Innovative Approaches
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview
1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview This Weekly Bulletin focuses on selected acute public health emergencies Contents occurring in the WHO African Region. The WHO Health Emergencies Programme is currently monitoring 71 events in the region. This week’s edition covers key new and ongoing events, including: 2 Overview Humanitarian crisis in Niger 3 - 6 Ongoing events Ebola virus disease in Democratic Republic of the Congo Humanitarian crisis in Central African Republic 7 Summary of major issues, challenges Cholera in Burundi. and proposed actions For each of these events, a brief description, followed by public health measures implemented and an interpretation of the situation is provided. 8 All events currently being monitored A table is provided at the end of the bulletin with information on all new and ongoing public health events currently being monitored in the region, as well as recent events that have largely been controlled and thus closed. Major issues and challenges include: The humanitarian crisis in Niger and the Central African Republic remains unabated, characterized by continued armed attacks, mass displacement of the population, food insecurity, and limited access to healthcare services. In Niger, the extremely volatile security situation along the borders with Burkina Faso, Mali, and Nigeria occasioned by armed attacks from Non-State Actors as well as resurgence in inter-communal conflicts, is contributing to an unprecedented mass displacement of the population along with its associated consequences. Seasonal flooding with huge impact as well as high morbidity and mortality rates from common infectious diseases have also complicated response to the humanitarian crisis. -

Republique Du Cameroun Republic of Cameroon Details Des Projets Par Region, Departement, Chapitre, Programme Et Action Extreme N
REPUBLIQUE DU CAMEROUN REPUBLIC OF CAMEROON PAIX - TRAVAIL - PATRIE PEACE - WORK - FATHERLAND DETAILS DES PROJETS PAR REGION, DEPARTEMENT, CHAPITRE, PROGRAMME ET ACTION OPERATIONS BOOK PER REGION, DIVISION, HEAD, PROGRAMME AND ACTION Exercice/ Financial year : 2017 Région EXTREME NORD Region FAR NORTH Département DIAMARE Division En Milliers de FCFA In Thousand CFAF Année de Tâches démarrage Localité Montant AE Montant CP Tasks Starting Year Locality Montant AE Montant CP Chapitre/Head MINISTERE DE L'ADMINISTRATION TERRITORIALE ET DE LA DECENTRALISATION 07 MINISTRY OF TERRITORIAL ADMINISTRATION AND DECENTRALIZATION PETTE : Reprogrammation des travaux de construction de la sous-préfecture (Phase 1) PETTE 50 000 50 000 2 017 PETTE : Reprogramming of the construction of the Sub-Divisional Office MAROUA: Règlement de la maîtrise d'œuvre pour la construction résidence Préfet MAROUA 5 350 5 350 MAROUA: Payment of the project management of the construction of the residence of 2 017 the SDO MAROUA: Règlement des travaux de la première phase de construction résidence Préfet MAROUA 80 000 80 000 2 017 MAROUA: Payment of the construction of the residence of the SDO Total Chapitre/Head MINATD 135 350 135 350 Chapitre/Head MINISTERE DE LA JUSTICE 08 MINISTRY OF JUSTICE Cour d'Appel de l'Extrême-Nord : Etudes architecturales et géotechniques pour la MAROUA I 40 000 5 000 construction 2 017 Architectural and geotchnical construction studies of the Court of Appeal of Far-North Total Chapitre/Head MINJUSTICE 40 000 5 000 Chapitre/Head MINISTERE DES MARCHES -

Cameroon |Far North Region |Displacement Report Round 15 | 03– 15 September 2018
Cameroon |Far North Region |Displacement Report Round 15 | 03– 15 September 2018 Cameroon | Far North Region | Displacement Report | Round 15 | 03– 15 September 2018 The opinions expressed in the report are those of the authors and do not necessarily reflect the views of the International Organization for Migration (IOM). The designations employed and the presentation of material throughout the report do not imply the expression of any opinion whatsoever on the part of IOM concerning the legal status of any country, territory, city or area, or of its authorities, or concerning its frontiers or boundaries1. IOM is committed to the principle that humane and orderly migration benefits migrants and society. As an intergovernmental organization, IOM acts with its partners in the international community to assist in meeting the operational challenges of migration, advance understanding of migration issues, encourage social and economic development through migration and uphold the human dignity and well-being of migrants. International Organization for Migration Cameroon Mission Maroua Sub-Office UN House Comice Maroua Far North Region Cameroon Tel.: +237 222 20 32 78 E-mail: [email protected] Websites: https://ww.iom.int/fr/countries/cameroun and https://displacement.iom.int/cameroon All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior written permission of the publisher. 1The maps included in this report are illustrative. The representations and the use of borders and geographic names may include errors and do not imply judgment on legal status of territories nor acknowledgement of borders by the Organization. -

Rapport De Situation N° 15 Épidémie De Cholera Dans La Région De L’Extrême-Nord Cameroun - 18 Septembre 2019
RAPPORT DE SITUATION N° 15 ÉPIDÉMIE DE CHOLERA DANS LA RÉGION DE L’EXTRÊME-NORD CAMEROUN - 18 SEPTEMBRE 2019 - Réunion du comité Régional de lutte contre le choléra présidé par le Sensibilisation contre le choléra à Boboyo par l’équipe CERPLE, ECD Gouverneur de la Région de l’Extrême-Nord, 12/09/2019 Kaélé et AAEDC/Unicef, Région de l’Extrême-Nord, 08/09/2019 I. FAITS SAILLANTS • 12/09/2019 : Deuxième réunion du comité Régional de Lutte contre la Choléra présidée par le Gouverneur de la région de l’Extrême-Nord ; • 16/09/2019 : 01 nouveau décès hospitalier enregistré dans le district de santé Kaélé, aire de santé Kaélé ; • 3 nouveaux cas notifiés à Zouayé (DS Karhay) après 26 jours de notification zéro ; • À ce jour : o 243 cas suspects enregistrés dans les districts de santé Kaélé, Kar Hay, Moutourwa, Maroua 1 et Guidiguis ; o 08/18 échantillons confirmés par le laboratoire de la CNPS de Maroua ; o 11 décès (dont 04 en communauté et 07 hospitaliers) enregistrés dans les aires de santé Midjivin, Gané, Mindjil et Boboyo ; o Taux de létalité : 4,5%. 1 II. SITUATION ÉPIDÉMIOLOGIQUE Cas Décès 10 8 6 4 Nombre de cas 2 0 7/5/2019 8/4/2019 8/9/2019 9/3/2019 9/8/2019 6/25/2019 6/30/2019 7/10/2019 7/15/2019 7/20/2019 7/25/2019 7/30/2019 8/14/2019 8/19/2019 8/24/2019 8/29/2019 9/13/2019 9/18/2019 Date de début des symptômes Figure 1 : Courbe épidémique des cas suspects et des décès de choléra dans la Région de l’Extrême-Nord, 18/09/2019 Tableau 1 : Résumé de la situation épidémiologique au 18/09/2019 DS DS Binder DS DS Kaélé DS Kar Hay DS Moutourwa -

Patrimoine Et Patrimonialisation Au Cameroun Les Diy-Gid-Biy Des Monts Mandara Septentrionaux Pour Une Étude De Cas
Patrimoine et patrimonialisation au Cameroun Les Diy-gid-biy des monts Mandara septentrionaux pour une étude de cas Thèse Jean-Marie Datouand Djoussou Doctorat en ethnologie et patrimoine Philosophiae Doctor (Ph. D.) Québec, Canada © Jean-Marie Datouang Djoussou, 2014 RÉSUMÉ Portant le titre Patrimoine et patrimonialisation au Cameroun: les Diy-gid-biy des monts Mandara septentrionaux pour une étude de cas, notre thèse est un chainon d'éléments argumentatifs orientés vers l'élucidation du statut de bien patrimonial. Elle s'inscrit dans le champ des recherches considérant le patrimoine et la patrimonialisation comme un ensemble de codes discursifs dont l'intérêt pour l'anthropologue est la compréhension du sens et non de la caractéristique ontique. Il s'agit de l'intelligibilité des rapports aux éléments patrimoniaux qui passe par une mise en évidence de la patrimonialité, l'expression des changements et des conséquences sociaux patrimogènes. De ce fait, le travail met en discours les mises en patrimoine et les rapports sous-tendant le statut d'élément patrimonial. D'une manière générale, c'est un exposé sur le grand paysage patrimonial du Cameroun à travers un regard à la fois vertical et horizontal qui souligne les différentes formes de constructions patrimoniales ayant eu cours dans ledit pays. Il est donc question d‘une mise en relief de l'alchimie de la construction patrimoniale, et donc, du comment les choses deviennent patrimoniales. Pour ce faire, notre thèse se penche sur l'analyse des processus de mise en patrimoine en les considérant dans deux échelles de temps focalisées respectivement sur leur genèse historique et leur construction procédurale actuelle. -

Proceedingsnord of the GENERAL CONFERENCE of LOCAL COUNCILS
REPUBLIC OF CAMEROON REPUBLIQUE DU CAMEROUN Peace - Work - Fatherland Paix - Travail - Patrie ------------------------- ------------------------- MINISTRY OF DECENTRALIZATION MINISTERE DE LA DECENTRALISATION AND LOCAL DEVELOPMENT ET DU DEVELOPPEMENT LOCAL Extrême PROCEEDINGSNord OF THE GENERAL CONFERENCE OF LOCAL COUNCILS Nord Theme: Deepening Decentralization: A New Face for Local Councils in Cameroon Adamaoua Nord-Ouest Yaounde Conference Centre, 6 and 7 February 2019 Sud- Ouest Ouest Centre Littoral Est Sud Published in July 2019 For any information on the General Conference on Local Councils - 2019 edition - or to obtain copies of this publication, please contact: Ministry of Decentralization and Local Development (MINDDEVEL) Website: www.minddevel.gov.cm Facebook: Ministère-de-la-Décentralisation-et-du-Développement-Local Twitter: @minddevelcamer.1 Reviewed by: MINDDEVEL/PRADEC-GIZ These proceedings have been published with the assistance of the German Federal Ministry for Economic Cooperation and Development (BMZ) through the Deutsche Gesellschaft für internationale Zusammenarbeit (GIZ) GmbH in the framework of the Support programme for municipal development (PROMUD). GIZ does not necessarily share the opinions expressed in this publication. The Ministry of Decentralisation and Local Development (MINDDEVEL) is fully responsible for this content. Contents Contents Foreword ..............................................................................................................................................................................5 -

WEEKLY BULLETIN on OUTBREAKS and OTHER EMERGENCIES Week 49: 2 - 8 December 2019 Data As Reported By: 17:00; 8 December 2019
WEEKLY BULLETIN ON OUTBREAKS AND OTHER EMERGENCIES Week 49: 2 - 8 December 2019 Data as reported by: 17:00; 8 December 2019 REGIONAL OFFICE FOR Africa WHO Health Emergencies Programme 1 62 51 12 New event Ongoing events Outbreaks Humanitarian crises 1 179 0 11 1 Mali 1 0 3 1 9 969 54 Senegal 25 916 255 1 0 Niger 1 194 0 Guinea Burkina Faso 52 0 Chad 4 690 18 26 2 2 089 21 Côte d’Ivoire Nigeria Sierra léone 9 0 839 4 South Sudan Ethiopia 804 179 118 2 9 437 7 4 Ghana 3 787 192 Cameroon Central African 3 0 Liberia 3 963 23 Benin Republic 16 0 54 739 0 1 170 14 1 071 53 1 638 40 Togo 55 476 275 1 0 Democratic Republic Uganda 95 20 1 569 5 3 0 of Congo 4 758 37 Congo Kenya 3 320 2 209 1 1 Legend 6 0 2 788 34 269 058 5 430 Measles Humanitarian crisis 11 434 0 26 505 465 Burundi Hepatitis E 7 392 429 2 823 Monkeypox 76 0 50 8 1 064 6 Yellow fever Lassa fever Dengue fever 4 761 95 Cholera Angola Ebola virus disease Rift Valley Fever Comoros 60 0 1 0 Chikungunya 144 0 cVDPV2 Zambia 1 0 Leishmaniasis Malaria Mozambique Floods Plague Cases Namibia Countries reported in the document Deaths Non WHO African Region WHO Member States with no reported events 6 746 56 N W E 3 0 Lesotho 59 0 South Africa 20 0 S Graded events † 3 15 2 Grade 3 events Grade 2 events Grade 1 events 37 22 20 21 Ungraded events PB ProtractedProtracted 3 3 events events Protracted 2 events ProtractedProtracted 1 1 events event 1 Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview This Weekly Bulletin focuses on public health emergencies occurring in the WHO Contents African Region. -

Republique Du Cameroun Ministere De L'energie Et De L'eau Contrat D'affermage Du Service Public De L'alimentation En Eau
REPUBLIQUE DU CAMEROUN MINISTERE DE L'ENERGIE ET DE L’EAU CONTRAT D'AFFERMAGE DU SERVICE PUBLIC DE L’ALIMENTATION EN EAU POTABLE DES CENTRES URBAINS ET PERIURBAINS DU CAMEROUN SOMMAIRE TITRE I – RÉGIME DE L'AFFERMAGE............................................................................... 6 Article 1 - Définitions ..............................................................................................................6 Article 2 - Valeur de l’exposé et des annexes..........................................................................9 Article 3 - Objet du Contrat d'Affermage..................................................................................9 Article 4 - Objet de l’Affermage...............................................................................................9 Article 5 - Définition du Périmètre d'Affermage......................................................................10 Article 6 - Révision du Périmètre d'Affermage.......................................................................10 Article 7 - Biens de retour .....................................................................................................10 Article 8 - Régime de Biens de Retour..................................................................................12 Article 9 - Renouvellement des Biens de Retour ...................................................................13 Article 10 - Inventaire des Biens de Retour.............................................................................13 Article 11 - Biens -

Review of Initiatives to Assess and Secure the Land Tenure Rights of Communities in Northern Cameroon
Review of initiatives to assess and secure the land tenure rights of communities in Northern Cameroon Kossoumna Liba’a Natali November 2018 KOSSOUMNA LIBA’A Natali teaches geography at the École Normale Supérieure and at the Faculty of Arts, Lettres and Human Sciences of Maroua University (Cameroon). He is interested in the management of rural territories and of natural resources, in questions of marginality, ethnic minorities and pastoralism. LandCam : Securing land and resource rights and improving governance in the Cameroon Cameroon has initiated a reform of its land and natural resources legislation. ImplementedUn projet by CED CED,, RELUF ARELUFA et IIED and IIED, the LandCam project supports this Un projet CED, RELUFA et IIED Un projet CED, RELUFA et IIED effort by piloting approaches on the ground and helping citizens engage in the reform process. www.landcam.org The Centre for Environment and Development (CED) is an independent organisation working to promote environmental justice and protect the rights, interests, culture and aspirations of local and indigenous communities in Central Africa. www.cedcameroun.org The Network for the Fight Against Hunger (RELUFA) is a platform of civil society and grassroots community actors created in 2001, which aims to address systemic problems that lead to poverty, hunger and social, economic and environmental injustices in Cameroon. www.relufa.org The International Institute for Environment and Development (IIED) promotes sustainable development by linking local priorities to global challenges. We supports some of the world’s most vulnerable populations to make their voices heard in decision-making. www.iied.org Table of contents Acronyms 4 Summary 5 Introduction 6 Methodology 7 1. -
Displacement Tracking Matrix I Dtm
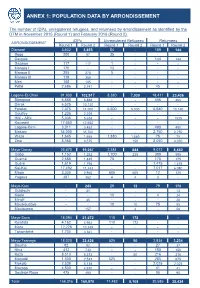
ANNEX 1: POPULATION DATA BY ARRONDISSEMENT The number of IDPs, unregistered refugees, and returnees by arrondissement as identified by the DTM in November 2015 (Round 1) and February 2016 (Round 2). IDPs Unregistered Refugees Returnees ARRONDISSEMENT Round 1 Round 2 Round 1 Round 2 Round 1 Round 2 Diamaré 3,602 3,655 54 - 189 144 Bogo 200 57 35 - - - Dargala - - - - 144 144 Gazawa 117 117 1 - - - Maroua I 170 - 13 - - - Maroua II 205 270 5 - - - Maroua III 119 365 - - - - Meri 105 105 - - - - Pétté 2,686 2,741 - - 45 - Logone-Et-Chari 91,930 102,917 8,380 7,030 18,411 23,436 Blangoua 6,888 6,888 - - 406 406 Darak 6,525 10,120 - - - - Fotokol 7,375 11,000 6,500 5,000 6,640 10,140 Goulfey 1,235 2,229 - - - - Hilé - Alifa 5,036 5,638 - - - 1525 Kousséri 17,650 17,650 - - - - Logone-Birni 3,011 3,452 - - 490 490 Makary 34,000 35,700 - - 2,750 2,750 Waza 1,645 1,665 1,880 1,880 75 75 Zina 8,565 8,575 - 150 8,050 8,050 Mayo-Danay 26,670 19,057 2,384 844 9,072 8,450 Gobo 1,152 1,252 1,700 235 390 595 Guémé 2,685 1,445 75 - 175 175 Guéré 1,619 1,795 - - 1,475 1,475 Kai-Kai 17,492 11,243 - - 7,017 6,080 Maga 3,335 2,960 605 605 12 125 Yagoua 387 362 4 4 3 - Mayo-Kani - 243 29 12 79 170 Guidiguis - 41 - 13 Kaélé - - 19 - 4 24 Mindif - 45 - - - 20 Moulvoudaye - - 10 10 75 55 Moutourwa - 157 - 2 - 58 Mayo-Sava 18,094 21,672 110 172 - - Kolofata 4,162 4,962 110 172 - - Mora 12,228 13,349 - - - - Tokombéré 1,704 3,361 - - - - Mayo-Tsanaga 18,020 22,426 525 50 2,834 3,234 Bourha 82 92 - - 27 37 Hina 412 730 - - 150 150 Koza 8,513 8,513 - 50 216 216 Mogodé 1,500 2,533 525 - 285 675 Mokolo 2,538 5,138 - - 2,025 2,025 Mozogo 4,500 4,930 - - 41 41 Soulèdé-Roua 475 490 - - 90 90 TotalDTM Cameroon 158,316 Round169,970 1 – November 11,482 2015 8,108 30,585 35,434 1 ANNEXE 2: LOCATIONS OF DISPLACED INDIVIDUALS Location of internally displaced persons, unregistered refugees, and returnees in the Far North region. -

Centre D'examen De Maroua
AO/CBGI REPUBLIQUE DU CAMEROUN REPUBLIC OF CAMEROON Paix –Travail – Patrie Peace – Work – Fatherland -------------- --------------- MINISTERE DE LA FONCTION PUBLIQUE MINISTRY OF THE PUBLIC SERVICE ET DE LA REFORME ADMINISTRATIVE AND ADMINISTRATIVE REFORM --------------- --------------- SECRETARIAT GENERAL SECRETARIAT GENERAL --------------- --------------- DIRECTION DU DEVELOPPEMENT DEPARTMENT OF STATE HUMAN DES RESSOURCES HUMAINES DE L’ETAT RESSOURCES DEVELOPMENT --------------- --------------- SOUS DIRECTION DES CONCOURS SUB DEPARTMENT OF EXAMINATIONS ------------------ -------------------- TEST DE SÉLECTION POUR LE RECRUTEMENT DE 1000 INSTITUTEURS DE L’ENSEIGNEMENT MATERNEL ET PRIMAIRE RELEVANT DU CODE DU TRAVAIL POUR LE COMPTE DU MINISTÈRE DE L’ÉDUCATION DE BASE SESSION 201 8 CENTRE D’EXAMEN DE MAROUA LISTE DES CANDIDATS AUTORISÉS À SUBIR LES ÉPREUVES ÉCRITES DU 08 DÉCEMBRE 2018 RÉGION NO MATRICULE NOMS ET PRÉNOMS DATE ET LIEU DE NAISSANCE SEXE LANGUE D’ORIGINE DÉPARTEMENT D’ORIGINE 1. ICM00482 AAZETI CHRISTIANE épse DANAH 24/04/1984 A GAROUA F EN MAYO KANI F 2. ICM00926 ABAÏCHO ABAKOURA 31/12/1985 A MAKARY M EN LOGONE ET CHARI F 3. ICM01450 ABAICHO AHMAT 20/01/1987 A BODO M EN LOGONE ET CHARI F 4. ICM03345 ABAICHO OUSMAN MAKAYE 01/01/1990 A MAKARY M EN LOGONE ET CHARI F 5. ICM01423 ABAIGUEIME ALADJI 03/01/1987 A WOULKY M EN LOGONE ET CHARI F MINFOPRA/SG/DDRHE/SDC |Liste générale des candidats Instituteurs de l’Enseignement Maternel et Primaire_Maroua, session 2018 Page 1 6. ICM05052 ABAKACHI KALI 30/09/1992 A MAKARY M EN LOGONE ET CHARI F 7. ICM04003 ABAKAI JEAN 31/12/1990 A MBOUKJANG M EN MAYO DANAY F 8. ICM06046 ABAKAI MATHIAS 13/11/1995 A KAI KAI M EN MAYO DANAY F 9. -
Pachyderm S P E C I E S S U R V I V a L 1995 Number 19 C O M M I S S I O N Contents
1995 Number 19 Pachyderm S P E C I E S S U R V I V A L 1995 Number 19 C O M M I S S I O N Contents 1 Chairman’s Report: Asian Rhino Specialist Group Mohd Khan bin Momin Khan with Thomas J. Foose 2 Rapport du Président: Groupe de SpéciaIistes du Rhinocéros Asiatique Editor Greg Overton Mohd Khan bin Momin Khan avec Thomas J. Foose Editorial Board Holly Dublin Chryssee Martin 4 Chairman’s Report: African Rhino Specialist Group Mark Stanley Price Martin Brooks Nico Van Strien Lucy Vigne Clive Walker 5 Rapport du Président: Groupe de SpéciaIistes du All correspondence, including enquiries about subscription, Rhinocéros Africain should be sent to: Martin Brooks The Editor Pachyderm WWF Regional Office PO Box 62440 7 Chairman’s Report: African Elephant Specialist Group Nairobi, Kenya Holly T. Dublin Tel: 254-2-331543/332963 Fax: 254-2-332878 E-mail: [email protected] E-mail: [email protected] 8 Rapport de la Présidente: Groupe de SpéciaIistes de I’EIéphant Africain Holly T. Dublin 10 African Elephant Specialist Group Meeting, Mombasa, Kenya, May 27th to June 1st, 1994: Presentations and Working Group Recommendations Publicationn costs for this issue have 11 Human-Elephant Conflict: the Challenge Ahead been provided by the United States Fish and Wildlife Service Kadzo Kangwana Production supported by: United States Fish and Wildlife Services 15 The Current Status of Human-Elephant Conflict in Kenya Winnie Kiiru Cover photo: An Amboseli elephant with her calf IUCNThe World Conservation Union Photo credit: Kadzo Kangwana Pachyderm No.