Hereditary Gingival Fibromatosis CASE REPORT
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Chlorhexidine Soap Instructions
Pre-Operative Bathing Instructions Infection Prevention Because skin is not sterile, we need to be sure that your skin is as free of germs as possible before your admission. You can reduce the number of germs on your skin and decrease the risk of surgical site infection by preparing your skin with a special soap called chlorhexidine gluconate (CHG). The instructions for use are attached. What is CHG? CHG is a chemical antiseptic that is effective on both gram-positive and gram-negative bacteria. It is both bacteriocidal (kills) and bacteriostatic (stops reproductions) of any bacteria on the skin. CHG is in several products such as mouthwash, contact lens solution, wound wash, acne skin wash topical skin cleansers (chloraprep-what is used to clean your skin before an IV), thus we do not expect using this soap will cause skin irritation but please speak with your primary care physician to discuss any allergies. Studies show that repeated use of CHG soap enhances the ability of CHG to reduce bacterial counts on the skin; not only during the immediate period after the shower, but for a number of hours afterward. Studies suggest that patients may benefit from bathing or showering with CHG soap for at least 3 days before surgery in order to achieve the most benefit. It is unknown whether using CHG soap for less than or more than 3 days is beneficial. We recommend 3 days of treatment but understand this is not always possible and bathing the night before and the day of using CHG is acceptable. CHG soap can be purchased at any local pharmacy. -

Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report Abstract Hereditary gingival fibromatosis (HGF) is a rare condition characterized by varying degrees of gingival hyperplasia. Gingival fibromatosis usually occurs as an isolated disorder or can be associated with a variety of other syndromes. A 33-year-old male patient who had a generalized severe gingival overgrowth covering two thirds of almost all maxillary and mandibular teeth is reported. A mucoperiosteal flap was performed using interdental and crevicular incisions to remove excess gingival tissues and an internal bevel incision to reflect flaps. The patient was treated 15 years ago in the same clinical facility using the same treatment strategy. There was no recurrence one year following the most recent surgery. Keywords: Gingival hyperplasia, hereditary gingival hyperplasia, HGF, hereditary disease, therapy, mucoperiostal flap Citation: S¸engün D, Hatipog˘lu H, Hatipog˘lu MG. Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report. J Contemp Dent Pract 2007 January;(8)1:090-096. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 8, No. 1, January 1, 2007 Introduction Hereditary gingival fibromatosis (HGF), also Ankara, Turkey with a complaint of recurrent known as elephantiasis gingiva, hereditary generalized gingival overgrowth. The patient gingival hyperplasia, idiopathic fibromatosis, had presented himself for examination at the and hypertrophied gingival, is a rare condition same clinic with the same complaint 15 years (1:750000)1 which can present as an isolated ago. At that time, he was treated with full-mouth disorder or more rarely as a syndrome periodontal surgery after the diagnosis of HGF component.2,3 This condition is characterized by had been made following clinical and histological a slow and progressive enlargement of both the examination (Figures 1 A-B). -

Health Evidence Review Commission's Value-Based Benefits Subcommittee
Health Evidence Review Commission's Value-based Benefits Subcommittee September 28, 2017 8:00 AM - 1:00 PM Clackamas Community College Wilsonville Training Center, Room 111-112 29373 SW Town Center Loop E, Wilsonville, Oregon, 97070 Section 1.0 Call to Order AGENDA VALUE-BASED BENEFITS SUBCOMMITTEE September 28, 2017 8:00am - 1:00pm Wilsonville Training Center, Rooms 111-112 29353 SW Town Center Loop E Wilsonville, Oregon 97070 A working lunch will be served at approximately 12:00 PM All times are approximate I. Call to Order, Roll Call, Approval of Minutes – Kevin Olson 8:00 AM II. Staff report – Ariel Smits, Cat Livingston, Darren Coffman 8:05 AM A. Chronic Pain Task Force meeting report B. Errata C. Retreat III. Straightforward/Consent agenda – Ariel Smits 8:15 AM A. Consent table B. Straightforward Modifications to the Prioritized List Changes: Continuous Glucose Monitoring in Diabetes Mellitus C. Straightforward changes to the PPI guideline for Barrett’s esophagus with dysplasia D. Tobacco cessation guideline clarification IV. Advisory Panel reports 8:25 AM A. OHAP 1. 2018 CDT code placement recommendations V. Previous discussion items 8:30 AM A. Consideration for prioritization on lines 500/660, Services with Minimal or No Clinical Benefit and/or Low Cost-Effectiveness 1. New medications for the treatment of Duchenne muscular dystrophy i. deflazacort (Emflaza) ii. etepliren (Exondys 51) VI. New discussion items 9:30 AM A. Testicular prostheses B. Capsulorrhaphy for recurrent shoulder dislocation C. Transcutaneous neurostimulators D. Physical therapy for interstitial cystitis E. Acute peripheral nerve injuries F. SOI on role of Prioritized List in Coverage G. -
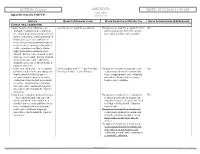
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Essential Dental (Pdf)
Dental Essential Plans 2 Plans1 for Individuals & Families with Optional Vision Benefits2 Table of Contents Optional Vision Benefits 5 Why Dental Essential? 2 Exclusions & Limitations 6 Dental Essential & Notice of Privacy Practices 10 Dental Essential Preferred 3 Wisconsin Outline of Coverage 14 Hearing Discounts 4 California Notices 18 Golden Rule Insurance Company is the underwriter of these plans. This product is administered by Dental Benefit Providers, Inc. Policy Forms GRI-DEN3-JR, -01 (AL), -02 (AZ), -03 (AR), -04 (CA), -05 (CO), -06 (CT), (DE), -08 (DC), -09 (FL), -10 (GA), -51 (HI), -12 (IL), -13 (IN), -14 (IA), -15 (KS), -16 (KY), -17 (LA), -19 (MD), -21 (MI), -22 (MN), -23 (MS), -24 (MO), -26 (NE), -28 (NH), -30 (NM), -32 (NC), -33 (ND), -35 (OK), -36 (OR), -37 (PA), -38 (RI), -39 (SC), -40 (SD), -41 (TN), -42 (TX), -43 (UT), -44 (VT), -45 (VA), -47 (WV), and -48 (WI); GRI-DEN3-JR-PB, -11 (ID), -34 (OH), -46 (WA); GRI-DEN3-JR-PBM, -11 (ID), -34 (OH), -46 (WA) 1 Essential Preferred is the only plan available in CO and MN. 2 The optional vision benefit is not available in MN, RI or WA. The ratio of incurred claims to earned premiums (loss-ratio) for total accident and health for Golden Rule Insurance Company in all states in 2019 was 62.4%. This is an outline only and is not intended to serve as a legal interpretation of benefits. Reasonable effort has been made to have this outline represent the intent of contract language. However, the contract language stands alone and the complete terms of the coverage will be determined by the policy. -

Sensitive Teeth.Qxp
Sensitive teeth may be a warning of more serious problems Do You Have Sensitive Teeth? If you have a common problem called “sensitive teeth,” a sip of iced tea or a cup of hot cocoa, the sudden intake of cold air or pressure from your toothbrush may be painful. Sensitive teeth can be experienced at any age as a momentary slight twinge to long-term severe discomfort. It is important to consult your dentist because sensitive teeth may be an early warning sign of more serious dental problems. Understanding Tooth Structure. What Causes Sensitive Teeth? To better understand how sensitivity There can be many causes for sensitive develops, we need to consider the teeth. Cavities, fractured teeth, worn tooth composition of tooth structure. The crown- enamel, cracked teeth, exposed tooth root, the part of the tooth that is most visible- gum recession or periodontal disease may has a tough, protective jacket of enamel, be causing the problem. which is an extremely strong substance. Below the gum line, a layer of cementum Periodontal disease is an infection of the protects the tooth root. Underneath the gums and bone that support the teeth. If left enamel and cementum is dentin. untreated, it can progress until bone and other supporting tissues are destroyed. This Dentin is a part of the tooth that contains can leave the root surfaces of teeth exposed tiny tubes. When dentin loses its and may lead to tooth sensitivity. protective covering and is exposed, these small tubes permit heat, cold, Brushing incorrectly or too aggressively may certain types of foods or pressure to injure your gums and can also cause tooth stimulate nerves and cells inside of roots to be exposed. -

Vhi Dental Rules - Terms and Conditions
Vhi Dental Rules - Terms and Conditions Date of Issue: 1st January 2021 Introduction to Your Policy The purpose of this Policy is to provide an Insured Person with Dental Services as described below. Only the stated Treatments are covered. Maximum benefit limits and any applicable waiting periods are listed in Your Table of Benefits. In order to qualify for cover under this Policy all Treatments must be undertaken by a Dentist or a Dental Hygienist in a dental surgery, be clinically necessary, in line with usual, reasonable and customary charges for the area where the Treatment was undertaken, and must be received by the Insured Person during their Period of Cover. Definitions We have defined below words or phrases used throughout this Policy. To avoid repeating these definitions please note that where these words or phrases appear they have the precise meaning described below unless otherwise stated. Where words or phrases are not listed within this section, they will take on their usual meaning within the English language. Accident An unforeseen injury caused by direct impact outside of oral cavity to an Insured Person’s teeth and gums (this includes damage to dentures whilst being worn). Cancer A malignant tumour, tissues or cells, characterised by the uncontrolled growth and spread of malignant cells and invasion of tissue. Child/Children Your children, step-child/children, legally adopted child/children or child/children where you are their legal guardian provided that the child/children is under age 18 on the date they are first included under this Policy. Claims Administrator Vhi Dental Claims Department, Intana, IDA Business Park, Athlumney, Navan, Co. -

Gingivectomy Approaches: a Review
ISSN: 2469-5734 Peres et al. Int J Oral Dent Health 2019, 5:099 DOI: 10.23937/2469-5734/1510099 Volume 5 | Issue 3 International Journal of Open Access Oral and Dental Health REVIEW ARTICLE Gingivectomy Approaches: A Review Millena Mathias Peres1, Tais da Silva Lima¹, Idiberto José Zotarelli Filho1,2*, Igor Mariotto Beneti1,2, Marcelo Augusto Rudnik Gomes1,2 and Patrícia Garani Fernandes1,2 1University Center North Paulista (Unorp) Dental School, Brazil 2Department of Scientific Production, Post Graduate and Continuing Education (Unipos), Brazil Check for *Corresponding author: Prof. Idiberto José Zotarelli Filho, Department of Scientific Production, Post updates Graduate and Continuing Education (Unipos), Street Ipiranga, 3460, São José do Rio Preto SP, 15020-040, Brazil, Tel: +55-(17)-98166-6537 gingival tissue, and can be corrected with surgical tech- Abstract niques such as gingivectomy. Many patients seek dental offices for a beautiful, harmoni- ous smile to boost their self-esteem. At present, there is a Gingivectomy is a technique that is easy to carry great search for oral aesthetics, where the harmony of the out and is usually well accepted by patients, who, ac- smile is determined not only by the shape, position, and col- cording to the correct indications, can obtain satisfac- or of teeth but also by the gingival tissue. The present study aimed to establish the etiology and diagnosis of the gingi- tory results in dentogingival aesthetics and harmony val smile, with the alternative of correcting it with very safe [3]. surgical techniques such as gingivectomy. The procedure consists in the elimination of gingival deformities resulting The procedure consists in the removal of gingival de- in a better gingival contour. -

Being Aware of Chlorhexidine Allergy
Being aware of chlorhexidine allergy If you have an immediate allergic reaction to chlorhexidine you may experience symptoms such as: x itching x skin rash (hives) x swelling x anaphylaxis. People who develop anaphylaxis to chlorhexidine may have experienced mild reactions, such as skin rash, to chlorhexidine before. Irritant contact dermatitis or allergic contact dermatitis Chlorhexidine can also cause irritant dermatitis. This is not a true allergic reaction. It is caused by chlorhexidine directly irritating skin and results in rough, dry and scaly Chlorhexidine is an antiseptic. Allergic reactions to skin, sometimes with weeping sores. chlorhexidine are rare but are becoming more common. Chlorhexidine is used in many products both in Chlorhexidine can also cause allergic contact hospitals and in the community. dermatitis. Symptoms look like irritant dermatitis, but the cause of the symptoms is delayed by 12-48 hours Why have I been given this factsheet? after contact with chlorhexidine. You have been given this brochure because you have had a reaction to a medication, a medical dressing Both irritant dermatitis and allergic contact dermatitis or antiseptic. This may or may not be caused by a caused by chlorhexidine are annoying but not chlorhexidine allergy. dangerous. It is important that you are aware of the possibility of an It is recommended that you avoid chlorhexidine if you allergy. experience these responses as some people have gone on to develop immediate allergic reaction to chlorhexidine. Allergic reactions to chlorhexidine Severe allergic reactions to chlorhexidine are rare, but How do I know which products contain they can be serious. Immediate allergic reactions can chlorhexidine? cause anaphlaxis (a very severe allergic reaction which can be life-threatening). -

3Rd Quarter 2001 Bulletin
In This Issue... Promoting Colorectal Cancer Screening Important Information and Documentaion on Promoting the Prevention of Colorectal Cancer ....................................................................................................... 9 Intestinal and Multi-Visceral Transplantation Coverage Guidelines and Requirements for Approval of Transplantation Facilities12 Expanded Coverage of Positron Emission Tomography Scans New HCPCS Codes and Coverage Guidelines Effective July 1, 2001 ..................... 14 Skilled Nursing Facility Consolidated Billing Clarification on HCPCS Coding Update and Part B Fee Schedule Services .......... 22 Final Medical Review Policies 29540, 33282, 67221, 70450, 76090, 76092, 82947, 86353, 93922, C1300, C1305, J0207, and J9293 ......................................................................................... 31 Outpatient Prospective Payment System Bulletin Devices Eligible for Transitional Pass-Through Payments, New Categories and Crosswalk C-codes to Be Used in Coding Devices Eligible for Transitional Pass-Through Payments ............................................................................................ 68 Features From the Medical Director 3 he Medicare A Bulletin Administrative 4 Tshould be shared with all General Information 5 health care practitioners and managerial members of the General Coverage 12 provider/supplier staff. Hospital Services 17 Publications issued after End Stage Renal Disease 19 October 1, 1997, are available at no-cost from our provider Skilled Nursing Facility -

Informed Consent for Gingivectomy
DR. J J FARGHER AND ASSOCIATES P ERIODONTICS AND DENT AL IMPLANTOLOGY Informed Consent for Gingivectomy Gingivectomy: A type of surgery used to remove excessive tissue or reduce pockets. It involves not only removal of the tissue, but scaling and root planning of the affected teeth. This procedure is performed with local anesthesia. All dental treatments have an associated risk. Periodontal surgery of any type may result in bleeding, swelling, bruising, pain, infection, sore jaws, recession, tooth sensitivity to hot and cold, caries exposure, etc. I understand that every person responds to treatment differently. Therefore, it is impossible for the doctor to predict how long the healing period may require or if time away from normal routines may be necessary. I understand that smoking and poor oral hygiene may significantly interfere with healing and cause disease reoccurrence. I understand if no treatment is rendered or if active treatment is interrupted or discontinued, my periodontal condition would likely continue and worsen. This may result in pain, swelling, bleeding, infection, recession, mobility, decay, staining, bone loss, and tooth loss. In the case of a gingivectomy, a second procedure may be required to ensure good symmetry and esthetics, depending on how the tissue heals. I have been advised of my alternatives to this treatment and understand what has been proposed thoroughly. I confirm with my signature that: My periodontist has discussed the above information with me. I have had the chance to ask questions. All of my questions have been answered to my satisfaction. I do hereby consent to the treatment described in this form. -
Don't We All Want Healthy Teeth and Gums? Yet Sometimes, Even with Brushing, Flossing, and Eating Healthy Foods — It Still Isn't Enough
Don't we all want healthy teeth and gums? Yet sometimes, even with brushing, flossing, and eating healthy foods — it still isn't enough. Or maybe you just want a whiter, brighter smile without the toxic ingredients in conventional products. It's herbs to the rescue! These 10 healing herbs prevent decay, and even restore. Add them to toothpaste, make them into tea, or make them into tinctures to combine into an herbal mouthwash. Herb #1 — Myrrh This is my go-to for teeth and gums. When toothache strikes, a little myrrh tincture placed on the tooth relieves pain in less than a minute. It also heals and tightens gums, cures bleeding gums, and fights bacteria that would otherwise cause gum disease and tooth decay. I use it daily as a preventative. Herb #2 — Neem Traditionally, sticks of neem were used as a natural toothbrush due to its strong antibacterial properties. Even today, it's regaining popularity. Modern research attests its ability to reduce plaque, prevent cavities and gum disease, and freshen breath. You can easily add powdered neem to your usual toothpaste. And remember, the bark is more potent than the leaf. Herb #3 — Echinacea. No, echinacea isn't just a cold-fighting herb! It also reduces inflamma- tion, boosts the immune system, and helps fight infection in the mouth. Herb #4 — Goldenseal. This herb is especially helpful for healing gums. It's antibiotic, anti- viral, and anti-inflammatory. Herb #5 — Oregon Grape Root. Antimicrobial and an astringent, Oregon grape root also soothes and tightens swollen gums. Herb #6 — Propolis.