Gingivectomy Approaches: a Review
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report Abstract Hereditary gingival fibromatosis (HGF) is a rare condition characterized by varying degrees of gingival hyperplasia. Gingival fibromatosis usually occurs as an isolated disorder or can be associated with a variety of other syndromes. A 33-year-old male patient who had a generalized severe gingival overgrowth covering two thirds of almost all maxillary and mandibular teeth is reported. A mucoperiosteal flap was performed using interdental and crevicular incisions to remove excess gingival tissues and an internal bevel incision to reflect flaps. The patient was treated 15 years ago in the same clinical facility using the same treatment strategy. There was no recurrence one year following the most recent surgery. Keywords: Gingival hyperplasia, hereditary gingival hyperplasia, HGF, hereditary disease, therapy, mucoperiostal flap Citation: S¸engün D, Hatipog˘lu H, Hatipog˘lu MG. Long-term Uncontrolled Hereditary Gingival Fibromatosis: A Case Report. J Contemp Dent Pract 2007 January;(8)1:090-096. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 8, No. 1, January 1, 2007 Introduction Hereditary gingival fibromatosis (HGF), also Ankara, Turkey with a complaint of recurrent known as elephantiasis gingiva, hereditary generalized gingival overgrowth. The patient gingival hyperplasia, idiopathic fibromatosis, had presented himself for examination at the and hypertrophied gingival, is a rare condition same clinic with the same complaint 15 years (1:750000)1 which can present as an isolated ago. At that time, he was treated with full-mouth disorder or more rarely as a syndrome periodontal surgery after the diagnosis of HGF component.2,3 This condition is characterized by had been made following clinical and histological a slow and progressive enlargement of both the examination (Figures 1 A-B). -
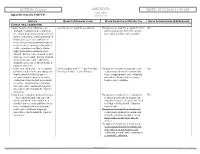
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Essential Dental (Pdf)
Dental Essential Plans 2 Plans1 for Individuals & Families with Optional Vision Benefits2 Table of Contents Optional Vision Benefits 5 Why Dental Essential? 2 Exclusions & Limitations 6 Dental Essential & Notice of Privacy Practices 10 Dental Essential Preferred 3 Wisconsin Outline of Coverage 14 Hearing Discounts 4 California Notices 18 Golden Rule Insurance Company is the underwriter of these plans. This product is administered by Dental Benefit Providers, Inc. Policy Forms GRI-DEN3-JR, -01 (AL), -02 (AZ), -03 (AR), -04 (CA), -05 (CO), -06 (CT), (DE), -08 (DC), -09 (FL), -10 (GA), -51 (HI), -12 (IL), -13 (IN), -14 (IA), -15 (KS), -16 (KY), -17 (LA), -19 (MD), -21 (MI), -22 (MN), -23 (MS), -24 (MO), -26 (NE), -28 (NH), -30 (NM), -32 (NC), -33 (ND), -35 (OK), -36 (OR), -37 (PA), -38 (RI), -39 (SC), -40 (SD), -41 (TN), -42 (TX), -43 (UT), -44 (VT), -45 (VA), -47 (WV), and -48 (WI); GRI-DEN3-JR-PB, -11 (ID), -34 (OH), -46 (WA); GRI-DEN3-JR-PBM, -11 (ID), -34 (OH), -46 (WA) 1 Essential Preferred is the only plan available in CO and MN. 2 The optional vision benefit is not available in MN, RI or WA. The ratio of incurred claims to earned premiums (loss-ratio) for total accident and health for Golden Rule Insurance Company in all states in 2019 was 62.4%. This is an outline only and is not intended to serve as a legal interpretation of benefits. Reasonable effort has been made to have this outline represent the intent of contract language. However, the contract language stands alone and the complete terms of the coverage will be determined by the policy. -

Hereditary Gingival Fibromatosis CASE REPORT
Richa et al.: Management of Hereditary Gingival Fibromatosis CASE REPORT Hereditary Gingival Fibromatosis and its management: A Rare Case of Homozygous Twins Richa1, Neeraj Kumar2, Krishan Gauba3, Debojyoti Chatterjee4 1-Tutor, Unit of Pedodontics and preventive dentistry, ESIC Dental College and Hospital, Rohini, Delhi. 2-Senior Resident, Unit of Pedodontics and preventive dentistry, Oral Health Sciences Centre, Post Correspondence to: Graduate Institute of Medical Education and Research , Chandigarh, India. 3-Professor and Head, Dr. Richa, Tutor, Unit of Pedodontics and Department of Oral Health Sciences Centre, Post Graduate Institute of Medical Education and preventive dentistry, ESIC Dental College and Research, Chandigarh, India. 4-Senior Resident, Department of Histopathology, Oral Health Sciences Hospital, Rohini, Delhi Centre, Post Graduate Institute of Medical Education and Research, Chandigarh, India. Contact Us: www.ijohmr.com ABSTRACT Hereditary gingival fibromatosis (HGF) is a rare condition which manifests itself by gingival overgrowth covering teeth to variable degree i.e. either isolated or as part of a syndrome. This paper presented two cases of generalized and severe HGF in siblings without any systemic illness. HGF was confirmed based on family history, clinical and histological examination. Management of both the cases was done conservatively. Quadrant wise gingivectomy using ledge and wedge method was adopted and followed for 12 months. The surgical procedure yielded functionally and esthetically satisfying results with no recurrence. KEYWORDS: Gingival enlargement, Hereditary, homozygous, Gingivectomy AA swollen gums. The patient gave a history of swelling of upper gums that started 2 years back which gradually aaaasasasss INTRODUCTION increased in size. The child’s mother denied prenatal Hereditary Gingival Enlargement, being a rare entity, is exposure to tobacco, alcohol, and drug. -

Vhi Dental Rules - Terms and Conditions
Vhi Dental Rules - Terms and Conditions Date of Issue: 1st January 2021 Introduction to Your Policy The purpose of this Policy is to provide an Insured Person with Dental Services as described below. Only the stated Treatments are covered. Maximum benefit limits and any applicable waiting periods are listed in Your Table of Benefits. In order to qualify for cover under this Policy all Treatments must be undertaken by a Dentist or a Dental Hygienist in a dental surgery, be clinically necessary, in line with usual, reasonable and customary charges for the area where the Treatment was undertaken, and must be received by the Insured Person during their Period of Cover. Definitions We have defined below words or phrases used throughout this Policy. To avoid repeating these definitions please note that where these words or phrases appear they have the precise meaning described below unless otherwise stated. Where words or phrases are not listed within this section, they will take on their usual meaning within the English language. Accident An unforeseen injury caused by direct impact outside of oral cavity to an Insured Person’s teeth and gums (this includes damage to dentures whilst being worn). Cancer A malignant tumour, tissues or cells, characterised by the uncontrolled growth and spread of malignant cells and invasion of tissue. Child/Children Your children, step-child/children, legally adopted child/children or child/children where you are their legal guardian provided that the child/children is under age 18 on the date they are first included under this Policy. Claims Administrator Vhi Dental Claims Department, Intana, IDA Business Park, Athlumney, Navan, Co. -

Informed Consent for Gingivectomy
DR. J J FARGHER AND ASSOCIATES P ERIODONTICS AND DENT AL IMPLANTOLOGY Informed Consent for Gingivectomy Gingivectomy: A type of surgery used to remove excessive tissue or reduce pockets. It involves not only removal of the tissue, but scaling and root planning of the affected teeth. This procedure is performed with local anesthesia. All dental treatments have an associated risk. Periodontal surgery of any type may result in bleeding, swelling, bruising, pain, infection, sore jaws, recession, tooth sensitivity to hot and cold, caries exposure, etc. I understand that every person responds to treatment differently. Therefore, it is impossible for the doctor to predict how long the healing period may require or if time away from normal routines may be necessary. I understand that smoking and poor oral hygiene may significantly interfere with healing and cause disease reoccurrence. I understand if no treatment is rendered or if active treatment is interrupted or discontinued, my periodontal condition would likely continue and worsen. This may result in pain, swelling, bleeding, infection, recession, mobility, decay, staining, bone loss, and tooth loss. In the case of a gingivectomy, a second procedure may be required to ensure good symmetry and esthetics, depending on how the tissue heals. I have been advised of my alternatives to this treatment and understand what has been proposed thoroughly. I confirm with my signature that: My periodontist has discussed the above information with me. I have had the chance to ask questions. All of my questions have been answered to my satisfaction. I do hereby consent to the treatment described in this form. -

The Treatment of Acute Neerotizing Ulcerative Gingivitis Anne C
Penodontics The treatment of acute neerotizing ulcerative gingivitis Anne C. Hartnett* / Jacob Shiloah** The destruction of tbe interdental papillae and formation of permanent gingiva! craierx are common sequelae of acute neerotizing uleerative gingivitis. These craters ean be disfiguring, especially in the anterior gingiva, and ean act as a nidus for recurrent epi- sodes. Traditional therapy has emphasized a stirgieal approach for elimination of Ihese defects, often increasing the esthelie problems. The pwpose of this paper is to review the treatment modalities of acitte neerotizing itlcerative gingivitis and ¡Ilústrate an al- ternative treatment approach of periodic sealing, root planing, and antimicrohiai rinses with 0.12% chlorhexidine. With this therapeutic regimen, the disease proeess ean be reversed and damaged papillae may regenérale. (Quintessence Int 1991:22:95-100.) Introduction chetes, fusifonn bacteria, and species of Bacteroides are the organisms most frequently cultivated from Acute neerotizing ulcerative gingivitis (ANUG) is a these lesions,' a definitive periodontal pathogen has rapidly destructive, noncommunicable, gingival infec- yet to be tmplicated in the onset or progression of tion of complex etiology. It is characterized by necrosis ANUG. A susceptible animal model in which to study of the crest of the gingival papillae, spontaneous ANUG has not been found. bleeding, pain, and halitosis. If left untreated, it may Previous studies have speculated on the importance spread laterally and apically to involve the entire -

Literature Review
LITERATURE REVIEW PERIODONTAL ANATOMY The tissues which surround the teeth, and provide the support necessary for normal function form the periodontium (Greek peri- “around”; odont-, “tooth”). The periodontium is comprised of the gingiva, periodontal ligament, alveolar bone, and cementum. The gingiva is anatomically divided into the marginal (unattached), attached and interdental gingiva. The marginal gingiva forms the coronal border of the gingiva which surrounds the tooth, but is not adherent to it. The cemento-enamel junction (CEJ) is where the crown enamel and the root cementum meet. The Marginal gingiva in normal periodontal tissues extends approximately 2mm coronal tothe CEJ. Microscopically the gingiva is comprised of a central core of dense connective tissue and an outer surface of stratified squamous epithelium. The space between the marginal gingiva and the external tooth surface is termed the gingival sulcus. The normal depth of the gingival sulcus, and corresponding width of the marginal gingival, is variable. In general, sulcular depths less than 2mm to 3mm in humans and animals are considered normal1. Ranges from 0.0mm to 6.0mm 2 have been reported.. The depth of a sulcus histologically is not necessarily the same as the depth which could be measured with a periodontal probe. The probing depth of a clinically normal human or canine gingival sulcus is 2 to 3 mm2 1. Attached gingiva is bordered coronally by the apical extent of the unattached gingiva, which is, in turn, defined by the depth of the gingival sulcus. The apical extent of the attached 1 gingiva is the mucogingival junction on the facial aspect of the mandible and maxilla, and the lingual aspect of the mandibular attached gingiva. -

Hereditary Gingival Fibromatosis, Inherited Disease, Gingivectomy
Clinical Practice 2014, 3(1): 7-10 DOI: 10.5923/j.cp.20140301.03 Hereditary Gingival Fibromatosis - A Case Report Anand Kishore1,*, Vivek Srivastava2, Ajeeta Meenawat2, Ambrish Kaushal3 1King George Medical College, Lucknow 2BBD College of dental sciences 3Chandra Dental College & Hospital Abstract Hereditary gingival fibromatosis is characterized by a slow benign enlargement of gingival tissue. It causes teeth being partially or totally covered by enlarged gingiva, causing esthetic and functional problems. It is usually transmitted both as autosomal dominant trait and autosomal recessive inheritance although sporadic cases are commonly reported. This paper reports three cases of gingival fibromatosis out of which one was in a 15 year old girl treated with convectional gingivectomy. Keywords Hereditary gingival fibromatosis, Inherited disease, Gingivectomy having the gingival enlargement before the patient’s birth 1. Introduction and she got operated in the village government hospital. No further relevant medical history was present. Hereditary gingival fibromatosis (HGF) or Idiopathic gingival fibromatosis is a rare, benign, asymptomatic, non-hemorrhagic and non-exudative proliferative fibrous lesion of gingival tissue occurring equally among men and women, in both arches with varying intensity in individuals within the same family [1]. It occurs as an autosomal dominant condition although recessive form also does occur. Consanguinity seems to increase the risk of autosomal dominant inheritance. It affects the marginal gingival, attached gingival and interdental papilla presenting as pink, non-hemorrhagic and have a firm, fibrotic consistency [2]. It also shows a generalized firm nodular enlargement with smooth to stippled surfaces and minimal tendency to bleed. Figure 1. Gingival enlargement However, in some cases the enlargement can be so firm and dense that it feels like bone on palpation [3]. -

POST-OPERATIVE INSTRUCTIONS Gingivectomy
POST-OPERATIVE INSTRUCTIONS Gingivectomy MEDICATIONS ☐ Take all prescribed medications as directed- Finish ALL antibiotics and anti-inflammatories. (Naproxen, Ibuprofen, Medrol Dose Pack). MEDICATIONS ☐ Take Naproxen Sodium 500mg (2X/day) with food, as needed for pain. ☐ One tablet of Extra Strength Tylenol every 6 hours is okay to take in between doses of Naproxen. FOR DISCOMFORT SWELLING ☐ Swelling is normal for up to 1-2 weeks post procedure, peaking at 2 to 4 days and especially in the early morning. ☐ First Two Days: Apply ice pack 20 minutes on/ 20 minutes off ☐ Third Day: Apply heat pack 20 minutes on/20 minutes off ☐ Sleep on 2 pillows to elevate head. BLEEDING ☐ Light bleeding (oozing) from the surgical area may occur for up to 48 hours post-surgery. ☐ Control by applying pressure with moist gauze or a wet tea bag for minimum of 30 minutes. DIET ☐ All soft foods for 7 days post-procedure. ☐ Do NOT chew on surgical site for 1 week. ☐ Do NOT eat hard, crunchy, fried or spicy foods along with small seeds, pretzels, crust, chips, peanuts, popcorn, sesame seeds, kiwi seeds, cereal, bread, pizza, candy, rice, nuts, gum, nachos, steak, wings, sausage, etc. ☐ Eat soft foods such as: yogurt or cottage cheese, soup, well-cooked veggies, soft bread, mashed potatoes, stuffing, pudding or gelatin, sorbet, oatmeal, pasta, eggs, applesauce, bananas, protein shakes, fish. ORAL HYGIENE ☐ Do NOT brush or floss the area for 1 week. Okay to clean other teeth. ☐ Do NOT use WaterPik for 6 months around the surgical site. ☐ Use a Q-tip dipped in Peridex (0.12% Chlorhexidine) to very gently swab surgical site for the first 2 weeks. -

Scholars Journal of Medical Case Reports
DOI: 10.21276/sjmcr.2016.4.6.16 Scholars Journal of Medical Case Reports ISSN 2347-6559 (Online) Sch J Med Case Rep 2016; 4(6):416-419 ISSN 2347-9507 (Print) ©Scholars Academic and Scientific Publishers (SAS Publishers) (An International Publisher for Academic and Scientific Resources) Hereditary Gingival Fibromatosis: A Case Report with Review of Literature Jesudass Govada1, Sridhar Reddy Erugula2, Narendra Kumar Narahari3, Vijay Kumar R4,Rajajee KTSS5, Sudhir Kumar Vujhini6 1Associate Professor, Department of Pedodontics and Preventive Dentistry, Government Dental College and Hospital, RIMS, Kadapa, Andhra Pradesh, India 2Senior lecturer, Department of Oral Pathology, MNR Dental College and Hospital, Sangareddy, Telangana, India 3Assistant Professor, Department of Respiratory Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, India. 4Assistant Professor, Dept. of Dentistry, Govt. Dental College, Ananthapur,, Andhra Pradesh, India 5Reader, Dept of Pedodontics, Anil Neerukonda Institute of Dental Sciences, Visakhapatnam, Andhra Pradesh, India. 6Assistant Professor, Transfusion Medicine, Nizam’s Institute of Medical Sciences, Hyderabad, India *Corresponding author Sudhir Kumar Vujhini Email: [email protected] Abstract: Gingival fibromatosis is characterized by localized or generalized fibrous enlargement of the gingivae, mainly around permanent teeth. Gingival fibromatosis affects only the masticatory mucosa and does not extend beyond the muco-gingival junction. This article describes an unusual case of hereditary gingival fibromatosis with delayed eruption of permanent teeth in an 11 year-old girl and her younger sibling. The patient presented with severely enlarged gingival tissues affecting both arches and multiple retained deciduous. Most of the permanent teeth were not erupted. She had no associated symptoms to suggest any syndrome but there was family history of similar disorder with father and paternal aunt. -

Treating Patients with Drug-Induced Gingival Overgrowth
Source: Journal of Dental Hygiene, Vol. 78, No. 4, Fall 2004 Copyright by the American Dental Hygienists Association Treating Patients with Drug-Induced Gingival Overgrowth Ana L Thompson, Wayne W Herman, Joseph Konzelman and Marie A Collins Ana L. Thompson, RDH, MHE, is a research project manager and graduate student, and Marie A. Collins, RDH, MS, is chair & assistant professor, both in the Department of Dental Hygiene, School of Allied Health Sciences; Wayne W. Herman, DDS, MS, is an associate professor, and Joseph Konzelman, DDS, is a professor, both in the Department of Oral Diagnosis, School of Dentistry; all are at the Medical College of Georgia in Augusta, Georgia. The purpose of this paper is to review the causes and describe the appearance of drug-induced gingival overgrowth, so that dental hygienists are better prepared to manage such patients. Gingival overgrowth is caused by three categories of drugs: anticonvulsants, immunosuppressants, and calcium channel blockers. Some authors suggest that the prevalence of gingival overgrowth induced by chronic medication with calcium channel blockers is uncertain. The clinical manifestation of gingival overgrowth can range in severity from minor variations to complete coverage of the teeth, creating subsequent functional and aesthetic problems for the patient. A clear understanding of the etiology and pathogenesis of drug-induced gingival overgrowth has not been confirmed, but scientists consider that factors such as age, gender, genetics, concomitant drugs, and periodontal variables might contribute to the expression of drug-induced gingival overgrowth. When treating patients with gingival overgrowth, dental hygienists need to be prepared to offer maintenance and preventive therapy, emphasizing periodontal maintenance and patient education.