Triage During a MCI: a Collaborative Process
Total Page:16
File Type:pdf, Size:1020Kb
Load more
Recommended publications
-

Emergency Medical Services Program Policies – Procedures – Protocols
Emergency Medical Services Program Policies – Procedures – Protocols Protocols Table of Contents GENERAL PROVISIONS ................................................................................................ 3 DESTINATION DECISION SUMMARY-METRO BAKERSFIELD AREA ........................ 5 DETERMINATION OF DEATH ..................................................................................... 12 101 AIRWAY OBSTRUCTION ...................................................................................... 16 102 ALTERED LEVEL OF CONSCIOUSNESS ............................................................ 18 103 ALLERGIC REACTION/ANAPHYLAXIS ................................................................ 20 104 ASYSTOLE/ PULSELESS ELECTRICAL ACTIVITY ............................................. 22 105 BITES STINGS ENVENOMATION ......................................................................... 24 106 BRADYCARDIA ..................................................................................................... 26 107 BRIEF RESOLVED UNEXPLAINED EVENT ......................................................... 29 108 BURNS ................................................................................................................... 32 109 CHEMPACK ........................................................................................................... 35 110 CHEST PAIN OR ACUTE CORONARY SYNDROME ........................................... 37 111 CHEST TRAUMA .................................................................................................. -

Mass/Multiple Casualty Triage
9.1 MASS/MULTIPLE CASUALTY TRIAGE PURPOSE · The goal of the mass/multiple Casualty Triage protocol is to prepare for a unified, coordinated, and immediate EMS mutual aid response by prehospital and hospital agencies to effectively expedite the emergency management of the victims of any type of Mass Casualty Incident (MCI). · Successful management of any MCI depends upon the effective cooperation, organization, and planning among health care professionals, hospital administrators and out-of-hospital EMS agencies, state and local government representatives, and individuals and/or organizations associated with disaster-related support agencies. · Adoption of Model Uniform Core Criteria (MUCC). DEFINITIONS Multiple Casualty Situations · The number of patients and the severity of the injuries do not exceed the ability of the provider to render care. Patients with life-threatening injuries are treated first. Mass Casualty Incidents · The number of patients and the severity of the injuries exceed the capability of the provider, and patients sustaining major injuries who have the greatest chance of survival with the least expenditure of time, equipment, supplies, and personnel are managed first. H a z GENERAL CONSIDERATIONS m Initial assessment to include the following: a t · Location of incident. & · Type of incident. M · Any hazards. C · Approximate number of victims. I · Type of assistance required. 9 . 1 COMMUNICATION · Within the scope of a Mass Casualty Incident, the EMS provider may, within the limits of their scope of practice, perform necessary ALS procedures, that under normal circumstances would require a direct physician’s order. · These procedures shall be the minimum necessary to prevent the loss of life or the critical deterioration of a patient’s condition. -

Guidelines for Trauma Team Activation (TTA)
Guidelines for Trauma Team Activation (TTA) ONE of the following criteria must be present with associated traumatic mechanism L e v e Measure Vital Signs and level of consciousness l Trauma Team Activation ALL TTA 1 & 2's MUST BE TRANSPORTED TO RGH Rural Travel time greater than 1 hour, failed airway · Glasgow Coma Scale less than 13 or immediate life threat divert to local facility and · Systolic Blood Pressure less than 90mmHg arrange STAT transport to RGH Trauma Center · Respiratory Rate less than 10 or greater then 29 breaths Prehospital per minute (less than 20 in infant), or advanced airway · Assess patient and determine TTA Level 1 support required · Early activation to receiving facility with: TTA Level, MIVT Report, ETA · STARS Activation or ALS (ACP) intercept NO · Update facility as needed Yes · Transport to Trauma Center Assess anatomy of injury Triage Nurse · Alert TTL Physician with TTA level, MIVT Report, ETA · TTL has a 20min response time · All penetrating injuries to head, neck, torso, and · Alert switchboard to overhead page: extremities proximal to elbow or knee Trauma Level ‘#’ ETA · Chest wall instability or deformity (e.g. flail chest) Trauma Team Lead · Two or more proximal long-bone fractures · Update ER on incoming Rural Trauma patients · Crushed, degloved, mangled, pulseless or amputation · Assume lead role and MRP status of an extremity proximal to wrist or ankle · Prepare resuscitation team · Pelvic fractures (high impact) · Assess, Treat and Stabilize patient 2 · Major facial or head trauma including depressed/open -

MASS CASUALTY TRAUMA TRIAGE PARADIGMS and PITFALLS July 2019
1 Mass Casualty Trauma Triage - Paradigms and Pitfalls EXECUTIVE SUMMARY Emergency medical services (EMS) providers arrive on the scene of a mass casualty incident (MCI) and implement triage, moving green patients to a single area and grouping red and yellow patients using triage tape or tags. Patients are then transported to local hospitals according to their priority group. Tagged patients arrive at the hospital and are assessed and treated according to their priority. Though this triage process may not exactly describe your agency’s system, this traditional approach to MCIs is the model that has been used to train American EMS As a nation, we’ve got a lot providers for decades. Unfortunately—especially in of trailers with backboards mass violence incidents involving patients with time- and colored tape out there critical injuries and ongoing threats to responders and patients—this model may not be feasible and may result and that’s not what the focus in mis-triage and avoidable, outcome-altering delays of mass casualty response is in care. Further, many hospitals have not trained or about anymore. exercised triage or re-triage of exceedingly large numbers of patients, nor practiced a formalized secondary triage Dr. Edward Racht process that prioritizes patients for operative intervention American Medical Response or transfer to other facilities. The focus of this paper is to alert EMS medical directors and EMS systems planners and hospital emergency planners to key differences between “conventional” MCIs and mass violence events when: • the scene is dynamic, • the number of patients far exceeds usual resources; and • usual triage and treatment paradigms may fail. -
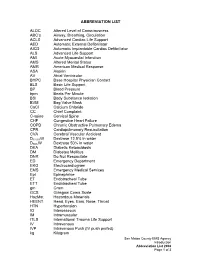
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC's Airway, Breathing, Circulation ACLS Advanced Cardiac Life Suppo
ABBREVIATION LIST ALOC Altered Level of Consciousness ABC’s Airway, Breathing, Circulation ACLS Advanced Cardiac Life Support AED Automatic External Defibrillator AICD Automatic Implantable Cardiac Defibrillator ALS Advanced Life Support AMI Acute Myocardial Infarction AMS Altered Mental Status AMR American Medical Response ASA Aspirin AV Atrial Ventricular BHPC Base Hospital Physician Contact BLS Basic Life Support BP Blood Pressure bpm Beats Per Minute BSI Body Substance Isolation BVM Bag Valve Mask CaCl Calcium Chloride CC Chief Complaint C-spine Cervical Spine CHF Congestive Heart Failure COPD Chronic Obstructive Pulmonary Edema CPR Cardiopulmonary Resuscitation CVA Cerebral Vascular Accident D12.5%W Dextrose 12.5% in water D50%W Dextrose 50% in water DKA Diabetic Ketoacidosis DM Diabetes Mellitus DNR Do Not Resuscitate ED Emergency Department EKG Electrocardiogram EMS Emergency Medical Services Epi Epinephrine ET Endotracheal Tube ETT Endotracheal Tube gm Gram GCS Glasgow Coma Scale HazMat Hazardous Materials HEENT Head, Eyes, Ears, Nose, Throat HTN Hypertension IO Interosseous IM Intramuscular ITLS International Trauma Life Support IV Intravenous IVP Intravenous Push (IV push prefed) kg Kilogram San Mateo County EMS Agency Introduction Abbreviation List 2008 Page 1 of 3 J Joule LOC Loss of Consciousness Max Maximum mcg Microgram meds Medication mEq Milliequivalent min Minute mg Milligram MI Myocardial Infarction mL Milliliter MVC Motor Vehicle Collision NPA Nasopharyngeal Airway NPO Nothing Per Mouth NS Normal Saline NT Nasal Tube NTG Nitroglycerine NS Normal Saline O2 Oxygen OB Obstetrical OD Overdose OPA Oropharyngeal Airway OPQRST Onset, Provoked, Quality, Region and Radiation, Severity, Time OTC Over the Counter PAC Premature Atrial Contraction PALS Pediatric Advanced Life Support PEA Pulseless Electrical Activity PHTLS Prehospital Trauma Life Support PID Pelvic Inflammatory Disease PO By Mouth Pt. -

A Uniform Triage Scale in Emergency Medicine Information Paper
A Uniform Triage Scale in Emergency Medicine Information Paper Triage: sorting, sifting (Webster’s New Collegiate Dictionary) from the French verb trier- “to sort.” Triage has long been considered a simple frontline sorting mechanism in hospital-based emergency departments (EDs). However, evolution in the practice of emergency medicine during the past two decades necessitates a change in how this entry point process is performed and utilized. Many triage systems are in use in the US, but there is no uniform triage scale that would facilitate the development of operational standards in EDs. A nationally standardized triage scale would provide an analytic basis for determining whether the health care system provides safe access to emergency care based on design, resources, and utilization. The performance of EDs could be compared based on case mix and acuity, and expected standards for facilities could be defined. Planners and policy makers would have the tools and the data needed to make rational improvements in the health care delivery system. This paper on triage will acquaint the reader with the history of triage, and provide an overview of the Australian and Canadian systems which are already in use on a national level. The reliability of triage is addressed, and the Canadian and Australian scales are compared. Future implications for a national triage scale are described, along with the goals and benefits of triage development. While there is some controversy about potential liability issues, the many advantages of a national triage scale appear to outweigh any potential disadvantages. History of triage The first medical application of triage occurred on the French battlefield where sorting the victims determined who would be left behind. -

Severe Localized Scapular Pain After a Strenuous Weight-Lifting Session
CASE REPORT Severe localized scapular Editor’s key points With the rising popularity of ultra- pain after a strenuous distance endurance events, strength and conditioning programs, and obstacle course races, exertional weight-lifting session rhabdomyolysis (ER) has become increasingly common in sporting Rosamond E. Lougheed Simpson MD MSc CCFP(SEM) DipSportMed communities. Steven R. Joseph MD MA CCFP(SEM) DipSportMed Lisa Fischer MD CCFP(SEM) FCFP DipSportMed Exertional rhabdomyolysis is often characterized by the classic triad habdomyolysis is a medical condition whereby the intracellular con- of generalized weakness, myalgia, tents from damaged skeletal muscle tissues are released into the blood, and myoglobinuria; however, it is critical to recognize that many cases causing myriad clinical symptoms and outcomes. These can range will not present with all 3 of these Rfrom muscle pain to compartment syndrome, end-organ failure, and death.1-3 criteria. For the male patient in this While the triggers of rhabdomyolysis are numerous, physical exertion as a report, severe myalgia was his only presenting symptom from the triad. causal factor has been receiving increasing media attention recently.4-7 The incidence of exertional rhabdomyolysis (ER) has been challenging The ability to recognize ER, stratify 8 patients into low- and high-risk to estimate, as many cases are likely underrecognized. Current incidence categories, and understand how estimates range from 22.2 to 29.9 per 100 000 patients a year.9,10 As ultra- risk affects patients’ return to play distance endurance events, strength and conditioning programs (eg, CrossFit), can help family physicians make treatment, referral, and return- and obstacle course races have become wildly popular with the superfit to-play decisions with increased and weekend warriors alike, ER is being increasingly recognized as common confidence. -

Redefining the Trauma Triage Matrix
journalofsurgicalresearch july 2020 (251) 195e201 Available online at www.sciencedirect.com ScienceDirect journal homepage: www.JournalofSurgicalResearch.com Redefining the Trauma Triage Matrix: The Role of Emergent Interventions Rachel S. Morris, MD,a,* Nicholas J. Davis, MD,b Amy Koestner, MSN,c Lena M. Napolitano, MD,d Mark R. Hemmila, MD,d and Christopher J. Tignanelli, MDa,b,e a Department of Surgery, University of Minnesota, Minneapolis, Minnesota b Department of Surgery, North Memorial Medical Center, Robbinsdale, Minnesota c Department of Surgery, Spectrum Health - Butterworth Hospital, Grand Rapids, Michigan d Department of Surgery, University of Michigan, Ann Arbor, Michigan e Institute for Health Informatics, University of Minnesota, Minneapolis, Minnesota article info abstract Article history: Background: A tiered trauma team activation (TTA) system aims to allocate resources pro- Received 10 July 2019 portional to the patient’s need based upon injury burden. The current metrics used to Received in revised form evaluate appropriateness of TTA are the trauma triage matrix (TTM), need for trauma 22 October 2019 intervention (NFTI), and secondary triage assessment tool (STAT). Accepted 2 November 2019 Materials and methods: In this retrospective study, we compared the effectiveness of the Available online xxx need for an emergent intervention within 6 h (NEI-6) with existing definitions. Data from the Michigan Trauma Quality Improvement Program was utilized. The dataset contains Keywords: information from 31 level 1 and 2 trauma centers from 2011 to 2017. Inclusion criteria were: Activation adult patients (16 y) and ISS 5. Trauma Results: 73,818 patients were included in the study. Thirty percentage of trauma patients Triage met criteria for STAT, 21% for NFTI, 20% for TTM, and 13% for NEI-6. -

FIRST AID QUICK SHEET- Airway and Breathing
FIRST AID QUICK SHEET Airway and Breathing After you have checked to make sure the scene is safe and put on gloves to protect yourself (Danger) and checked if the patient is responsive (Response), if you find the patient is not responding, you should think: ABC. First check for an Airway and Breathing. Instructions for the A and B steps of the DR. ABC acronym for first aid priorities are below: How to Adjust Someone’s Airway (A): 1. Gently swipe the mouth with one finger to ensure that no objects are blocking the airway. 2. Place two fingers under the casualties chin and one hand on the forehead. 3. Gently lift the chin with two fingers, removing the tongue from the back of the throat. 4. If transport is delayed, roll the casualty onto their side in the recovery position to allow fluids to drain from the mouth Note: If someone is able to speak, their airway is open. Breathing (B): 1. Always remember to look, listen, and feel when checking for breathing. 2. LOOK to see the chest rise and fall. 3. LISTEN to hear breath sounds. 4. Place one hand on the stomach and FEEL for breathing movement and FEEL beneath the nose for air movement. After you have secured an airway and checked for breathing, you may move on to check for bleeding in the C (circulation) step of DR. ABC. *Please be safe and practice first aid at your own risk. LFR International is not liable for injuries resulting from any first aid attempts. . -

Mass Casualty Incident (MCI) Response Module 1
Mass Casualty Incident (MCI) Response Module 1 (Hamilton County Fire Chief's Association, 2013) 1 Objectives Purpose: This module will educate staff on mass casualty triage incident response, including how to: • Define mass casualty triage • Determine considerations for adults and pediatrics • Understand the importance of a patient tracking system • Recognize and implement the patient admission/ discharge MCI triage process • Determine how to appropriately handle the deceased in a large-scale MCI • Recognize the range of incidents that may cause MCIs 2 MCI Basics 3 What is an MCI? • A mass casualty incident (MCI) is an incident where the number of patients exceeds the amount of healthcare resources available. • This number varies widely across the country, but is typically greater than 10 patients. 4 Types of MCI Notifications • During a large scale incident such as a mass casualty, it is important to have a mass notification system. Successful mass notification systems will: . Internally: alert staff to activate MCI protocols and prepare for a potential surge of patients . Externally: increase community awareness 5 Assisting in MCI Response Considerations for hospital staff in an MCI: • Some patients may arrive to the hospital without having been assessed/ triaged at the scene • MCI response requires efficiency and coordination • Non-clinical personnel (including hospital volunteers) can assist in moving patients to designated areas based on level of care • Help gather patient information in the emergency treatment area • Staff should review patients in clinical assignment for any potential discharges/ transfers to make room for potential MCI admissions, a process known as “surge discharge” (Chung S, 2019) 6 Triage Basics Definition of MCI Triage Triage means “to sort.” Triage in an MCI is the assignment of resources based on the initial patient assessment and consideration of available resources. -
Basic Trauma Overview - ABC
Basic Trauma Overview - ABC Dale Dangleben, MD, FACS 1 2 Team 3 Extended Team 4 Team Leader Decrease chaos / optimize care. – Remains calm – Maintains control and provides direction – Stays decisive – Sees the big picture (situational awareness) – Is open to other team members input – Directs resuscitation – Makes early decision to transfer the patients that exceed the local capabilities 5 Team Members − Know your roles in the trauma team − Remain calm − Be responsive to team leader −Voice suggestions or concerns 6 Responsibilities – Perform the Primary and secondary survey – Verbalize patient care – Report completed tasks 7 Responsibilities – Monitors the patient – Manual BP – Obtains IV access – Administers medications – Dresses wounds – Performs or assists in resuscitative procedures 8 Responsibilities Records data Ensures documentation accompanies patient upon transfer Assists team members as needed 9 Responsibilities – Obtains needed supplies – Coordinates communication with local and external resources – Assists team members as needed 10 Responsibilities • Place Oxygen on patient • Manage airway • Hold C spine • Manage ventilator if • Manage rapid infuser line patient intubated where indicated • Assists team members as needed 11 Organization of trauma resuscitation area – Basic adult and pediatric equipment for: • Airway management (cart) • IV access with warm fluids • Chest tube insertion • Hemorrhage control (tourniquets, pelvic binders) • Immobilization • Medications • Pediatric length/weight based tape (Broselow Tape) – Warming -

Abdominal Pain 02/02/2021
Medical Control Board Approved Protocols ABDOMINAL PAIN 02/02/2021 Follow Assessment, General Procedures Protocol EMR • Assess and support ABCs • Position of comfort • Supine if: • Trauma • Hypotension • Syncope • NPO • Monitor vital signs • Oxygen indicated for: • Unstable vitals • Severity of pain • Suspected GI bleed EMT • 12-lead – See CARDIAC-ECG/12 Lead Procedure A-EMT • IV – NS with standard tubing • Titrate fluid to patient’s needs – See Shock Protocol EMT-I/ • Cardiac monitoring PARAMEDIC • Pain management – See Acute Pain Management Protocol 199 March, 2021 Medical Control Board Approved Protocols This page intentionally left blank 200 March, 2021 Medical Control Board Approved Protocols ACUTE ADRENAL INSUFFICIENCY PROTOCOL 02/02/2021 Follow Assessment, General Procedures Protocol • Acute adrenal insufficiency (crisis) can occur in the following settings: - During neonatal period (undiagnosed adrenal insufficiency) - In patients with known, pre-existing adrenal insufficiency (e.g., Addison’s disease) - In patients who are chronically steroid dependent (i.e., taking steroids daily, long- term, for any number of medical conditions) - Adrenal crisis can be triggered by any acute stressor (e.g., trauma or illness), as well as by abrupt cessation of steroid use (for any reason). • Signs/symptoms of adrenal crisis: Altered mental status, seizures; generalized weakness, hypotension, hypoglycemia, hyperkalemia. • Notify hospital you are transporting known/suspected adrenal crisis patient • Emergency transport for: ALOC, hypotension, hypoglycemia, suspected hyperkalemia. Acute adrenal crisis is an immediately life-threatening emergency, and must be treated aggressively EMR • PMH, Take thorough history of patient’s steroid use/dependence. Determine if the patient is on oral hydrocortisone. • Assess and support ABC’s • Oxygen therapy, as needed • Monitor vitals EMT • Check blood glucose • If blood glucose is <60: administer glucose solution orally if the patient is awake and able to protect own airway • Obtain 12 lead ECG; if time permitted.