Long-Term Uncontrolled Hereditary Gingival Fibromatosis: a Case Report
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Effects of Direct Dental Restorations on Periodontium - Clinical and Radiological Study
Effects of direct dental restorations on periodontium - clinical and radiological study Luiza Ungureanu, Albertine Leon, Cristina Nuca, Corneliu Amariei, Doru Petrovici Constanta, Romania Summary The authors have performed a clinical study - 175 crown obturations of class II, II, V and cavities have been analyzed in 125 patients, following their impact on the marginal periodontium and a radi- ological study - consisting of the analysis of 108 proximal amalgam obturations and of their nega- tive effects on the profound periodontium. The results showed alarming percentages (over 80% in the clinical examination and 87% in the radiological examination of improper restorations, which generated periodontal alterations, from gingivitis to chronic marginal progressive periodontitis. The percentage of 59.26% obturations that triggered different degrees of osseous lysis imposed the need of knowing the negative effects of direct restorations on the periodontium and also the impor- tance of applying the specific preventive measures. Key words: dental anatomy, gingival embrasure contact area, under- and over sizing, cervical exten- sion, osseous lysis. Introduction the antagonist tooth can trigger enlargement of the contact point during functional movements. Dental restorations and periodontal health This allows interdental impact of foodstuff, with are closely related: periodontal health is needed devastating consequent effects on interproximal for the correct functioning of all restorations periodontal tissues. while the functional stimulation due to dental Marginal occlusal ridges must be placed restorations is essential for periodontal protection. above the proximal contact surface, and must be Coronal obturations with improper occlusal rounded and smooth so as to allow the access of modeling, oversized proximally or on the dental floss. -
DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity
October 2008 | Volume 4, Number 9 (Special Issue) DENTIN HYPERSENSITIVITY: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity A Supplement to InsideDentistry® Published by AEGISPublications,LLC © 2008 PUBLISHER Inside Dentistry® and De ntin Hypersensitivity: Consensus-Based Recommendations AEGIS Publications, LLC for the Diagnosis & Management of Dentin Hypersensitivity are published by AEGIS Publications, LLC. EDITORS Lisa Neuman Copyright © 2008 by AEGIS Publications, LLC. Justin Romano All rights reserved under United States, International and Pan-American Copyright Conventions. No part of this publication may be reproduced, stored in a PRODUCTION/DESIGN Claire Novo retrieval system or transmitted in any form or by any means without prior written permission from the publisher. The views and opinions expressed in the articles appearing in this publication are those of the author(s) and do not necessarily reflect the views or opinions of the editors, the editorial board, or the publisher. As a matter of policy, the editors, the editorial board, the publisher, and the university affiliate do not endorse any prod- ucts, medical techniques, or diagnoses, and publication of any material in this jour- nal should not be construed as such an endorsement. PHOTOCOPY PERMISSIONS POLICY: This publication is registered with Copyright Clearance Center (CCC), Inc., 222 Rosewood Drive, Danvers, MA 01923. Permission is granted for photocopying of specified articles provided the base fee is paid directly to CCC. WARNING: Reading this supplement, Dentin Hypersensitivity: Consensus-Based Recommendations for the Diagnosis & Management of Dentin Hypersensitivity PRESIDENT / CEO does not necessarily qualify you to integrate new techniques or procedures into your practice. AEGIS Publications expects its readers to rely on their judgment Daniel W. -

DENTAL CALCULUS: a STRATEGIC REVIEW Rajiv Saini1 1.Associate Professor,Department of Periodontology,Pravra Institute of Medical Sciences-Loni
International Journal of Dental and Health Sciences Review Article Volume 01,Issue 05 DENTAL CALCULUS: A STRATEGIC REVIEW Rajiv Saini1 1.Associate Professor,Department of Periodontology,Pravra Institute of Medical Sciences-Loni ABSTRACT: Dental calculus or tartar is an adherent calcified mass that form on the surface of teeth and dental appliance through mineralization of bacterial dental plaque in aqueous environment. Dental calculus plays a vital role in aggravating the periodontal disease by acting as reservoir for the bacterial plaque and providing the protected-covered niche for bacteria to proliferate. Based upon the location of dental calculus in relation to marginal gingiva, it is classified into mainly two types: 1. Supragingival calculus and subgingival calculus. Calcium and phosphate are two salivary ions which are raw materials for dental calculus formation. The various techniques and equipments involved for calculus removal is Hand Instruments, Ultrasonic, Ultrasound Technology and Lasers. Chemotherapeutic agents have been used to supplement the mechanical removal of dental plaque, but a more potent oral rinse with anti-calculus properties to prevent mineralization will be the need of time to suppress calculus formation. Key Words: Periodontitis, Anti-calculus, Periogen. INTRODUCTION: biofilm is that it allows the micro-organisms to stick and to multiply on surfaces. [3] Periodontitis is a destructive inflammatory Mineralization of dental plaque leads to disease of the supporting tissues of the calculus formation. Dynamic state of tooth teeth and is caused either by specific surface is responsible for mineralization of microorganisms or by a group of specific plaque. A continuous exchange of ions is microorganisms, resulting in progressive always happening on the tooth surface with destruction of periodontal ligament and a constant exchange of calcium and alveolar bone with periodontal pocket phosphate ions. -
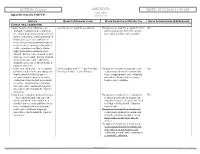
02/23/2018 11:54 AM Appendix Appendix a to Rule 5160-5-01 5160-5-01
ACTION: Original AMENDED DATE: 02/23/2018 11:54 AM Appendix Appendix A to rule 5160-5-01 5160-5-01 SERVICE QUANTITY/FREQUENCY LIMIT OTHER CONDITION OR RESTRICTION PRIOR AUTHORIZATION (PA) REQUIRED CLINICAL ORAL EXAMINATION Comprehensive oral evaluation – A 1 per 5 years per provider per patient No payment is made for a comprehensive No thorough evaluation and recording of oral evaluation performed in conjunc- the extraoral and intraoral hard and soft tion with a periodic oral evaluation. tissues, it includes a dental and medical history and a general health assess- ment. It may encompass such matters as dental caries, missing or unerupted teeth, restorations, occlusal relation- ships, periodontal conditions, peri- odontal charting, tissue anomalies, and oral cancer screening. Interpretation of information may require additional diagnostic procedures, which should be reported separately. Periodic oral evaluation – An evaluation Patient younger than 21: 1 per 180 days No payment is made for a periodic oral No performed to determine any changes in Patient 21 or older: 1 per 365 days evaluation performed in conjunction dental and medical health since a with a comprehensive oral evaluation previous comprehensive or periodic nor within 180 days after a compre- evaluation, it may include periodontal hensive oral evaluation. screening. Interpretation of informa- tion may require additional diagnostic procedures, which should be reported separately. Limited oral evaluation, problem-focused No payment is made if the evaluation is No – An evaluation limited to a specific performed solely for the purpose of oral health problem or complaint, it adjusting dentures, except as specified includes any necessary palliative treat- in Chapter 5160-28 of the Adminis- ment. -

Essential Dental (Pdf)
Dental Essential Plans 2 Plans1 for Individuals & Families with Optional Vision Benefits2 Table of Contents Optional Vision Benefits 5 Why Dental Essential? 2 Exclusions & Limitations 6 Dental Essential & Notice of Privacy Practices 10 Dental Essential Preferred 3 Wisconsin Outline of Coverage 14 Hearing Discounts 4 California Notices 18 Golden Rule Insurance Company is the underwriter of these plans. This product is administered by Dental Benefit Providers, Inc. Policy Forms GRI-DEN3-JR, -01 (AL), -02 (AZ), -03 (AR), -04 (CA), -05 (CO), -06 (CT), (DE), -08 (DC), -09 (FL), -10 (GA), -51 (HI), -12 (IL), -13 (IN), -14 (IA), -15 (KS), -16 (KY), -17 (LA), -19 (MD), -21 (MI), -22 (MN), -23 (MS), -24 (MO), -26 (NE), -28 (NH), -30 (NM), -32 (NC), -33 (ND), -35 (OK), -36 (OR), -37 (PA), -38 (RI), -39 (SC), -40 (SD), -41 (TN), -42 (TX), -43 (UT), -44 (VT), -45 (VA), -47 (WV), and -48 (WI); GRI-DEN3-JR-PB, -11 (ID), -34 (OH), -46 (WA); GRI-DEN3-JR-PBM, -11 (ID), -34 (OH), -46 (WA) 1 Essential Preferred is the only plan available in CO and MN. 2 The optional vision benefit is not available in MN, RI or WA. The ratio of incurred claims to earned premiums (loss-ratio) for total accident and health for Golden Rule Insurance Company in all states in 2019 was 62.4%. This is an outline only and is not intended to serve as a legal interpretation of benefits. Reasonable effort has been made to have this outline represent the intent of contract language. However, the contract language stands alone and the complete terms of the coverage will be determined by the policy. -

Intrusion of Incisors to Facilitate Restoration: the Impact on the Periodontium
Note: This is a sample Eoster. Your EPoster does not need to use the same format style. For example your title slide does not need to have the title of your EPoster in a box surrounded with a pink border. Intrusion of Incisors to Facilitate Restoration: The Impact on the Periodontium Names of Investigators Date Background and Purpose This 60 year old male had severe attrition of his maxillary and mandibular incisors due to a protrusive bruxing habit. The patient’s restorative dentist could not restore the mandibular incisors without significant crown lengthening. However, with orthodontic intrusion of the incisors, the restorative dentist was able to restore these teeth without further incisal edge reduction, crown lengthening, or endodontic treatment. When teeth are intruded in adults, what is the impact on the periodontium? The purpose of this study was to determine the effect of adult incisor intrusion on the alveolar bone level and on root length. Materials and Methods We collected the orthodontic records of 43 consecutively treated adult patients (aged > 19 years) from four orthodontic practices. This project was approved by the IRB at our university. Records were selected based upon the following criteria: • incisor intrusion attempted to create interocclusal space for restorative treatment or correction of excessive anterior overbite • pre- and posttreatment periapical and cephalometric radiographs were available • no incisor extraction or restorative procedures affecting the cementoenamel junction during the treatment period pretreatment pretreatment Materials and Methods We used cephalometric and periapical radiographs to measure incisor intrusion. The radiographs were imported and the digital images were analyzed with Image J, a public-domain Java image processing program developed at the US National Institutes of Health. -

Hereditary Gingival Fibromatosis CASE REPORT
Richa et al.: Management of Hereditary Gingival Fibromatosis CASE REPORT Hereditary Gingival Fibromatosis and its management: A Rare Case of Homozygous Twins Richa1, Neeraj Kumar2, Krishan Gauba3, Debojyoti Chatterjee4 1-Tutor, Unit of Pedodontics and preventive dentistry, ESIC Dental College and Hospital, Rohini, Delhi. 2-Senior Resident, Unit of Pedodontics and preventive dentistry, Oral Health Sciences Centre, Post Correspondence to: Graduate Institute of Medical Education and Research , Chandigarh, India. 3-Professor and Head, Dr. Richa, Tutor, Unit of Pedodontics and Department of Oral Health Sciences Centre, Post Graduate Institute of Medical Education and preventive dentistry, ESIC Dental College and Research, Chandigarh, India. 4-Senior Resident, Department of Histopathology, Oral Health Sciences Hospital, Rohini, Delhi Centre, Post Graduate Institute of Medical Education and Research, Chandigarh, India. Contact Us: www.ijohmr.com ABSTRACT Hereditary gingival fibromatosis (HGF) is a rare condition which manifests itself by gingival overgrowth covering teeth to variable degree i.e. either isolated or as part of a syndrome. This paper presented two cases of generalized and severe HGF in siblings without any systemic illness. HGF was confirmed based on family history, clinical and histological examination. Management of both the cases was done conservatively. Quadrant wise gingivectomy using ledge and wedge method was adopted and followed for 12 months. The surgical procedure yielded functionally and esthetically satisfying results with no recurrence. KEYWORDS: Gingival enlargement, Hereditary, homozygous, Gingivectomy AA swollen gums. The patient gave a history of swelling of upper gums that started 2 years back which gradually aaaasasasss INTRODUCTION increased in size. The child’s mother denied prenatal Hereditary Gingival Enlargement, being a rare entity, is exposure to tobacco, alcohol, and drug. -

Gingivectomy Approaches: a Review
ISSN: 2469-5734 Peres et al. Int J Oral Dent Health 2019, 5:099 DOI: 10.23937/2469-5734/1510099 Volume 5 | Issue 3 International Journal of Open Access Oral and Dental Health REVIEW ARTICLE Gingivectomy Approaches: A Review Millena Mathias Peres1, Tais da Silva Lima¹, Idiberto José Zotarelli Filho1,2*, Igor Mariotto Beneti1,2, Marcelo Augusto Rudnik Gomes1,2 and Patrícia Garani Fernandes1,2 1University Center North Paulista (Unorp) Dental School, Brazil 2Department of Scientific Production, Post Graduate and Continuing Education (Unipos), Brazil Check for *Corresponding author: Prof. Idiberto José Zotarelli Filho, Department of Scientific Production, Post updates Graduate and Continuing Education (Unipos), Street Ipiranga, 3460, São José do Rio Preto SP, 15020-040, Brazil, Tel: +55-(17)-98166-6537 gingival tissue, and can be corrected with surgical tech- Abstract niques such as gingivectomy. Many patients seek dental offices for a beautiful, harmoni- ous smile to boost their self-esteem. At present, there is a Gingivectomy is a technique that is easy to carry great search for oral aesthetics, where the harmony of the out and is usually well accepted by patients, who, ac- smile is determined not only by the shape, position, and col- cording to the correct indications, can obtain satisfac- or of teeth but also by the gingival tissue. The present study aimed to establish the etiology and diagnosis of the gingi- tory results in dentogingival aesthetics and harmony val smile, with the alternative of correcting it with very safe [3]. surgical techniques such as gingivectomy. The procedure consists in the elimination of gingival deformities resulting The procedure consists in the removal of gingival de- in a better gingival contour. -

Dentinal Hypersensitivity: a Review
Dentinal Hypersensitivity: A Review Abstract Dentinal hypersensitivity is generally reported by the patient after experiencing a sharp pain caused by one of several different stimuli. The pain response varies substantially from one person to another. The condition generally involves the facial surfaces of teeth near the cervical aspect and is very common in premolars and canines. The most widely accepted theory of how the pain occurs is Brannstrom’s hydrodynamic theory, fluid movement within the dentinal tubules. The dental professional, using a variety of diagnostic techniques, will discern the condition from other conditions that may cause sensitive teeth. Treatment of the condition can be invasive or non-invasive in nature. The most inexpensive and efficacious first line of treatment for most patients is a dentifrice containing a desensitizing active ingredient such as potassium nitrate and/or stannous fluoride. This review will address the prevalence, diagnosis, and treatment of dentinal hypersensitivity. In addition the home care recommendations will focus on desensitizing dentifrices. Keywords: Dentinal hypersensitivity, hydrodynamic theory, stannous fluoride, potassium nitrate Citation: Walters PA. Dentinal Hypersensitivity: A Review. J Contemp Dent Pract 2005 May;(6)2:107-117. © Seer Publishing 1 The Journal of Contemporary Dental Practice, Volume 6, No. 2, May 15, 2005 Introduction The prevalence of dentinal hypersensitivity Dentifrices and mouth rinses are routinely used has been reported over the years in a variety as a delivery system for therapeutic agents of ways: as greater than 40 million people such as antimicrobials and anti-sensitivity in the U.S. annually1, 14.3% of all dental agents. Therapeutic oral care products are patients2, between 8% and 57% of adult dentate available to assist the patient in the control of population3, and up to 30% of adults at some time dental caries, calculus formation, and dentinal during their lifetime.4 hypersensitivity to name a few. -

Staining and Calculus Formation After 0.12% Chlorhexidine Rinses in Plaque-Free and Plaque Covered Surfaces: a Randomized Trial
www.scielo.br/jaos Staining and calculus formation after 0.12% chlorhexidine rinses in plaque-free and plaque covered surfaces: a randomized trial Fabrício Batistin Zanatta1,2, Raquel Pippi Antoniazzi1, Cassiano Kuchenbecker RÖSING2 1- DDS, School of Dentistry, Division of General Dentistry, Franciscan University Center (UNIFRA), Santa Maria, RS, Brazil. 2- PhD, Post-Graduate Program in Dentistry, Lutheran University of Brazil (ULBRA), Canoas, RS, Brazil. Corresponding address: Fabrício B. Zanatta - Rua Tiradentes, 76/801 - Bairro Centro - 97050730 - Santa Maria, RS - Brasil - Phone: +55 55 33078026 - Fax: +55 51 3338 4221 - e-mail: [email protected] Received: February 2, 2009 - Modification: September 5, 2009 - Accepted: September 28, 2009 ABSTRACT bjectives: Studies concerning side effects of chlorhexidine as related to the presence Oof plaque are scarce. The purpose of this study was to compare the side effects of 0.12% chlorhexidine gluconate (CHX) on previously plaque-free (control group) and plaque-covered surfaces (test group). Methods: This study had a single-blind, randomized, split-mouth, 21 days-experimental gingivitis design, including 20 individuals who abandoned all mechanical plaque control methods during 25 days. After 4 days of plaque accumulation, the individuals had 2 randomized quadrants cleaned, remaining 2 quadrants with plaque-covered dental surfaces. On the fourth day, the individuals started with 0.12% CHX rinsing lasting for 21 days. Stain index intensity and extent as well as calculus formation were evaluated during the experimental period. Results: Intergroup comparisons showed statistically higher (p<0.05) stain intensity and extent index as well as calculus formation over the study in test surfaces as compared to control surfaces. -

Desensitizing Agent Reduces Dentin Hypersensitivity During Ultrasonic Scaling: a Pilot Study Dentistry Section
Original Article DOI: 10.7860/JCDR/2015/13775.6495 Desensitizing Agent Reduces Dentin Hypersensitivity During Ultrasonic Scaling: A Pilot Study Dentistry Section TOMONARI SUDA1, HIROAKI KOBAYASHI2, TOSHIHARU AKIYAMA3, TAKUYA TAKANO4, MISA GOKYU5, TAKEAKI SUDO6, THATAWEE KHEMWONG7, YUICHI IZUMI8 ABSTRACT of the dentin hypersensitivity agent. Evaluation of effects on Background: Dentin hypersensitivity can interfere with optimal dentin hypersensitivity was determined by a questionnaire and periodontal care by dentists and patients. The pain associated visual analog scale (VAS) pain scores after ultrasonic scaling. with dentin hypersensitivity during ultrasonic scaling is intolerable The statistical analysis was performed using the paired Student for patient and interferes with the procedure, particularly during t-test and Spearman rank correlation coefficient. supportive periodontal therapy (SPT) for patients with gingival Results: The desensitizing agent reduced the mean VAS pain recession. score from 69.33 ± 16.02 at baseline to 26.08 ± 27.99 after Aim: This study proposed to evaluate the desensitizing effect of application. The questionnaire revealed that >80% patients the oxalic acid agent on pain caused by dentin hypersensitivity were satisfied and requested the application of the desensitizing during ultrasonic scaling. agent for future ultrasonic scaling sessions. Materials and Methods: This study involved 12 patients who Conclusion: This study shows that the application of the oxalic were incorporated in SPT program and complained of dentin acid agent considerably reduces pain associated with dentin hypersensitivity during ultrasonic scaling. We examined the hypersensitivity experienced during ultrasonic scaling. This availability of the oxalic acid agent to compare the degree of pain control treatment may improve patient participation and pain during ultrasonic scaling with or without the application treatment efficiency. -

Dental Cementum Reviewed: Development, Structure, Composition, Regeneration and Potential Functions
Braz J Oral Sci. January/March 2005 - Vol.4 - Number 12 Dental cementum reviewed: development, structure, composition, regeneration and potential functions Patricia Furtado Gonçalves 1 Enilson Antonio Sallum 1 Abstract Antonio Wilson Sallum 1 This article reviews developmental and structural characteristics of Márcio Zaffalon Casati 1 cementum, a unique avascular mineralized tissue covering the root Sérgio de Toledo 1 surface that forms the interface between root dentin and periodontal Francisco Humberto Nociti Junior 1 ligament. Besides describing the types of cementum and 1 Dept. of Prosthodontics and Periodontics, cementogenesis, attention is given to recent advances in scientific Division of Periodontics, School of Dentistry understanding of the molecular and cellular aspects of the formation at Piracicaba - UNICAMP, Piracicaba, São and regeneration of cementum. The understanding of the mechanisms Paulo, Brazil. involved in the dynamic of this tissue should allow for the development of new treatment strategies concerning the approach of the root surface affected by periodontal disease and periodontal regeneration techniques. Received for publication: October 01, 2004 Key Words: Accepted: December 17, 2004 dental cementum, review Correspondence to: Francisco H. Nociti Jr. Av. Limeira 901 - Caixa Postal: 052 - CEP: 13414-903 - Piracicaba - S.P. - Brazil Tel: ++ 55 19 34125298 Fax: ++ 55 19 3412 5218 E-mail: [email protected] 651 Braz J Oral Sci. 4(12): 651-658 Dental cementum reviewed: development, structure, composition, regeneration and potential functions Introduction junction (Figure 1). The areas and location of acellular Cementum is an avascular mineralized tissue covering the afibrillar cementum vary from tooth to tooth and along the entire root surface. Due to its intermediary position, forming cementoenamel junction of the same tooth6-9.