug substance for inclusion on the 503A Bulks List. As part of this review, the Division of Bone, Reproductive and Urologic Products (DBRUP), now the Division of Urology, Obstetrics and Gynecology (DUOG), evaluated the nomination of quinacrine for intrauterine administration for non-surgical female sterilization and recommended that quinacrine should not be included on the 503A Bulks List for this use. This recommendation was based on the lack of information on efficacy comparable to other available methods of female sterilization and serious safety concerns of mutagenicity, cytotoxicity and possible carcinogenicity in use of quinacrine for this indication and route of administration.