Health Emergency Information and Risk Assessment Health Emergency Information and Risk Assessment Overview
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Medical School Rural Tracks in the US Policy Brief: September 2013
Medical School Rural Tracks in the US Policy brief: September 2013 Key points: A rural track (RT) is a program within an existing school of medicine designed to identify, admit, nurture and educate students who have a declared interest in future rural practice with the goal of increasing the number of graduates who enter and remain in rural practice. Rural background and rural commitment are strongly sought applicant characteristics. Community involvement and commitment to primary care in general and Family Medicine in particular are common selection criteria. Many RTs provide for admission of students who would otherwise not be admitted to medical school. Many RTs have dedicated scholarships for their students. Most RTs exist in public medical schools that confer the MD degree and involve 5% to 10% of the students in each class. RT curriculum elements in preclinical years expose students to rural-related topics and include early rural clinical exposure. The major RT curriculum element in the clinical years is lengthy rural clinical experience. Longer rural experience is positively related to rural practice choice. RTs serve a social function by forming a network of like-minded students and faculty. Most RTs are not permanently funded by their medical school and depend on external funding. Based on limited data, the annual cost of running a RT that serves 15 to 25 students per class (10% to 15% of total SOM population) ranges between $350,000 and $600,000. This amount excludes scholarships, but may include payments to rural clinical faculty preceptors. The mean percentage of RT graduates reported to be choosing “primary care” residencies is 65%. -

HRSA's Patient Safety and Clinical Pharmacy Services Collaborative
HRSA’s Patient Safety and Clinical Pharmacy Services Collaborative (PSPC) Krista M. Pedley, PharmD, MS Collaborative Improvement Advisor Department of Health and Human Services (HHS) Health Resources and Services Administration (HRSA) Healthcare Systems Bureau (HSB) Office of Pharmacy Affairs (OPA) 1 What is the Collaborative? • Improve patient safety, improve health outcomes, through integration of clinical pharmacy services • Rapid improvement method – uses IHI model • Leading practices come from the field • Principle of “All Teach, All Learn” 2 How Does the PSPC Create Improvements? • 16 mon th rapid l earni ng mod el • Focused on improving health outcomes • Led by an expert faculty and national leaders • Creates community of learning • Learning Sessions and Action Periods are venues for change • Improvements are tracked and shared for mutual benefit 3 Institute of Medicine Findings on PtitSftPatient Safety and dE Errors • Medication Errors are Most Common • Injure 1.5 Million People Annually • Cost Billions Annually “…for every dollar spent on ambulatory medications, another dollar is spent to treat new health problems caused bhby the me dication. ” 4 HRSA’s Commitment • StSupport programs to provide th e b est and saf est care in the Nation • Take previously supported Collaboratives with documented improvements to the next level • Going beyond one disease at a time to full patient-centered care 5 Patient Safety and Clinical Pharmacy Services Collaborative (PSPC): Aim “Committed to saving and enhancing thousands of lives a year by achieving optimal health outcomes and eliminating adverse drug events through increased clinical pharmacy services for the patients we serve.” 6 PSPC Performance Goals 1. All T eams will h ave a CPS process. -
De 40 MINMAP Région Du Nord SYNTHESE DES DONNEES SUR LA BASE DES INFORMATIONS RECUEILLIES
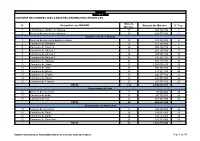
MINMAP Région du Nord SYNTHESE DES DONNEES SUR LA BASE DES INFORMATIONS RECUEILLIES Nbre de N° Désignation des MO/MOD Montant des Marchés N° Page Marchés 1 Communauté Urbaine de Garoua 11 847 894 350 3 2 Services déconcentrés régionaux 20 528 977 000 4 Département de la Bénoué 3 Services déconcentrés départementaux 10 283 500 000 6 4 Commune de Barndaké 13 376 238 000 7 5 Commune de Bascheo 16 305 482 770 8 6 Commune de Garoua 1 11 201 187 000 9 7 Commune de Garoua 2 26 498 592 344 10 8 Commune de Garoua 3 22 735 201 727 12 9 Commune de Gashiga 21 353 419 404 14 10 Commune de Lagdo 21 2 026 560 930 16 11 Commune de Pitoa 18 360 777 700 18 12 Commune de Bibémi 18 371 277 700 20 13 Commune de Dembo 11 300 277 700 21 14 Commune de Ngong 12 235 778 000 22 15 Commune de Touroua 15 187 777 700 23 TOTAL 214 6 236 070 975 Département du Faro 16 Services déconcentrés 5 96 500 000 25 17 Commune de Beka 15 230 778 000 25 18 Commune de Poli 22 481 554 000 26 TOTAL 42 808 832 000 Département du Mayo-Louti 19 Services déconcentrés 6 196 000 000 28 20 Commune de Figuil 16 328 512 000 28 21 Commune de Guider 28 534 529 000 30 22 Commune de Mayo Oulo 24 331 278 000 32 TOTAL 74 1 390 319 000 MINMAP / DIVISION DE LA PROGRAMMATION ET DU SUIVI DES MARCHES PUBLICS Page 1 de 40 MINMAP Région du Nord SYNTHESE DES DONNEES SUR LA BASE DES INFORMATIONS RECUEILLIES Nbre de N° Désignation des MO/MOD Montant des Marchés N° Page Marchés Département du Mayo-Rey 23 Services déconcentrés 7 152 900 000 35 24 Commune de Madingring 14 163 778 000 35 24 Commune de Rey Bouba -

Cameroon : Adamawa, East and North Rgeions
CAMEROON : ADAMAWA, EAST AND NORTH RGEIONS 11° E 12° E 13° E 14° E N 1125° E 16° E Hossere Gaval Mayo Kewe Palpal Dew atan Hossere Mayo Kelvoun Hossere HDossere OuIro M aArday MARE Go mbe Trabahohoy Mayo Bokwa Melendem Vinjegel Kelvoun Pandoual Ourlang Mayo Palia Dam assay Birdif Hossere Hosere Hossere Madama CHARI-BAGUIRMI Mbirdif Zaga Taldam Mubi Hosere Ndoudjem Hossere Mordoy Madama Matalao Hosere Gordom BORNO Matalao Goboum Mou Mayo Mou Baday Korehel Hossere Tongom Ndujem Hossere Seleguere Paha Goboum Hossere Mokoy Diam Ibbi Moukoy Melem lem Doubouvoum Mayo Alouki Mayo Palia Loum as Marma MAYO KANI Mayo Nelma Mayo Zevene Njefi Nelma Dja-Lingo Birdi Harma Mayo Djifi Hosere Galao Hossere Birdi Beli Bili Mandama Galao Bokong Babarkin Deba Madama DabaGalaou Hossere Goudak Hosere Geling Dirtehe Biri Massabey Geling Hosere Hossere Banam Mokorvong Gueleng Goudak Far-North Makirve Dirtcha Hwoli Ts adaksok Gueling Boko Bourwoy Tawan Tawan N 1 Talak Matafal Kouodja Mouga Goudjougoudjou MasabayMassabay Boko Irguilang Bedeve Gimoulounga Bili Douroum Irngileng Mayo Kapta Hakirvia Mougoulounga Hosere Talak Komboum Sobre Bourhoy Mayo Malwey Matafat Hossere Hwoli Hossere Woli Barkao Gande Watchama Guimoulounga Vinde Yola Bourwoy Mokorvong Kapta Hosere Mouga Mouena Mayo Oulo Hossere Bangay Dirbass Dirbas Kousm adouma Malwei Boulou Gandarma Boutouza Mouna Goungourga Mayo Douroum Ouro Saday Djouvoure MAYO DANAY Dum o Bougouma Bangai Houloum Mayo Gottokoun Galbanki Houmbal Moda Goude Tarnbaga Madara Mayo Bozki Bokzi Bangei Holoum Pri TiraHosere Tira -

National Healthcare Quality and Disparities Report CHARTBOOK on RURAL HEALTH CARE
National Healthcare Quality and Disparities Report CHARTBOOK ON RURAL HEALTH CARE Agency for Healthcare Research and Quality Advancing Excellence in Health Care www.ahrq.gov This document is in the public domain and may be used and reprinted without permission. Citation of the source is appreciated. Suggested citation: National Healthcare Quality and Disparities Report chartbook on rural health care. Rockville, MD: Agency for Healthcare Research and Quality; October 2017. AHRQ Pub. No. 17(18)-0001-2-EF. NATIONAL HEALTHCARE QUALITY AND DISPARITIES REPORT CHARTBOOK ON RURAL HEALTH CARE U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES Agency for Healthcare Research and Quality 540 Gaither Road Rockville, MD 20850 AHRQ Publication No. 17(18)-0001-2-EF October 2017 www.ahrq.gov/research/findings/nhqrdr/index.html ACKNOWLEDGMENTS The National Healthcare Quality and Disparities Report (QDR) is the product of collaboration among agencies across the U.S. Department of Health and Human Services (HHS). Many individuals guided and contributed to this effort. Without their magnanimous support, the report would not have been possible. Specifically, we thank: Authors: Barbara Barton (AHRQ), Irim Azam (AHRQ). Primary AHRQ Staff: Gopal Khanna, Sharon Arnold, Jeff Brady, Erin Grace, Karen Chaves, Nancy Wilson, Darryl Gray, Barbara Barton, Doreen Bonnett, and Irim Azam. HHS Interagency Workgroup for the QDR: Girma Alemu (HRSA), Nancy Breen (NIH-NIMHD), Victoria Cargill (NIH), Hazel Dean (CDC), Kirk Greenway (IHS), Chris Haffer (CMS-OMH), Edwin Huff (CMS), DeLoris Hunter (NIH-NIMHD), Sonja Hutchins (CDC), Ruth Katz (ASPE), Shari Ling (CMS), Darlene Marcoe (ACF), Tracy Matthews (HRSA), Ernest Moy (CDC-NCHS), Curt Mueller (HRSA), Ann Page (ASPE), Kathleen Palso (CDC-NCHS), D.E.B Potter (ASPE), Asel Ryskulova (CDC-NCHS), Adelle Simmons (ASPE), Marsha Smith (CMS), Caroline Taplin (ASPE), Emmanuel Taylor (NCI), Nadarajen Vydelingum (NIH-NCI), Barbara Wells (NIH-NHLBI), and Ying Zhang (IHS). -

Working Paper Series
UNIVERSITY OF MINNESOTA RURAL HEALTH RESEARCH CENTER – WORKING PAPER 36 Access to Rural Pharmacy Services In Minnesota, North Dakota, and South Dakota Working Paper Series Michelle M. Casey, M.S. Jill Klingner, R.N., M.S. Ira Moscovice, Ph.D. Rural Health Research Center Division of Health Services Research and Policy School of Public Health University of Minnesota July 2001 Working Paper #36 Support for this paper was provided by the Office of Rural Health Policy, Health Resources and Services Administration, PHS Grant No. CSRUC 0002-04. UNIVERSITY OF MINNESOTA RURAL HEALTH RESEARCH CENTER – WORKING PAPER 36 Acknowledgements Many individuals and organizations provided valuable input to this study. The members of the Rural Pharmacy Advisory Committee: Ray Christensen, M.D., Moose Lake, Minnesota; Mary Klimp, MHA, International Falls, Minnesota; Mark Malzar, RPh, Turtle Lake, North Dakota; Ann Nopens, RPh, Lake Preston, South Dakota, and Marv Thelen, RPh, Mahnomen, Minnesota, were very helpful identifying rural pharmacy practice issues. The study could not have been conducted without the cooperation of the many rural pharmacists who respond to the pharmacy survey, and the clinic nurses, public health nurses, and social services providers who participated in interviews about access to pharmacy services. Jeffrey Stensland, University of Minnesota Rural Health Research Center, provided computer programming assistance. David Holmstrom, Executive Director, Minnesota Board of Pharmacy; Howard Anderson, Jr., Executive Director, North Dakota Board -

VA Office of Rural Health Telehealth Fact Sheet
OFFICE OF RURAL Telehealth VHA HEALTH INFO SHEET Provider shortages, long distances to health care facilities and limited transportation options often keep rural Veterans from obtaining timely, quality care. To overcome these access challenges, the Department of Veterans Affairs (VA) Office of Rural Health (ORH) uses telehealth technology to help the nearly 3 million rural Veterans enrolled in the VA health care system access clinical services from their home or nearby medical facilities. In fiscal year (FY) 2018, ORH: Enabled telehealth care Funded more than Dedicated $120 million for more than 291,000 20 virtual programs to telehealth programs rural Veterans As the largest provider of telehealth services in the country, VA is leading the nation in telemedicine advancement. In FY 2018, 13% of Veterans who received care from VA did so via telehealth1. Expanding Telehealth Access Telehealth technology helps VA improve rural Veterans’ health and well-being by connecting rural communities with qualified clinicians. VA continues to work to expand telehealth access through the ‘Anywhere to Anywhere’ initiative, a new federal rule that allows VA doctors, nurses and other health care providers to administer care to Veterans using telehealth technology regardless of where they live. As part of its commitment to this initiative, ORH works closely with the Office of Connected Care, which oversees the three modalities of telehealth to provide Officerural Veterans with care regardless of of their location.Rural Health U.S. Department of Veterans Affairs Revised: March 2019 Veterans Health Administration Office of Rural Health Learn more about ORH at www.ruralhealth.va.gov INFO SHEET These three modalities help improve convenience to rural Veterans by providing access to care from their ORH-Funded Telehealth Enterprise-Wide homes or local communities: Initiatives } Synchronous, Real-time or Clinical Video } Clinical Resource } Technology-based Telehealth connects patients and clinicians in real Hubs Eye Care Services time via a communications link. -

Innovative Approaches
INNOVATIVE APPROACHES PREPOSITIONING OBSTETRIC KITS A Strategy for Reducing Maternal and Neonatal Mortality in Health Facilities in the Northern Region of Cameroon CAMEROON PARTNERS: Ministry of Health, UNFPA, SIDA , C2D (The Partnership Framework with France), H4+ Partners JUSTIFICATION OF THE INNOVATION The burden of maternal deaths is of great concern in Cameroon. Among various causes, is the fact that before 2011, in all health facilities including those in the northern region of P H Cameroon, pregnant women were expected to O T pay in advance for care related to delivery and O BY S. TORFINN management of obstetric complications. This prevented access to care for poor women or caused significant delays in the decision to use health facilities, thus leading to an increase in maternal and neonatal mortality in the poorest areas in Cameroon. To address this issue, the Ministry of Health and partners introduced an innovative approach in the northern region of Cameroon, the prepositioning of obstetric kits (birthing kit and emergency caesarean bag) in health facilities. These kits have general use items and medicines for normal vaginal delivery and caesarean delivery respectively. The strategy aims to reduce maternal and neonatal mortality by reducing the third delay (time lost between reaching the facility and initiation of treatment) to access care, especially delayed treatment of obstetric complications and deliveries in these facilities. 1 CAMEROON VE I BACKGROUND INNOVAT APPORACHES Maternal mortality continues to rise in Cameroon, with data reporting an increase of 352 maternal deaths per 100,000 live births from 1998 to 2011 with 430 deaths per 100,000 live births (DHS II, 1998) to 669 maternal deaths per 100,000 live births (DHS III, 2004) then 782 deaths per 100,000 live births (DHS IV, 2011). -

Understanding Rural Health
Rural Health Systems: Understanding Rural Health Medical Laboratory Science 515 Lecture 7 February 15, 2019 • Established in 1980, at The University of North Dakota (UND) School of Medicine and Health Sciences in Grand Forks, ND • One of the country’s most experienced state rural health offices • UND Center of Excellence in Research, Scholarship, and Creative Activity • Home to seven national programs • Recipient of the UND Award for Departmental Excellence in Research Focus on – Educating and Informing – Policy – Research and Evaluation – Working with Communities – American Indians – Health Workforce – Hospitals and Facilities ruralhealth.und.edu 2 1 What is Rural Health • Rural health focuses on population health and improving health status o “Health outcomes of a group of individuals, including the distribution of such outcomes within the group” Dr. David Kindig, What is Population Health? o Rely on social determinants of health and their impact on the population (Health care system, Health Behaviors, Socio-Economic factors, Physical Environment) – “drivers” of health policy (Better Health, Better Care, and Lowered Cost – Three Aims) • Historically, rural health has focused more on infrastructure: facilities, providers, services, and programs available to the public (all with quality, access, and cost implications) – In the ACA world more emphasis on population health, but infrastructure is still critical as it is the pathway to achieve better population health. o HRSA (ORHP, SORH, Flex, NHSC) – Federal bureaucracy orientation o Infrastructure -

Republique Du Cameroun Republic of Cameroon Details Des Projets Par Region, Departement, Chapitre, Programme Et Action Extreme N
REPUBLIQUE DU CAMEROUN REPUBLIC OF CAMEROON PAIX - TRAVAIL - PATRIE PEACE - WORK - FATHERLAND DETAILS DES PROJETS PAR REGION, DEPARTEMENT, CHAPITRE, PROGRAMME ET ACTION OPERATIONS BOOK PER REGION, DIVISION, HEAD, PROGRAMME AND ACTION Exercice/ Financial year : 2017 Région EXTREME NORD Region FAR NORTH Département DIAMARE Division En Milliers de FCFA In Thousand CFAF Année de Tâches démarrage Localité Montant AE Montant CP Tasks Starting Year Locality Montant AE Montant CP Chapitre/Head MINISTERE DE L'ADMINISTRATION TERRITORIALE ET DE LA DECENTRALISATION 07 MINISTRY OF TERRITORIAL ADMINISTRATION AND DECENTRALIZATION PETTE : Reprogrammation des travaux de construction de la sous-préfecture (Phase 1) PETTE 50 000 50 000 2 017 PETTE : Reprogramming of the construction of the Sub-Divisional Office MAROUA: Règlement de la maîtrise d'œuvre pour la construction résidence Préfet MAROUA 5 350 5 350 MAROUA: Payment of the project management of the construction of the residence of 2 017 the SDO MAROUA: Règlement des travaux de la première phase de construction résidence Préfet MAROUA 80 000 80 000 2 017 MAROUA: Payment of the construction of the residence of the SDO Total Chapitre/Head MINATD 135 350 135 350 Chapitre/Head MINISTERE DE LA JUSTICE 08 MINISTRY OF JUSTICE Cour d'Appel de l'Extrême-Nord : Etudes architecturales et géotechniques pour la MAROUA I 40 000 5 000 construction 2 017 Architectural and geotchnical construction studies of the Court of Appeal of Far-North Total Chapitre/Head MINJUSTICE 40 000 5 000 Chapitre/Head MINISTERE DES MARCHES -

Cameroon |Far North Region |Displacement Report Round 15 | 03– 15 September 2018
Cameroon |Far North Region |Displacement Report Round 15 | 03– 15 September 2018 Cameroon | Far North Region | Displacement Report | Round 15 | 03– 15 September 2018 The opinions expressed in the report are those of the authors and do not necessarily reflect the views of the International Organization for Migration (IOM). The designations employed and the presentation of material throughout the report do not imply the expression of any opinion whatsoever on the part of IOM concerning the legal status of any country, territory, city or area, or of its authorities, or concerning its frontiers or boundaries1. IOM is committed to the principle that humane and orderly migration benefits migrants and society. As an intergovernmental organization, IOM acts with its partners in the international community to assist in meeting the operational challenges of migration, advance understanding of migration issues, encourage social and economic development through migration and uphold the human dignity and well-being of migrants. International Organization for Migration Cameroon Mission Maroua Sub-Office UN House Comice Maroua Far North Region Cameroon Tel.: +237 222 20 32 78 E-mail: [email protected] Websites: https://ww.iom.int/fr/countries/cameroun and https://displacement.iom.int/cameroon All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form or by any means, electronic, mechanical, photocopying, recording or otherwise without the prior written permission of the publisher. 1The maps included in this report are illustrative. The representations and the use of borders and geographic names may include errors and do not imply judgment on legal status of territories nor acknowledgement of borders by the Organization. -

Rapport De Situation N° 15 Épidémie De Cholera Dans La Région De L’Extrême-Nord Cameroun - 18 Septembre 2019
RAPPORT DE SITUATION N° 15 ÉPIDÉMIE DE CHOLERA DANS LA RÉGION DE L’EXTRÊME-NORD CAMEROUN - 18 SEPTEMBRE 2019 - Réunion du comité Régional de lutte contre le choléra présidé par le Sensibilisation contre le choléra à Boboyo par l’équipe CERPLE, ECD Gouverneur de la Région de l’Extrême-Nord, 12/09/2019 Kaélé et AAEDC/Unicef, Région de l’Extrême-Nord, 08/09/2019 I. FAITS SAILLANTS • 12/09/2019 : Deuxième réunion du comité Régional de Lutte contre la Choléra présidée par le Gouverneur de la région de l’Extrême-Nord ; • 16/09/2019 : 01 nouveau décès hospitalier enregistré dans le district de santé Kaélé, aire de santé Kaélé ; • 3 nouveaux cas notifiés à Zouayé (DS Karhay) après 26 jours de notification zéro ; • À ce jour : o 243 cas suspects enregistrés dans les districts de santé Kaélé, Kar Hay, Moutourwa, Maroua 1 et Guidiguis ; o 08/18 échantillons confirmés par le laboratoire de la CNPS de Maroua ; o 11 décès (dont 04 en communauté et 07 hospitaliers) enregistrés dans les aires de santé Midjivin, Gané, Mindjil et Boboyo ; o Taux de létalité : 4,5%. 1 II. SITUATION ÉPIDÉMIOLOGIQUE Cas Décès 10 8 6 4 Nombre de cas 2 0 7/5/2019 8/4/2019 8/9/2019 9/3/2019 9/8/2019 6/25/2019 6/30/2019 7/10/2019 7/15/2019 7/20/2019 7/25/2019 7/30/2019 8/14/2019 8/19/2019 8/24/2019 8/29/2019 9/13/2019 9/18/2019 Date de début des symptômes Figure 1 : Courbe épidémique des cas suspects et des décès de choléra dans la Région de l’Extrême-Nord, 18/09/2019 Tableau 1 : Résumé de la situation épidémiologique au 18/09/2019 DS DS Binder DS DS Kaélé DS Kar Hay DS Moutourwa